Mini Review - Interventional Cardiology (2022)
Clinical benefits of Minimally Invasive Coronary Artery Bypass Grafting (MICS CABG)
- Corresponding Author:
- Keita Kikuchi
Department of Cardiovascular Surgery,
Tokyo Bay Urayasu Ichikawa Medical Center,
Chiba,
Japan,
E-mail: kikuchicvs@outlook.com
Received date: 16-Dec-2022, Manuscript No. FMIC-22-83726; Editor assigned: 19-Dec-2022, PreQC No. FMIC-22-83726 (PQ); Reviewed date: 02-Jan-2023, QC No. FMIC-22-83726; Revised date: 09-Jan-2023, Manuscript No. FMIC-22-83726 (R); Published date: 19-Jan-2023, DOI: 10.37532/1755-5310.2023.14 (S14). 339
Abstract
The advantage of Coronary Artery Bypass Grafting (CABG) is that it provides a good long-term prognosis. In particular, excellent long-term outcomes can be expected with the use of multiple arterial grafts such as BITA (bilateral internal thoracic artery) and radial artery. Due to the invasiveness of a sternotomy in CABG surgery, it tends to be shunned by patients who want a short recovery period and an early return to work. Taking all of these into consideration, Minimally Invasive Coronary Artery Bypass Grafting (MICS CABG) has come to the fore in recent years. MICS CABG was introduced in 2009 and it allows graft deployment to all coronary territories. We are currently proactive in performing MICS CABG using multiple arterial grafts such as BITA, Radial Artery (RA), and Gastroepiploic Artery (GEA). Refinement of techniques in MICS CABG has enabled less invasive surgery that preserves the sternum but makes it possible to do graft configurations comparable with conventional CABG. We would like to introduce advanced MICS CABG as a new standard in surgical coronary revascularization.
Keywords
Minimally invasive coronary artery bypass grafting • Bilateral internal thoracic artery • Hybrid coronary revascularization • Harmonic scalpel
Introduction
In recent years, Minimally Invasive Coronary Artery Bypass Grafting (MICS CABG), which preserves the sternum and performs multi-vessel bypass through a left small thoracotomy, has attracted attention [1]. I will discuss how treatment for ischemic heart disease will change with MICS CABG and its future prospects based on our clinical experience.
Aorto-coronary bypass to MICS CABG
The first surgical coronary revascularization was performed by Kolesov in 1964 [2], and Favolaro, et al. first performed Aorto-Coronary artery bypass grafting in 1967 [3]. In 1986, Loop, et al. reported the favorable clinical results of Internal Thoracic Artery (ITA) usage in surgical revascularization [4]. Since then it has evolved into the conventional Coronary Artery Bypass Grafting (CABG) that we know today, which uses ITA and Saphenous Vein Graft (SVG), performed under Cardiopulmonary Bypass (CPB) with an arrested heart.
In 1996, Calafiore, et al. reported direct anastomosis of the Left Internal Thoracic Artery (LITA) and the Left Anterior Descending artery (LAD) through a small left anterolateral incision (MIDCAB: Minimally Invasive Direct Coronary Artery Bypass) [5]. The minimally invasive approach to CABG was born. Thereafter, with the evolution of suction-type stabilizers, Off-Pump CABG (OPCAB) which performs multi-vessel bypass without the use of cardiopulmonary bypass has become popular as a less invasive form of CABG [6-8]. In 2009, McGinn, et al. reported on Minimally Invasive Coronary Artery Bypass Grafting (MICS CABG) [9], opening the door to a new era of minimally invasive CABG.
What Is MICS CABG?
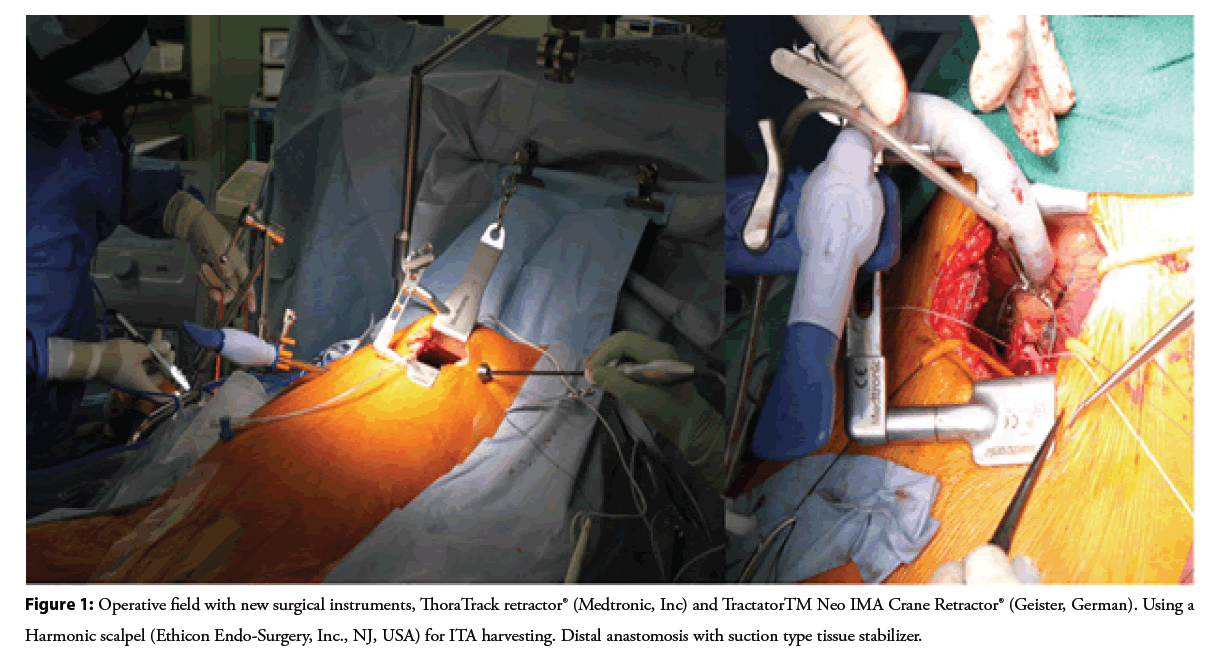
MICS CABG is surgical coronary revascularization done through a small left antero-lateral thoracotomy with or without CPB. The excellent operative field made possible by the new surgical instruments shown in the Figure 1, allows graft anastomosis to the ascending aorta and graft deployment to all coronary arteries [9]. Since MICS CABG does not violate the sternum, Deep Sternal Wound Infection (DSWI) will never be an issue even in severely diabetic patients. It is also expected that perioperative blood transfusions will be reduced. The minimally invasive approach will allow earlier discharge from the hospital and faster recovery after surgery [9-11]. Good results have also been reported in elderly patients [12]. MICS CABG can yield favorable long-term outcomes [13]. Initially LITA and SVG were the only conduits used in MICS CABG [9], but in 2014, the use of BITA Y-composite graft in MICS CABG was reported [14]. We reported the use of BITA in MICS CABG as an in-situ graft in 2015 [15]. Since then, many institutions have reported the use of BITA in MICS CABG [16-20]. We started doing MICS CABG since within 2012 and started using BITA in 2014 [15,16]. We are currently proactive in performing MICS CABG using multiple arterial grafts such as BITA, Radial Artery (RA), and right Gastroepiploic Artery (rGEA). Refinement of techniques in MICS CABG has enabled less invasive surgery that preserves the sternum but makes it possible to do graft configurations comparable with conventional CABG [20].
MICS CABG in our group
A review of MICS CABG based on the clinical results of our group was reported in 2022 [20].
Strategy and indication of MICS CABG
We currently aim to perform MICS CABG that preserves the sternum, does not use the cardiopulmonary bypass, and with minimal manipulation of the ascending aorta. We perform MICS CABG with these three main principles in mind.
Our indications for MICS CABG are shown in Table 1. Currently, we believe that MICS CABG is feasible in many cases. On the other hand, MICS CABG is not indicated in emergency cases such as Acute Coronary Syndrome (ACS), low cardiac output and cases with cardiomegaly. Furthermore, MICS CABG is contraindicated for patients with respiratory dysfunction such as severe Chronic Obstructive Pulmonary Disease (COPD) because the operation is performed with one-lung ventilation. MICS CABG is the default approach if there are no contraindications [21].
| Indications for MICS CABG | Contraindication for MICS CABG |
|---|---|
| Severe DM | Small and Severe diffuse TVD |
| High risk for DSWI | Emergent cases with hemodynamic instability |
| Patient desire for early recover to normal activity | Ischemic cardiomyopathy (Poor<40%EF, dilated heart) |
| Elderly patients | Severe COPD |
| Hybrid coronary revascularization | Severe chest wall deformity |
| Cosmetic |
Note: MICS: Minimally Invasive Cardiac Surgery; CABG: Coronary Artery Bypass Graft; DM: Diabetes Mellitus; TVD: Triple Vessel Disease; COPD: Chronic Obstructive Pulmonary Disease
Table 1: Indications and contra-indications of MICS CABG.
| Target coronary | No | ln situ ITA (n=393) | Free ITA (n=31) | RA (n=39) | GEA (n=26) | SVG (n = 223) | ||
|---|---|---|---|---|---|---|---|---|
| LITA (n=293) | RITA (n=100) | LITA (n=6) | RITA (n=25) | |||||
| Individual/composite | Individual/composite | Individual/composite | Individual/composite | Individual/composite | Individual/composite | Individual/composite | ||
| LAD | 242 | 166/2 | 65/1 | 1/1 | 0/2 | 2/0 | 0/0 | 1/2 |
| Diagonal | 64 | 23/3 | 5/2 | 0/1 | 0/4 | 0/0 | 0/0 | 23/2 |
| OM | 109 | 28/10 | 3/9 | 0/1 | 0/10 | 0/12 | 0/0 | 29/7 |
| PL | 138 | 42/8 | 1/8 | 0/2 | 0/6 | 1/6 | 0/5 | 51/8 |
| PDA | 159 | 0/11 | 1/5 | 0/1 | 0/3 | 6/12 | 18/3 | 91/9 |
| Total | 712 | 259/34 | 75/25 | 1/5 | 0/25 | 9/30 | 18/8 | 195/28 |
Note: ITA: Internal Thoracic Artery; LITA: Left Internal Thoracic Artery; RITA: Right Internal Thoracic Artery; RA: Radial Artery; GEA: Gastroepiploic Artery; SVG: Saphenous Vein Graft ; LAD: Left Anterior Descending; OM: Obtuse Marginal Artery; PL: Posterolateral Artery; PDA: Posterior Descending Artery
Table 2: Distribution of conduits and target vessels in MICS CABG.
Surgical Procedure
We have developed this step-by-step approach in doing MICS CABG [22]
• Pre-operative contrast CT scans have been done routinely to assess ascending aorta and ITAs.
• The patient is put on 30 degrees right decubitus position and an 8 cm incision is made on the 5th intercostal space on the left chest wall. ThoraTrack retractor® (Medtronic, Inc) and TractatorTM Neo IMA Crane Retractor® (Geister, German) are used to obtain a good surgical field during surgery.
• Left Internal Thoracic Artery (LITA) is harvested using a harmonic scalpel (Ethicon Endo-Surgery, Inc) via port from inserted in the same intercostal space lateral to the initial incision, and Right Internal Thoracic Artery (RITA) has been harvested since 2014 with the same technique via the same incision and port.
• Proximal anastomosis is done on the ascending aorta using a partial occluding aortic clamp and with a tissue stabilizer used to retract the main pulmonary artery away from the aorta.
• The heart is displaced using a heart positioner or three deep pericardial sutures. Distal anastomoses are performed with usual suction-type tissue stabilizer. We intend to do multiarterial and an-aortic MICS CABG after overcoming the learning curve.
Using BITA and multi-arterial grafts
LITA+SVG grafts have long been used for CABG. Lytle, et al. reported favorable results for CABG using Bilateral Internal Thoracic Arteries (BITA) [23], and many articles have since reported the superiority of BITA [24-26]. However, the use of BITA is low [27], due to the increased risk of DSWI complications [28,29]. In addition, recent reports of good clinical results with RA have highlighted the usefulness of multiple arteries in the ART trial, which was supposed to demonstrate the superiority of BITA [30]. The use of multi-arterial grafts has been reported to improve long-term outcomes in CABG [30,31]. In the 2021 ACC/AHA/SCAI Guideline, RA and ITA use are classified as class I [32], and the use of multiple artery grafts using ITAs and RA is recommended [32,33]. At the beginning of our MICS CABG series, we used LITA+SVG. Then we started using BITA in 2014 [16,17]. Now use BITA as our first choice. We prefer to use the Harmonic scalpel (Ethicon Endo-Surgery, Inc., NJ, USA), an ultrasonic energy device, for ITA harvesting (Figure 1). This allows longer ITAs to be harvested by skeletonization [34]. We also use the RA [35,36], as recommended by the guidelines, and r GEA [37,38]. We actively perform MICS CABG with a total arterial graft strategy [20]. Currently, there are many reports of MICS CABG using BITA [14-17,20] and graft deployment like the ones done in conventional CABG is possible in MICS CABG.
Discussion
Outcomes of MICS CABG
From February 2012 to May 2021, 247 consecutive patients who underwent MICS CABG using an ultrasonically skeletonized internal thoracic artery were reviewed retrospectively.
Multi-vessel bypass grafting was performed in 200 cases, in which triple bypass was the most common. We used BITA in 108 cases (43.4%), RA in 39 cases and r GEA in 26 cases. The total arterial graft strategy was completed in 126 cases (50.6%). Anaortic manner was achieved in 142 cases (57%). The average distal anastomosis was 2.6 and 94 cases (38.1%) underwent 3-vessel bypass, which was the most common. Average operative time was 289 min, CPB was used in 3 cases and there was no conversion to sternotomy. The distal anastomosis was possible for all territories which are shown in Table 2. There was no stroke and no DSWI. SSI was seen in 5 cases. There was one mortality (Table 3).
| Operative characteristics | Postoperative outcomes |
|---|---|
| No. of grafts | |
| 1 grafts | 47 (19.0%) |
| 2 grafts | 60 (24.3%) |
| 3 grafts | 94 (38.1%) |
| 4 grafts | 46 (18.6%) |
| Use of BITA | 108 (43.4%) |
| Sequential bypass | 97 (39.3%) |
| Average distal anastomosis | 2.62 ± 1.1 |
| Aortic no-touch technique | 142 (57.0%) |
| Total arterial revascularization | 126 (50.6%) |
| Use of cardiopulmonary bypass | 3 (1.2%) |
| Conversion to sternotomy | 0 (0%) |
| Hybrid coronary revascularization | 10 (4.0%) |
| Procedure time (min) | 288.6 ± 112.7 |
| In-hospital mortality | 1 (0.4%) |
| Stroke | 0 (0%) |
| Reoperation for bleeding | 7 (2.8%) |
| Perioperative transfusion | 47 (18.9%) |
| Respiratory insufficiency | 4 (1.6%) |
| New-onset atrial fibrillation | 23 (9.3%) |
| New-onset renal failure | 2 (0.8%) |
| Pleural effusion | 39 (15.8%) |
| Surgical site infection | 5 (2.0%) |
| Median days of hospitalization (lQR) | 11.5 (9-15) |
Note: IQR: Interquartile Range
Table 3: Operative characteristics (left) and postoperative outcomes of our study.
Future Prospects of MICS CABG
An-aortic MICS CABG with aggressive use of BITA
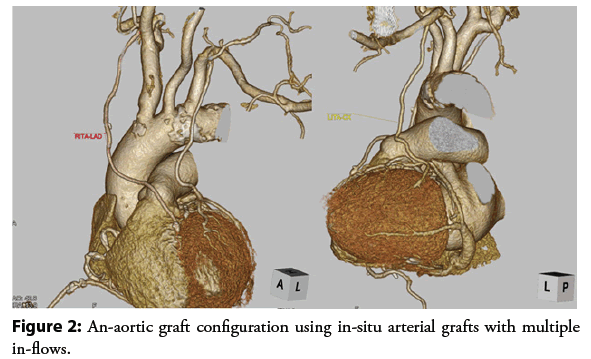
We are aiming for MICS CABG to become the standard surgical coronary revascularization procedure done without the use of CPB or OPCAB via left small thoracotomy. The greatest advantage of OPCAB is the prevention of acute complications [39-41], and an-aortic CABG that does not touch the ascending aorta is recommended to prevent further cerebral complications [42,43]. Therefore, recently we have been aggressively incorporated the principle of an-aortic surgery in our MICS CABG with multiarterial grafting. We believe that securing multiple in-flows by in-situ BITA and rGEA, will provide good blood flow and avoid competitive flow in the grafts.
The aggressive use of arterial grafting with multiple in-flows allows an-aortic graft configuration, which provides comparable outcomes to conventional CABG shown in the Figure 2. It is also important to note that DSWI will not occur in MICS CABG, even in severe diabetic patients with poor glucose control, because it does not cut the sternum. We believe that an-aortic MICS CABG using BITA or multiple arterial grafts will avoid serious complications such as DSWI and cerebral infarction but provide the benefits of a minimally invasive procedure with good long-term outcomes.
MICS CABG and HCR (Hybrid Coronary Revascularization)
Based on the patient’s condition and SYNTAX score [44,45], coronary artery lesions are evaluated, and a treatment policy is determined for each patient according to current guidelines [32,33]. Some coronary lesions may be better off with PCI while some will be better with CABG. The advantage of CABG is not for the LAD alone. If a HCR approach is tailor-made for a specific lesion set, satisfactory results can be obtained for any coronary artery lesion. In recent years, many reports have described HCR, which basically involves robotically assisted LITA harvesting and LITA-LAD anastomosis, followed by the Percutaneous Coronary Intervention (PCI) for other lesions [46-49]. However, lesions favoring CABG are not limited to the LAD.
MICS CABG, which allows multi-vessel bypass with a small wound, is not limited to bypass of the LAD, but also allows HCR to combine multi-vessel MICS CABG with PCI using multiple arterial grafts such as BITA and RA. This new era of HCR is expected to achieve better long-term outcomes because of multi-arterial grafting and proper HCR planning. From now on, the heart team should consider “treatment decisions for each coronary artery” instead of “treatment decisions for each patient”. We believe that HCR tailormade for specific lesion sets, could spark a paradigm shift in the field of coronary revascularization. Of course, HCR should be performed with consideration of the patient’s general condition. There are two types of HCR: HCR using SITA as the minimum requirement and HCR using BITA or arterial grafts to achieve a good long-term prognosis. The heart team should discuss these issues in order to deepen understanding of the benefits of each treatment method. As stated in the guidelines [32]. The role of the Heart Team also exists in coronary revascularization, and its significance is great.
Conclusion
With the development of standard procedures and protocols, MICS CABG has become an established procedure for surgical coronary revascularization. The use of BITA, multiple arterial grafts, and even an-aortic surgery is now possible in MICS CABG. MICS CABG is expected to bring a new treatment option to the heart team as a revolutionary minimally invasive treatment.
References
- Nambala S, Mishra YK, Ruel M. Less invasive multivessel coronary artery bypass grafting: Now is the time. Curr Opin Cardiol. 36(6): 735-739 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Kolessov VI. Mammary artery-coronary artery anastomosis as method of treatment for angina pectoris. J Thorac Cardiovasc Surg. 54(4): 535-544 (1967).
[Google Scholar] [PubMed]
- Favaloro RG. Saphenous vein autograft replacement of severe segmental coronary artery occlusion: Operative techniqueï¼Ann Thorac Surg. 5(4): 334-339 (1968).
[CrossRef] [Google Scholar] [PubMed]
- Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the internal mammary graft on 10-year survival and other cardiac events. New Engl J Med. 314(1): 1-6 (1986).
[CrossRef] [Google Scholar] [PubMed]
- Calafiore AM, Di Giammarco G, Teodori G, et al. Left anterior descending coronary artery grafting via a left anterior small thoracotomy without cardiopulmonary bypass. Ann Thorac Surg. 61(6): 1659-1665 (1996).
[CrossRef] [Google Scholar] [PubMed]
- Diegeler A, Matin M, Falk V, et al. Indication and patient selection in minimally invasive and 'off-pump' coronary artery bypass grafting. Eur J Cardiothorac Surg. 16(S1): 79-82 (1999).
[CrossRef] [Google Scholar] [PubMed]
- Yokoyama T, Baumgartner FJ, Gheissari A, et al. Off-pump versus on-pump coronary bypass in high-risk subgroups. Ann Thorac Surg. 70(5): 1546-1550 (2000).
[CrossRef] [Google Scholar] [PubMed]
- Meharwal ZS, Mishra YK, Kohli V, et al. Off-pump multivessel coronary artery surgery in high-risk patients. Ann Thorac Surg. 74(4): 1353-7 (2002).
[CrossRef] [Google Scholar] [PubMed]
- McGinn JT, Usman S, Lapierre H, et al. Minimally invasive coronary artery bypass grafting: Dual-center experience in 450 consecutive patients. Circulation. 120(S11): 78-84 (2009).
[CrossRef] [Google Scholar] [PubMed]
- Lapierre H, Chan V, Sohmer B, et al. Minimally invasive coronary artery bypass grafting via a small thoracotomy versus off-pump: A case-matched study. Eur J Cardiothorac Surg. 40(4): 804-810 (2011).
[CrossRef] [Google Scholar] [PubMed]
- Rabindranauth P, Burns JG, Vessey TT, et al. Minimally invasive coronary artery bypass grafting is associated with improved clinical outcomes. Innovations (Phila). 9(6): 421-426 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Barsoum EA, Azab B, Shah N, et al. Long-term mortality in minimally invasive compared with sternotomy coronary artery bypass surgery in the geriatric population (75 years and older patients). Eur J Cardiothorac Surg. 47(5): 862-867 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Guo MH, Vo TX, Horsthuis K, et al. Durability of minimally invasive coronary artery bypass grafting. J Am Coll Cardiol. 78(13): 1390-1391 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Nambiar P, Mittal C. Minimally invasive coronary bypass using internal thoracic arteries via a left minithoracotomy: "the Nambiar Technique". Innovations (Phila). 8(6): 420-426 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Kikuchi K, Une D, Endo Y, et al. Minimally invasive coronary artery bypass grating using bilateral in situ internal thoracic arteries. Ann Thorac Surg. 100(3): 1082-1084 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Kikuchi K, Chen X, Mori M, et al. Perioperative outcomes of off-pump minimally invasive coronary artery bypass grafting with bilateral internal thoracic arteries under direct vision. Interact Cardiovasc Thorac Surg. 24(5): 696-701 (2017).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Nambiar P, Kumar S, Mittal CM, et al. Outcomes of bilateral internal thoracic arteries in minimally invasive coronary artery bypass grafting with analogy to the SYNTAX trial. Innovations (Phila). 14(3): 227-235 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Davierwala PM, Verevkin A, Sgouropoulou S, et al. Minimally invasive coronary bypass surgery with bilateral internal thoracic arteries: Early outcomes and angiographic patency. J Thorac Cardiovasc Surg. 162(4): 1109-1119 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Diab M, Färber G, Sponholz C, et al. Coronary artery bypass grafting using bilateral internal thoracic arteries through a left-sided minithoracotomy: A single-center starting experience. Thorac Cardiovasc Surg. 67(6): 437-443 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Tachibana K, Kikuchi K, Narayama K, et al. Minimally invasive coronary artery bypass grafting with ultrasonically skeletonized internal thoracic artery. JTCVS Tech. 14: 107-113 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Kikuchi K, Mori M. Less-invasive coronary artery bypass grafting international landscape and progress. Curr Opin Cardiol. 32(6): 715-721 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Kikuchi K, Mori M. Minimally invasive coronary artery bypass grafting: A systematic review. Asian Cardiovasc Thorac Ann. 25(5): 364-370 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Lytle BW, Blackstone EH, Loop FD, et al. Two internal thoracic artery grafts are better than one. J Thorac Cardiovasc Surg. 117(5): 855-872 (1999).
[CrossRef] [Google Scholar] [PubMed]
- Lytle BW, Blackstone EH, Sabik JF, et al. The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years. Ann Thorac Surg. 78(6): 2005-2014 (2004).
[CrossRef] [Google Scholar] [PubMed]
- Aaron J. Weiss, Shan Zhao, et al. A meta-analysis comparing bilateral internal mammary artery with left internal mammary artery for coronary artery bypass grafting. Ann Cardiothorac Surg. 2(4): 390-400 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Gaudino M, Bakaeen F, Benedetto U, et al. Use Rate and outcome in bilateral internal thoracic artery grafting: Insights from a systematic review and meta-analysis. J Am Heart Assoc. 7(11): e009361 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Iribarne A, Goodney PP, Flores AM, et al. National trends and geographic variation in bilateral internal mammary artery use in the United States. Ann Thorac Surg. 104(6): 1902-1907 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Lazar HL. The risk of mediastinitis and deep sternal wound infections with single and bilateral, pedicled and skeletonized internal thoracic arteries. Ann Cardiothorac Surg. 7(5): 663-672 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Ohira S, Miyata H, Yamazaki S, et al. Deep sternal wound infection after bilateral internal thoracic artery grafting: Insights from a Japanese national database. J Thorac Cardiovasc Surg. 157(1): 166-173 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Taggart DP, Benedetto U, Gerry S, et al. Arterial revascularization trial investigators. Bilateral vs single internal-thoracic-artery grafts at 10 years. N Engl J Med. 380(5): 437-446 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Taggart DP, Audisio K, Gerry S, et al. Single vs multiple arterial grafting in diabetic patients at 10 years: The arterial revascularization trial. Eur Heart J. 43(44): 4644-4652 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: A report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation. 5(3): e18-e114 (2022).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 40(2): 87-165 (2019).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Higami T, Kozawa S, Asada T, et al. Skeletonization and harvest of the internal thoracic artery with an ultrasonic scalpel. Ann Thorac Surg. 70(1): 307-308 (2000).
[CrossRef] [Google Scholar] [PubMed]
- Gaudino M, Benedetto U, Fremes S, et al. Radial-artery or saphenous-vein grafts in coronary-artery bypass surgery. N Engl J Med. 378: 2069-2077 (2018).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Gaudino M, Benedetto U, Fremes S, et al. Association of radial artery graft vs saphenous vein graft with long-term cardiovascular outcomes among patients undergoing coronary artery bypass grafting: A systematic review and meta-analysis. JAMA. 324(2): 179-187 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Suma H, Tanabe H, Takahashi A, et al. Twenty years experience with the gastroepiploic artery graft for CABG. Circulation. 116(S11): 188-191 (2007).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Suzuki T, Asai T, Nota H, et al. Early and long-term patency of in situ skeletonized gastroepiploic artery after off-pump coronary artery bypass graft surgery. Ann Thorac Surg. 96(1): 90-95 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Polomsky M, He X, O'Brien SM, et al. Outcomes of off-pump versus on-pump coronary artery bypass grafting: Impact of preoperative risk. J Thorac Cardiovasc Surg. 145(5):1193-1198 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Kowalewski M, Pawliszak W, Malvindi PG, et al. Off-pump coronary artery bypass grafting improves short-term outcomes in high-risk patients compared with on-pump coronary artery bypass grafting: Meta-analysis. J Thorac Cardiovasc Surg. 151(1) 60-77 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Chawla LS, Zhao Y, Lough FC, et al. Off-pump versus on-pump coronary artery bypass grafting outcomes stratified by preoperative renal function. J Am Soc Nephrol. 23: 1389-1397 (2012).
[CrossRef] [Google Scholar] [PubMed]ã
- Misfeld M, Potger K, Ross DE, et al. "Anaortic" off-pump coronary artery bypass grafting significantly reduces neurological complications compared to off-pump and conventional on-pump surgery with aortic manipulation. Thorac Cardiovasc Surg. 58(7): 408-414 (2010).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Emmert MY, Seifert B, Wilhelm M, et al. Aortic no-touch technique makes the difference in off-pump coronary artery bypass grafting. J Thorac Cardiovasc Surg. 142(6): 1499-1506 (2011).
[CrossRef] [Google Scholar] [PubMed]ã
- Mohr FW, Morice MC, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow- up of the randomised, clinical SYNTAX trial. Lancet. 381(9867): 629-638 (2013).
[CrossRef] [Google Scholar] (All versions) [PubMed]ã
- Farooq V, van Klaveren D, Steyerberg EW, et al. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: Development and validation of SYNTAX score II. Lancet. 381(9867): 639-650 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Kiaii B, Teefy P. Hybrid coronary artery revascularization: A review and current evidence. Innovations (Phila). 14(5): 394-404 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Hage A, Giambruno V, Jones P, et al. Hybrid coronary revascularization vs off-pump coronary artery bypass grafting: Comparative effectiveness analysis with long-term follow-up. J Am Heart Assoc. 8(24): e014204 (2019).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Basman C, Hemli JM, Kim MC, et al. Long-term survival in triple-vessel disease: Hybrid coronary revascularization compared to contemporary revascularization methods. J Card Surg. 35(10): 2710-2718 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Reynolds AC, King N. Hybrid coronary revascularization vs conventional coronary artery bypass grafting. Systematic review and meta-analysis. Medicine (Baltimore). 97(33): e11941 (2018).
[CrossRef] [Google Scholar] [PubMed]