Case Report - Interventional Cardiology (2025)
Case Report on LAD Perforation During CTO-PCI Sealed by Coil Embolization
- Corresponding Author:
- Ayesha Siddika
Department of cardiology, United Hospital Limited, Dhaka, Bangladesh
E-mail:ayeshasiddika835@gmail.com
Received date: 28-Aug-2025, Manuscript No. FMIC-25-170510; Editor assigned: 29-Aug-2025, PreQC No. FMIC-25-170510 (PQ); Reviewed date: 12-Sep-2025, QC No. FMIC-25-170510; Revised date: 19-Sep-2025, Manuscript No. FMIC-25-170510 (R); Published date: 29-Sep-2025, DOI: 10.37532/1755-5310.2025.17(S28).714
Abstract
T he risk of Coronary Artery Perforation (CAP) is high during Percutaneous Coronary Intervention (PCI) for Chronic Total Occlusion (CTO). In cases of large proximal CAP, covered stents are often required. However, when the antegrade wire fails to cross the CTO lesion or enters a false tract, this approach becomes unfeasible. In such situations, coil embolization is a potential option. We present an unusual case of a 57-year-old hypertensive, diabetic man with dyslipidemia who presented with central, compressive chest pain at rest and on exertion, associated with dyspnea. He was eventually diagnosed with chronic stable angina. This case underscores the importance of coronary angiography and timely revascularization in patients at high risk of underdiagnosed coronary artery disease. Furthermore, it highlights the management of serious complications such as coronary perforation. An aggressive treatment strategy combined with prompt diagnosis can be lifesaving.
Keywords
Chronic total occlusion • Coronary artery perforation • Percutaneous coronary intervention
Description
CAP is an uncommon but potentially life-threatening complication of PCI, particularly in procedures involving CTO. While micro perforations are relatively common, generally well tolerated, and often do not require specific management, large perforations (Grade III) are associated with significant morbidity and mortality. The risk of adverse outcomes, including death, is estimated to be around 10% in such cases. Prompt recognition and appropriate management strategies are therefore essential to improve patient outcomes [1-4].
Case presentation
A 57-year-old man was referred to our united hospital with a 6-month history of intermittent compressive chest pain occurring both at rest and on exertion. His symptoms had progressively worsened over the previous 2 months despite receiving optimal medical therapy at the maximum tolerated doses. The patient had a 10 year history of hypertension but no relevant family history of cardiovascular disease. He had been on optimal medical therapy for coronary heart disease.
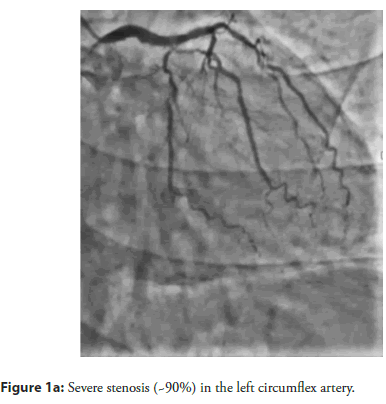
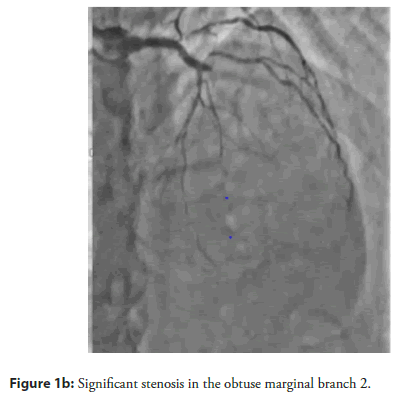
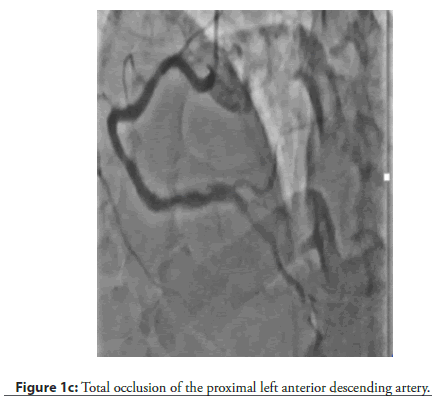
On admission, his blood pressure was 120/80 mmHg, and his heart rate was 72 beats per minute. Electrocardiography (ECG) demonstrated nonspecific ST-T wave changes in leads I, II, III, aVF, and aVL. Laboratory evaluation showed normal cardiac enzyme levels. Transthoracic Echocardiography (TTE) revealed a Left Ventricular Ejection Fraction (LVEF) of 62% without regional wall motion abnormalities. Diagnostic Coronary Angiography (CAG) demonstrated 90% stenosis in the Left Circumflex Artery (LCX) and Obtuse Marginal Branch 2 (OM2), along with total occlusion of the proximal Left Anterior Descending (LAD) artery (Figure 1a–Figure 1c).
Figure 1a: Severe stenosis (~90%) in the left circumflex artery.
Figure 1b: Significant stenosis in the obtuse marginal branch 2.
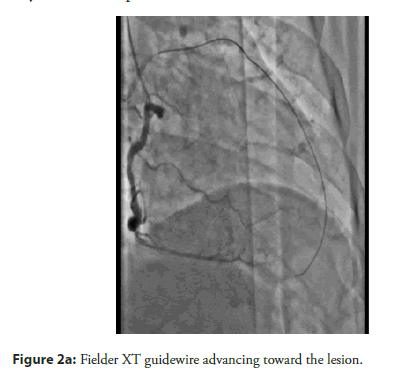
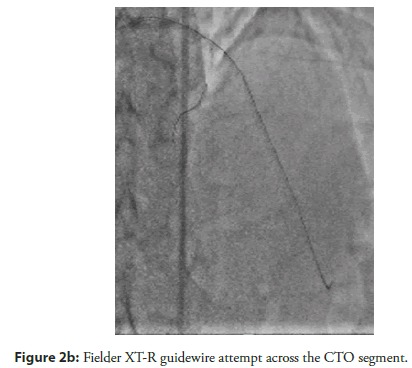
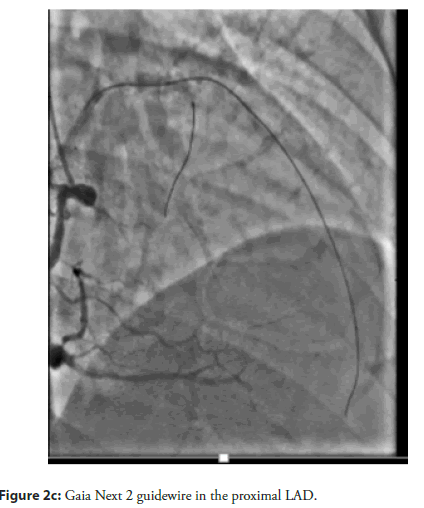
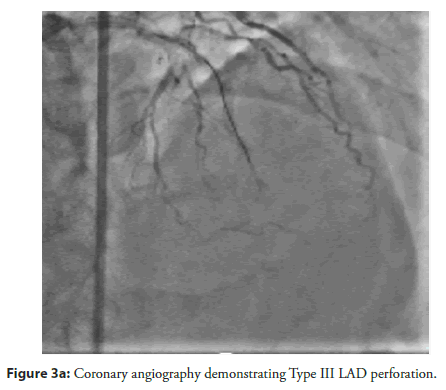
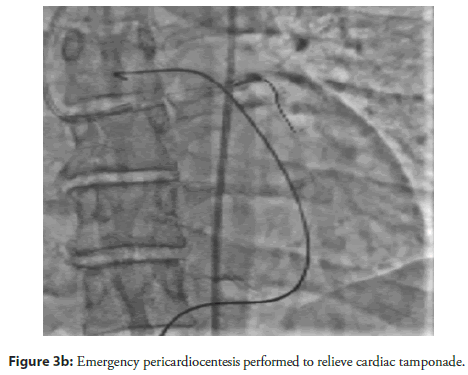
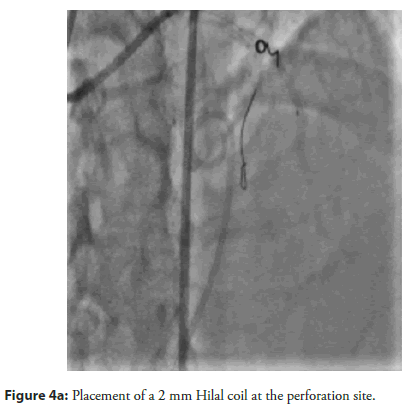
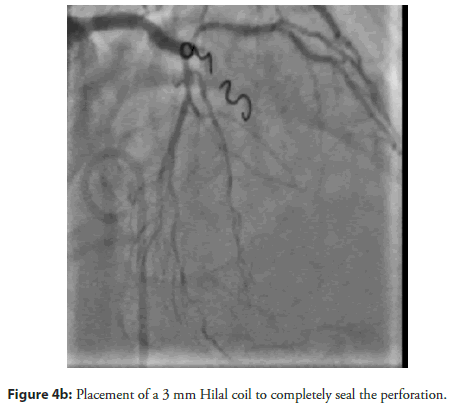
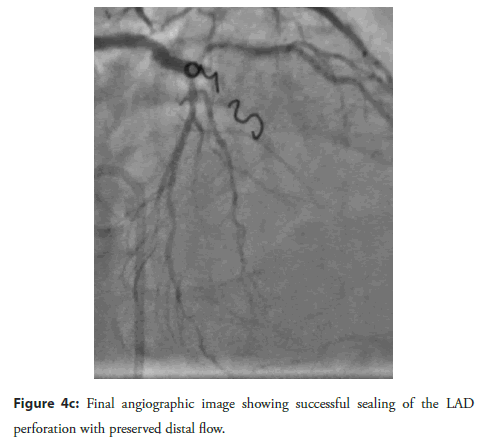
The patient and his family declined Coronary Artery Bypass Graft (CABG) surgery; therefore, the primary treatment strategy was to attempt revascularization of the LAD CTO lesion. An antegrade approach was selected, with the right femoral artery used as the primary access route and the right radial artery used for additional support. The initial attempts were made using Fielder XT, Fielder XT-R, and Gaia Next 2 guide wires (Figure 2a–Figure 2c). However, the Caravel microcatheter could not be advanced across the tight lesion. Therefore, predilatation was attempted using a 1.25 × 10 mm balloon followed by a 2 × 12 mm Non-Compliant (NC) balloon. Unfortunately, the wire was found to be in a false tract, which resulted in a Type III LAD perforation with subsequent cardiac tamponade. Emergency pericardiocentesis was performed (Figure 3a, Figure 3b). The LAD perforation was successfully sealed using 2 mm and 3 mm Hilal coils (Figure 4a–Figure 4c).
Figure 3a: Coronary angiography demonstrating Type III LAD perforation.
Following the procedure, the patient remained stable, and bedside echocardiography showed no remaining pericardial effusion. He was monitored in the Coronary Care Unit (CCU), with the pericardial drain removed the next day. The patient was subsequently discharged in good health without any further complications.
Discussion
The global use of CTO-PCI has steadily increased over time, accompanied by the development of new interventional tools. Among the most commonly used devices are hydrophilic-coated coronary guide wires, which facilitate navigation through complex, calcified, and severely stenotic lesions. However, these wires may inadvertently enter small side branches or penetrate the vessel wall, potentially leading to coronary perforation [5].
At United Hospital Limited, Dhaka, Bangladesh, a major tertiary care center with a strong focus on education, innovation, and technology adoption, numerous CTO-PCI procedures are performed annually, including complex and previously failed cases referred from across the country. While coronary perforation remains a rare complication at our center, the frequent use of hydrophilic guide wires makes awareness of this risk essential. Using the present case report as a reference, we briefly discuss strategies to minimize the risk of perforation and outline effective management approaches.
Strategies to minimize the risk of complications
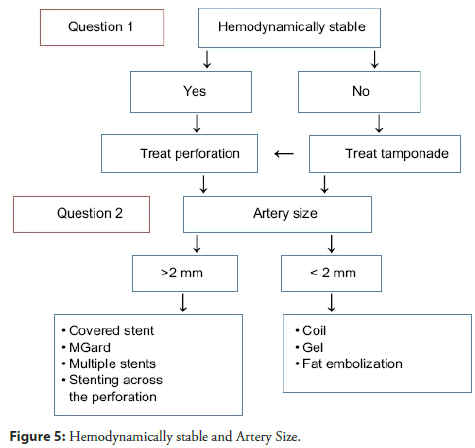
A comprehensive pre-procedural assessment of the patient’s blood profile is essential, including hemoglobin, platelet count, coagulation status, and liver and kidney function (Figure 5).
A number of advancements in technology (new guide wires and micro catheters, new reentry devices), imaging (intravascular imaging for reentry, computed tomography angiography guidance), methods (intra occlusion contrast injection, advanced sub intimal tracking and reentry), and artificial intelligence (automated computed tomography image analysis and prediction of the likelihood of crossing success with various techniques) could further enhance results [6, 7].
The implementation of a bail-out strategy is recommended. For example, in cases of challenging CTO of the LAD, wiring a large diagonal branch prior to the occlusion can provide a safeguard, allowing the operator to stent the perforated segment if necessary. While hydrophilic wires are useful for navigating tortuous and heavily calcified lesions, they can follow blood flow into smaller branches, increasing the risk of perforation. It is advisable to switch to non-hydrophilic wires as soon as feasible. Activated Clotting Time (ACT) should be closely monitored throughout the procedure.
The laboratory should be fully equipped with bedside echocardiography, a pericardial drain set, covered stents, coils, and all emergency medications readily available when performing CTO-PCI.
A well-prepared cathlab team, including an intensivist, and adherence to local cardiac arrest protocols are crucial to promptly manage any life-threatening complications.
Management of coronary perforation
When managing coronary perforation, the sequence of intervention depends on the patient’s hemodynamic status. In hemodynamically stable patients, it is generally recommended to seal the perforation via an antegrade approach before addressing pericardial tamponade. However, if the patient has experienced cardiac arrest or shows signs of impending arrest, immediate treatment of tamponade should take priority before continuing coronary intervention.
The use of fluoroscopy and echocardiography is essential to guide accurate pericardial drainage and ensure effective management of the complication. Repeat echocardiography during the first 24 to 48 hours is essential, as re-accumulation of pericardial fluid is common and perforations may arise from multiple sites simultaneously. Continuous patient monitoring is also recommended, as there is an increased risk of developing pericarditis in the subsequent period. However, in-hospital mortality rates and complications are higher for older patients with high co-morbidity burdens who have CTO-PCI.
Conclusion
Coronary artery perforation is a potentially life-threatening complication of PCI that requires prompt recognition and immediate management. Successful outcomes depend on the operator’s experience, careful planning, and the ready availability of appropriate equipment and resources.
References
- Lansky AJ, Yang YM, Khan Y, et al. Treatment of coronary artery perforations complicating percutaneous coronary intervention with a polytetrafluoroethylene-covered stent graft. Am J Cardiol. 98(3):370-374 (2006).
- Shirakabe A, Takano H, Nakamura S, et al. Coronary perforation during percutaneous coronary intervention. Int Heart J. 48(1):1-9 (2007).
- Ellis SG, Ajluni S, Arnold AZ, et al. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation. 90(6):2725-2730 (1994).
- Ajluni SC, Glazier S, Blankenship L, et al. Perforations after percutaneous coronary interventions: Clinical, angiographic, and therapeutic observations. Cathet Cardiovasc Diagn. 32:206-212 (1994).
- Abushaba, Ahmed G, Salem A, et al. Treatment of distal left anterior descending artery perforation with fat embolization. Heart views. 17(4): 159-163 (2016).
- Kostantinis S, Simsek B, Karacsonyi J, et al. Incidence, mechanisms, treatment, and outcomes of coronary artery perforation during chronic total occlusion percutaneous coronary intervention. Am J Cardiol. 182: 17-24 (2022).
- Azzalini L, Poletti E, Ayoub M, et al. Coronary artery perforation during chronic total occlusion percutaneous coronary intervention: Epidemiology, mechanisms, management, and outcomes. EuroIntervention. 15(9): e804-e811 (2019).