Research Article - Clinical Practice (2023) Volume 20, Issue 2
ASSESSMENT OF THE ROLE OF CLINICAL PHARMACIST IN IMPLEMENTATION OF ANTIMICROBIAL STEWARDSHIP IN A TERTIARY CARE HOSPITAL: AN OBSERVATIONAL STUDY
- Corresponding Author:
- Potu Gayathri
Pharm.D, Department of Pharmacy Practice, Geethanjali College of Pharmacy, Cheeryal (V), Keesara (M), MedchalMalkajgiri (D), Telangana-501301, India
E-mail:potugayathri1@gmail.com
Abstract
Background
A clinical pharmacist plays a key role in the implementation of antimicrobial stewardship by rationalizing antimicrobial use, decreasing the risk of antimicrobial resistance, and improving patient’s health-related quality of life. Objective To emphasize the role of clinical pharmacist in AMSP to develop and manage the optimal use of antimicrobial agents and to promote rational antimicrobial use. To rationalize antimicrobial use, to promote evidence-based medicine, to decrease the occurrence of antimicrobial resistance.
Methods
An observational study was conducted over 6 months in tertiary care hospitals, a total of 152 cases were collected from the patient and patient’s medical record and was assessed.
Results
Among 152 cases, 54 were rational and 98 were irrational irrespective of departments, 48.97% were wrong drug error, 27.55% were inappropriate duration of therapy, 5.1% were drug duplication, 19.38% were multiple antimicrobials for unnecessary use, 3.06% were overdose, 3.06% were subtherapeutic dose and 10.2% were drug without indication. Gram stain 13.26%, culture report 46.93%.
Conclusion
In this observational study, we are concluding that the role of the clinical pharmacist is vital in AMSP. With the implementation of AMSP, there is an opportunity for improvements in the appropriate use of antimicrobials without negatively affecting clinical outcomes.
Keywords
clinical pharmacist, irrational, rational, antimicrobial stewardship, drugrelated problems
Introduction
Clinical Pharmacy is a branch of pharmacy that deals with the practice of rational medication used thereby to promote the health outcomes of patients [1].One of the significant scientific advances of the 20th century is the discovery of antimicrobials which are considered life-saving drugs. Various types of antimicrobials act on micro-organisms with different mechanisms, such as antibacterial or antibiotics against bacteria, antivirals against viruses, antifungals against fungi, etc. A strong Antimicrobial Stewardship Program can both optimize the treatment of infectious diseases and reduce adverse events, cost of treatment, and length of hospital stay associated with antimicrobial use[2].
There has been data stating that antimicrobial misuse is widespread in all healthcare systems. This misuse has led to the development of AMR. Since inappropriate use of antibiotics is excessive in India, there is a need to improve antimicrobial safety in hospitals which can be achieved through the implementation of good “Antimicrobial stewardship” refers to interventions designed to promote the optimal use of antibiotic agents, including drug of choice, dosing, route, and duration of administration [3]. A strong Antimicrobial Stewardship Program can both optimize the treatment of infectious diseases and reduce adverse events, cost of treatment, and length of hospital stay associated with antimicrobial use.
Appropriate antimicrobial therapy is based on hospital guidelines and culture results which selectively report the susceptible pathogen are prominent stewardship practices to improve the rational use of antimicrobials[4].
Antimicrobial stewardship program helps clinicians toImprove the quality of patient care and patient safety, Reduce treatment failures, Prescribe appropriate antimicrobial therapy and prophylaxis,Reduces antimicrobial resistance [5].
■ Goals of antimicrobial stewardship
Primary goal is to optimize safe and appropriate use of antibiotics which improves clinical outcomes and minimizes adverse effects of antimicrobials.
Secondary goal to reduce health care costs by improving the quality of patient care and reduce the incidence of antimicrobials-induced adverse effects.
Antimicrobial stewardship is a key strategy to overcome resistance. It is a program that is designed to review and optimize the use of antibiotics in various health care departments. Implementation of an effective AMSP requires a multidisciplinary approach involving a variety of experts, as most of the hospitals in India lack the structure and process of AMSP [6].
■ Approaches to antimicrobial stewardship
There are 2 major approaches to antimicrobial stewardship:
• Front-end or pre-prescription approach: Prior authorization is required for the use of certain antibiotics.
• Back-end or post-prescription approach: It uses prospective review and feedback. Here recommendations are made to the clinicians on the appropriate use of antibiotics based on the patient's health condition.
The second approach is considered to be more convenient as it includes ADE and promotes reducing antibiotic use [6].
■ Components of antimicrobial stewardship
• Formulary restriction: It regulates the utilization of antibiotics by following the hospital formulary only. Thereby reducing the incidence of antibiotic resistance. It also reduces the treatment cost.
• Switch from parenteral to oral therapy: Long-term use of parenteral therapy may lead to IV-related complications in patients, a switch from parental to oral therapy has benefits like a decrease in duration of hospital stay and healthcare cost.
• Role of microbiology laboratory: It plays a major role in the identification of microorganisms and helps in formulating definitive antibiotic therapy. Escalation and de-escalation: Based on the culture results a more specific and targeted therapy can be designed that helps in decreasing antibiotic exposure and cost.
• 4 D’s (right dose, right drug, right duration, and right dosing interval): By following the 4D’s, one can provide the patient with appropriate antibiotic therapy.
• Point of care interventions: It includes appropriate use of guidance, antibiotic indication, drug of choice, route of administration (IV versus Oral), the prognosis of infection, escalation or de-escalation therapy. Antimicrobial stewardship intervention has an impact on patient morbidity and mortality [6].
■ Steps involved in antimicrobial stewardship
• Identify the patients who require antibiotics based on their subjective and objective findings.
• Obtain culture reports
• Identify antibiotic allergies, if any
• Start appropriate treatment based upon evidence on usage of specific antibiotics and hospital guidelines.
• Monitor the patient closely for any drugrelated problems.
• Based on patient outcomes decide whether to continue, adjust, change, escalate/deescalate or discontinue the therapy.
• Outcomes are based on the days of treatment.
Eg: A 45 year old female patient was admitted to the urology department with chief complaints of burning micturition and fever with chills since one week. Lab data of CUE has shown elevated pus cells and turbid in appearance. A urine sample has been sent for culture to the microbiology lab. Nitrofurantoin was initially started, later the culture reports identified the causative organism as pseudomonas aeruginosa, which is resistant to nitrofurantoin
Hence there is a change in the treatment from nitrofurantoin to piperacillin-tazobactam 4.5gm IV for a duration of 7days[6,7].
■ Antimicrobial stewardship program setting
An AMSP team includes seven parts:
• Infectious disease specialist
• Critical care specialist
• Hospital manager
• Clinical pharmacist for infectious diseases
• Clinical microbiologist
• Epidemiologist and
• Information technology expert subject.
The antibiotics were prescribed based on the antimicrobial susceptibility patterns of isolated microbe. The clinical microbiologist notifies the Pharmacist in regards to the susceptible agent. The data collected is evaluated by the chief pharmacist, results are discussed with the respective physicians, and feedback is sent to the providers in order to either stop, approve, use a sole antibiotic with an increasing/decreasing dose or by going with escalation/de- escalation patterns [8].
Methodology
An observational study was conducted over 6 months in tertiary care hospitals, a total of 152 cases were collected from the patient and patient’s medical record and was assessed [9-12].
■ Inclusion criteria
• Patients of all ages
• Patients of all genders
• Patients with all types of infectious diseases
• Surgery patients (pre-op and post-op)
• Patients of our study site
• Inpatients
■ Exclusion criteria
• Patients of emergency department
• Patients of oncology department
• Active COVID patients
• Outpatients
• ENT department
■ Collection of data
From patient and patient case reports
■ Statistical analysis
Prevalence
■ Expected outcome
Highlighting the role of clinical pharmacist need in AMSP by Improving health related quality of life of patients by rationalizing antimicrobials.
Results & Discussion
This study aims to evaluate and promote the role of clinical pharmacist in implementation of antimicrobial stewardship in a tertiary care hospital.
The appropriate implementation of an antibiotics stewardship program in a secondary care hospital is often challenging, given the involvement of various medical specialties with different department structures.
Antibiotic selection is influenced by the type of organism causing wound infection in the accordance with the international and local hospital guidelines, cephalosporins/penicillins were appropriately selected and administered than other classes of antibiotics (TABLE 1).
■ Reserved drugs used in prescriptions
TABLE 1. Sum of prevalence of DRPs in different departments
| Drug-related problems | % of DRPs identified in different departments |
|---|---|
| Wrong drug error | 48.97 |
| Inappropriate duration of therapy | 27.55 |
| Frequency error | 12.24 |
| Drug duplication | 5.1 |
| Multiple antimicrobials for unnecessary use | 19.38 |
| Overdose | 3.06 |
| Subtherapeutic dose | 3.06 |
| Drug without indication | 10.2 |
Prevalence of drps in various departments: Cases were collected from five departments for this report. The research contained a total of 152 cases, 54 of which were rational and 98 of which were irrational.
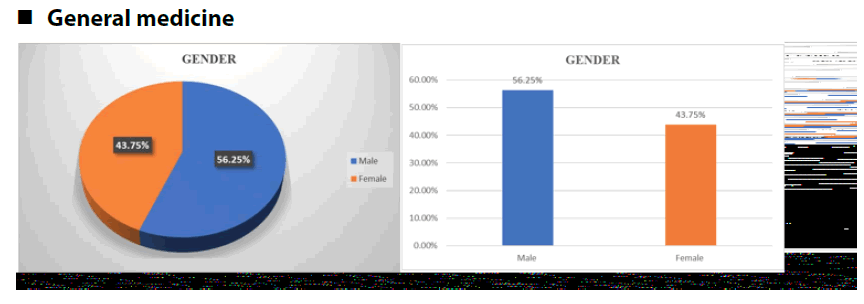
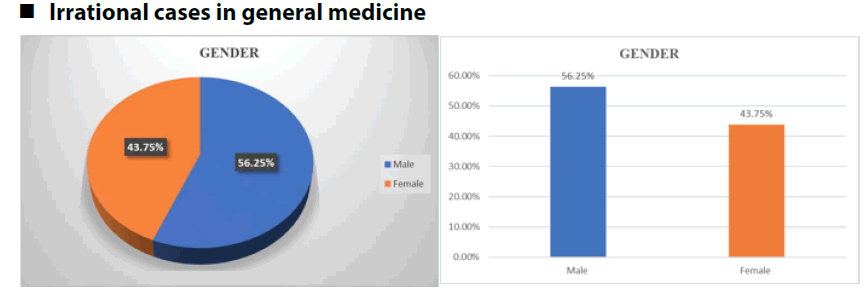
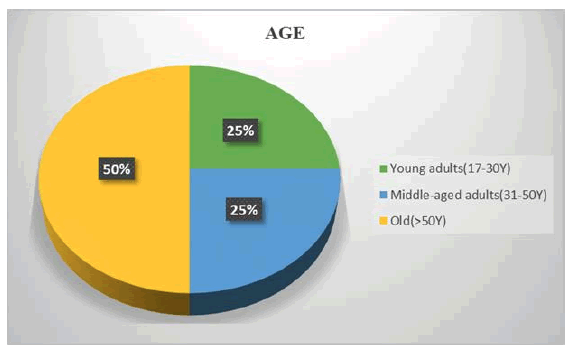
General medicine department:A total of 55 cases were obtained from General Medicine department of which 23 cases (48.18%) were rational and 32 cases (58.18%) were irrational. The total no. of irrational cases was 32 that is 58.18% in General Medicine department. Among 32 cases, 25% of cases were young adults, 25% were middle age and 50% were old age people. Out of 32 cases 56.25% were male and 43.75% were female.
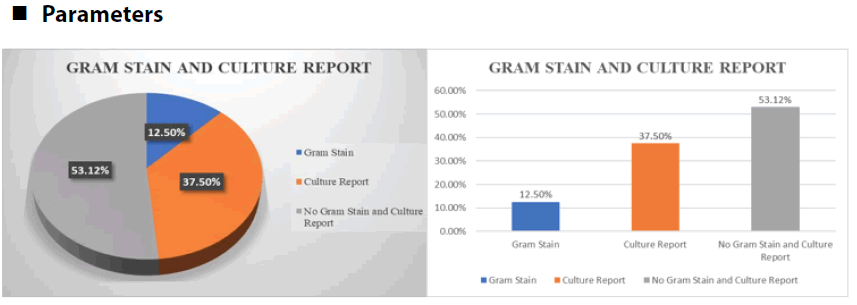
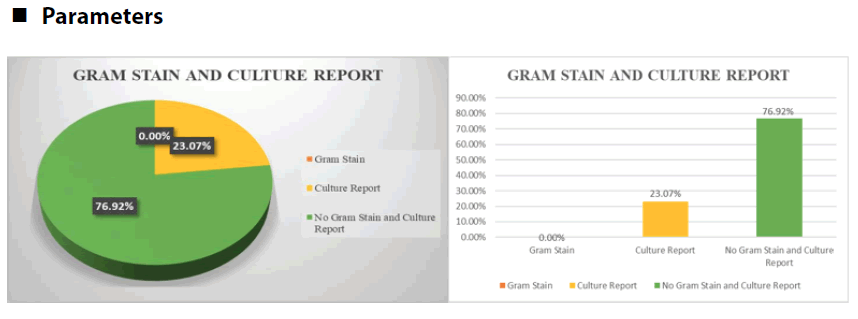
Among 32 irrational cases, gram stain was performed for 9.3% of the cases and for 37.5% of the cases culture and sensitivity test was done. For the remaining 53.12% of the case neither gram stain nor culture and sensitivity test were performed (FIGURE 1-7).
For the 32 irrational cases, Drug-Related Problems (DRP’s) were identified from which 15.6% were due to wrong drug errors, 18.75% were due to inappropriate duration of therapy, 18.75% were due to frequency error, 9.3%
were due to drug duplication, 40.6% were due to multiple antimicrobials for unnecessary use, 3.12% were due to subtherapeutic dose, 12.5% were due to drug without indication. Multiple antimicrobials for unnecessary use were found to be the most common DRP with highest prevalence that is 40.6%. FIGURE 8 shows the prevalence of DRP’s in General Medicine department.
Figure 8: Irrational cases in pulmonology (Gender)
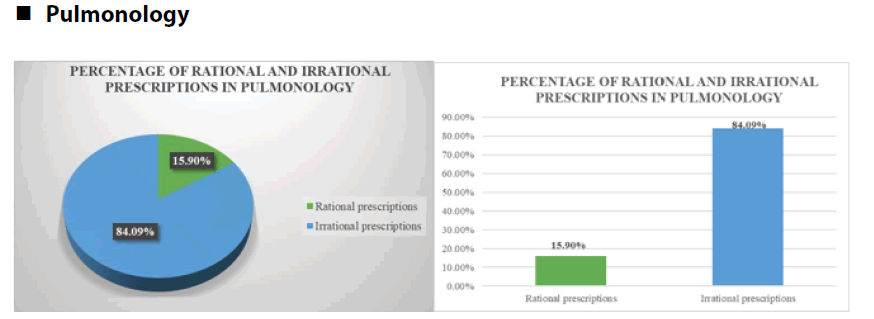
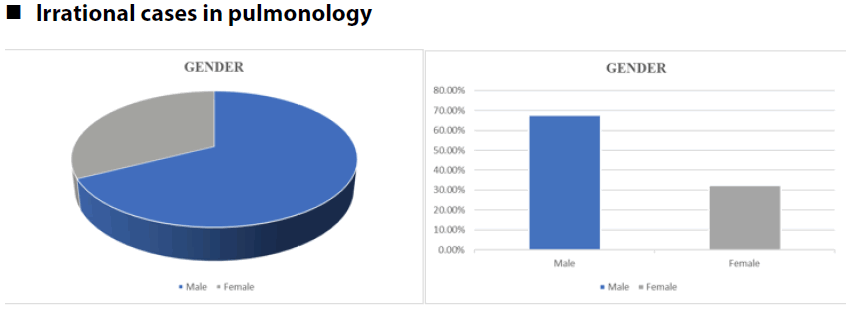
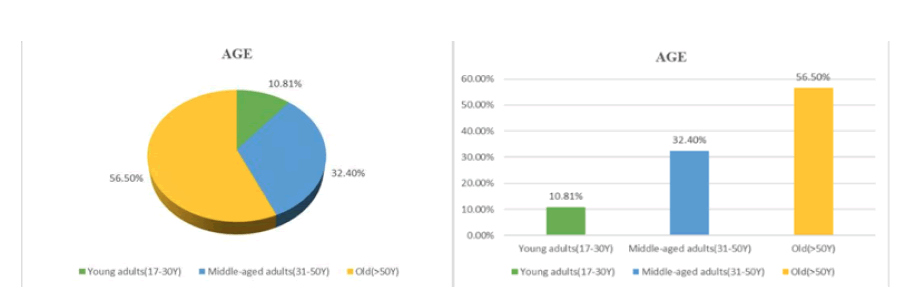
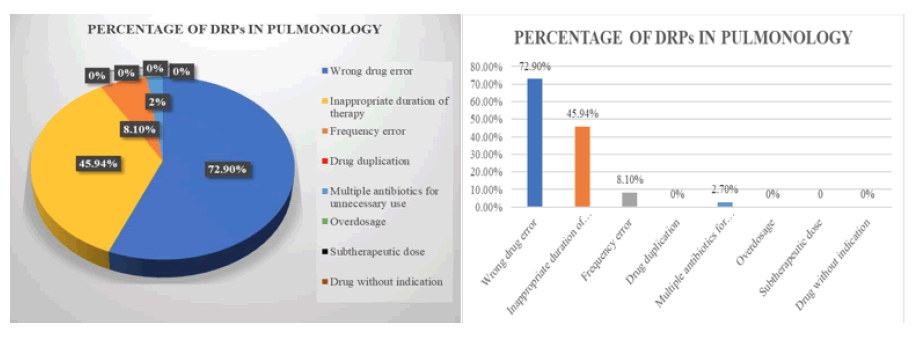
Pulmonology department:A total of 44 cases were obtained from Pulmonology department of which 7 cases (15.9%) were rational and 37 cases(84.09%) were irrational. The total no. of irrational cases was 37 that is 84.09% in Pulmonology department. Among 37 cases, 10.81% of cases were young adults, 32.4% were middle age and 56.75% were old age people. Out of 37 cases 67.56% were male and 32.43% were female.
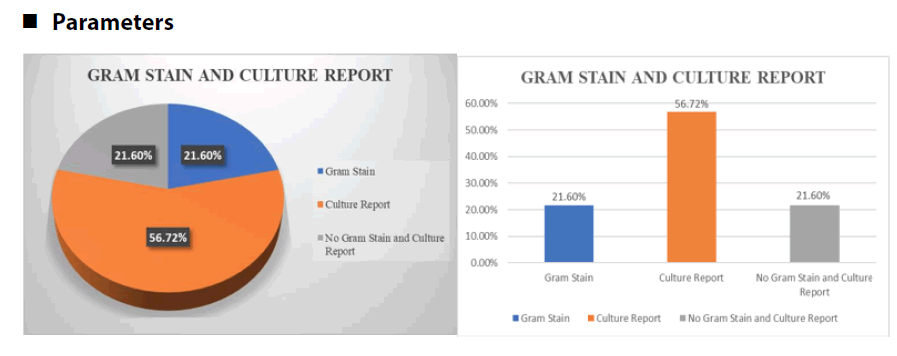
Among 37 irrational cases, gram stain was performed for 21.62% of the cases and for 56.75% of the cases culture and sensitivity test was done. For the remaining 21.62% of the case neither gram stain nor culture and sensitivity test was performed (FIGURE 9-12).
Figure 9: Irrational cases in pulmonology (Age)
For the 37 irrational cases, Drug related problems(DRP’s) were identified, from which 72.97% were due to wrong drug errors, 45.94% were due to inappropriate duration of therapy, 8.1% were due to frequency error, 2.7% were due to multiple antimicrobials for unnecessary use. Wrong drug error was found to be the most common DRP with highest prevalence that is 72.97%. FIGURE 13 shows the prevalence of DRP’s in Pulmonology department.
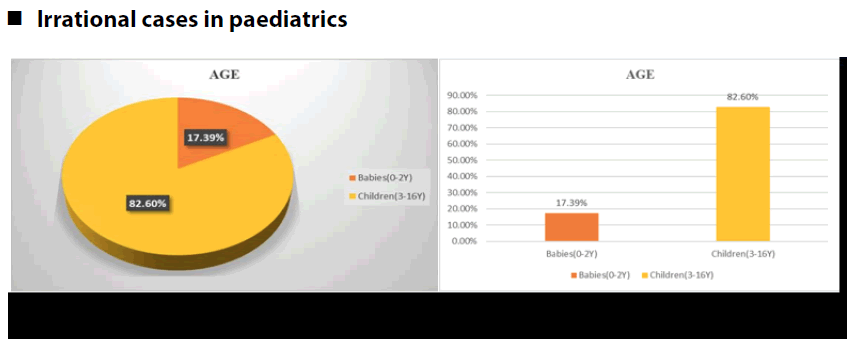
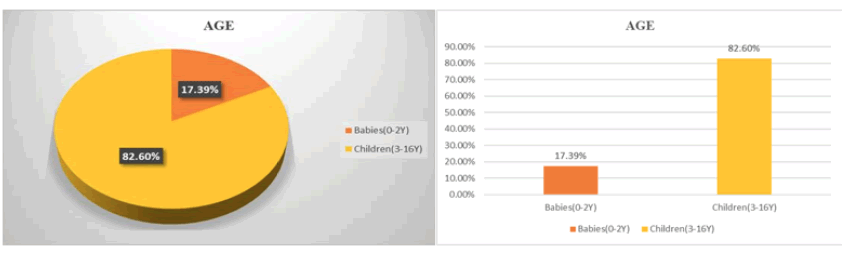
Paediatric department: A total of 23 cases were obtained from Paediatric department of which 10 cases (43.47%) were rational and 13 cases (56.52%) were irrational. Among 23 cases 17.39% of cases were babies, 82.6% were children. Out of 23 cases 52.17% were male and 47.84% were female.
The total no. of irrational cases were 13 that is 56.52% in Paediatric department. Among 13 cases, 23.07% of cases were babies, 76.92% were children. Out of 13 cases 30.76% were male and 69.2% were female.
Among 13 irrational cases, culture and sensitivity test was performed for 23.07% of the cases. Gram stain was not performed. For the remaining 76.92% of the cases neither gram stain nor culture and sensitivity test was performed (FIGURE 14-17)
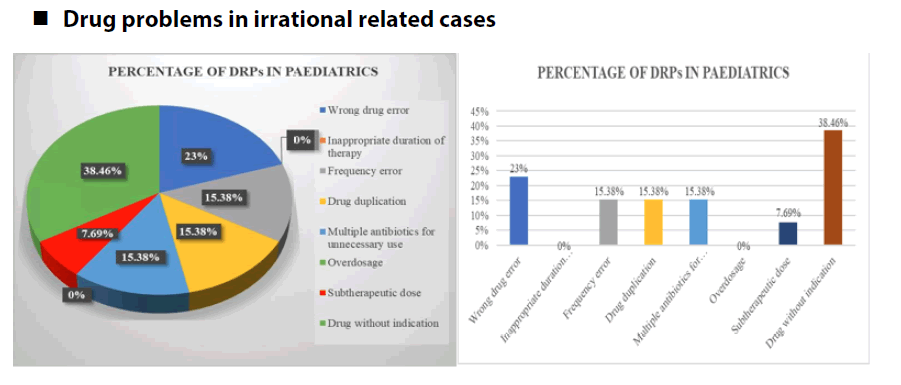
For the 13 irrational cases, Drug related problems(DRP’s) were identified, from which 23.07% were due to wrong drug errors, 15.38% were due to frequency error, 15.38% were due to drug duplication, 15.38% were due to multiple antimicrobials for unnecessary use, 7.69% were due to subtherapeutic dose, 38.46% were due to drug without indication. Drug without indication was found to be the most common DRP with highest prevalence that is 38.46%. FIGURE 18 shows the prevalence of DRP’s in Paediatric department.
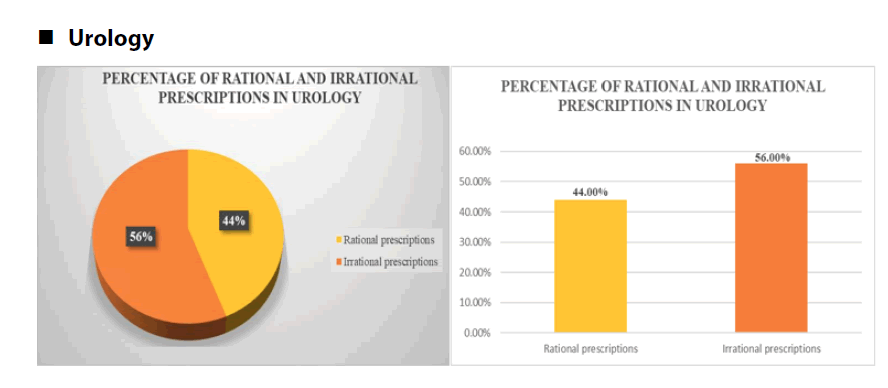
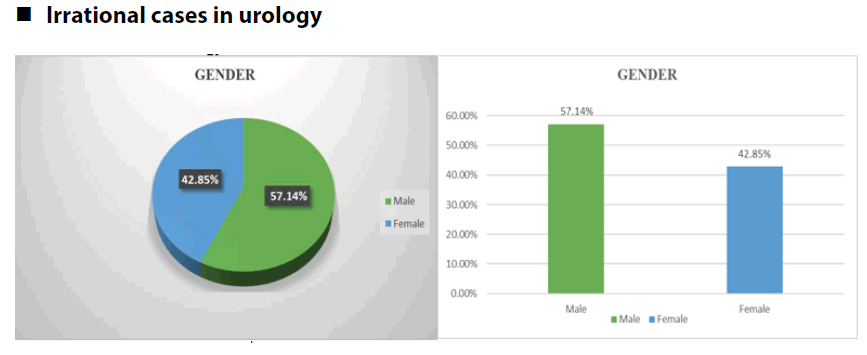
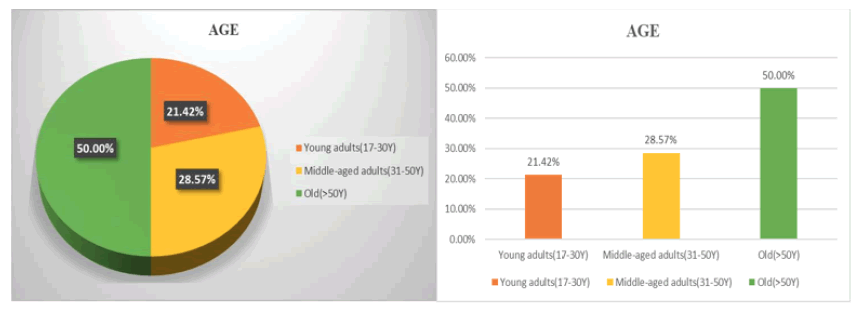
Urology department:A total of 25 cases were obtained from Urology department of which 11 cases(44%) were rational and 14 cases(56%) were irrational. The total no. of irrational cases were 14 that is 56% in Urology department. Among 14 cases, 21.42% of cases were young adults, 28.57% were middle age and 50% were old age people. Out of 14 cases 57.14% were male and 42.85% were female.
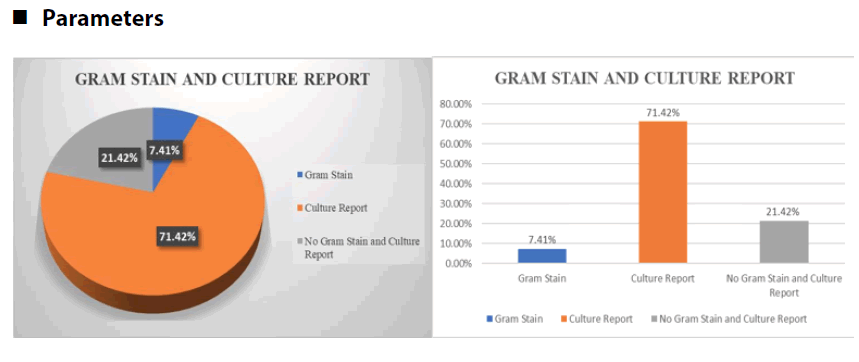
Among 14 irrational cases, gram stain was performed for 7.14% of the cases and for 71.42% of the cases culture and sensitivity test was done. For the remaining 21.42% of the case neither gram stain nor culture and sensitivity test was performed (FIGURE 19-22).
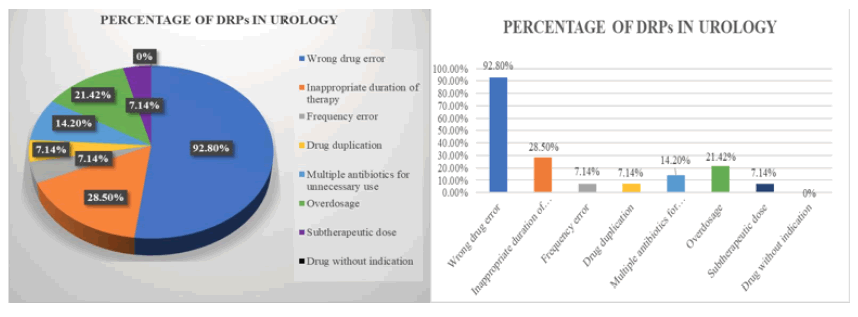
For the 14 irrational cases, Drug Related Problems(DRP’s) were identified, from which 92.8% were due to wrong drug errors, 28.5% were due to inappropriate duration of therapy, 7.14% were due to frequency error, 7.14% were due to drug duplication, 14.2% were due to multiple antimicrobials for unnecessary use, 21.42% were due to overdose, 7.14% were due to subtherapeutic dose. Wrong drug error was found to be the most common DRP with highest prevalence that is 92.8%. FIGURE 23 shows the prevalence of DRP’s in Urology department.
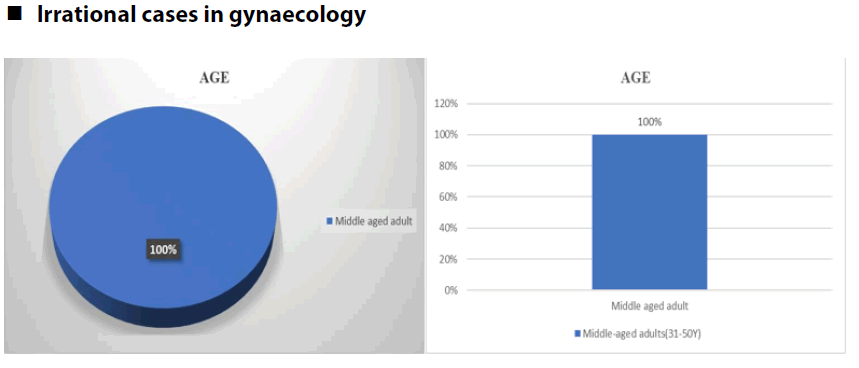
Gynaecology department: A total of 5 cases were obtained from Gynaecology department, of which 3 cases(60%) were rational and 2 cases(40%) were irrational. Among 5 cases, 80% were middle aged and 20% were old age. 100% of the cases were female
The total no. of irrational cases were 2 that is 40% in Gynaecology department. Among 2 cases, 100% were middle age. Among 2 irrational cases, neither gram stain nor culture and sensitivity test was performed.
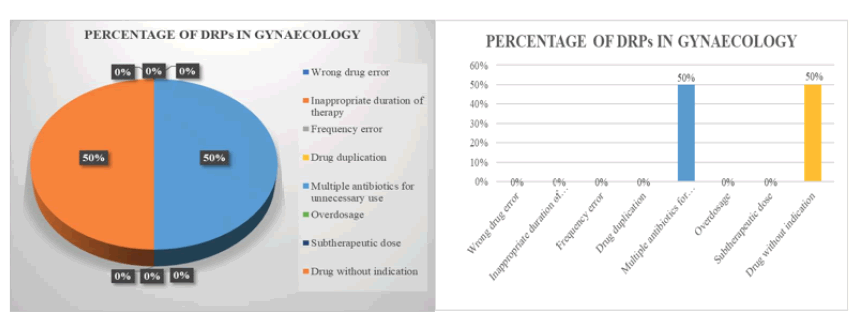
For the 2 irrational cases, Drug related problems(DRP’s) were identified, from which 50% were due to multiple antimicrobials for unnecessary use and 50% were due to drug without indication. FIGURE 24 shows the prevalence of DRP’s in Gynaecology department (TABLES 2-8).
TABLE 2. Drugs used in prescriptions
| S No. | Reserved drugs used | Diagnosis | Rational/Irrational |
|---|---|---|---|
| 1 | Meropenem | Acute Pulmonary Oedema | Irrational |
| 2 | Linezolid | Gangrene of foot | Irrational |
| 3 | Meropenem | AFI | Irrational |
| 4 | Linezolid | Cellulitis | Rational |
| 5 | Meropenem | Hepatic encephalopathy | Irrational |
| 6 | Linezolid | Cellulitis | Irrational |
| 7 | Vancomycin | LRTI | Irrational |
| 8 | Vancomycin | Dengue fever | Irrational |
TABLE 3. Percentage of DRPs in different departments
| Drug related problems | % of DRP’s in General medicine | % of DRP’s in Pulmonology | % of DRP’s in Paediatrics | % of DRP’s in Urology | % of DRP’s in Gynaecology |
|---|---|---|---|---|---|
| Wrong drug error | 15.6 | 72.97 | 23.07 | 92.8 | 0 |
| Inappropriate duration of therapy | 18.75 | 45.94 | 0 | 28.5 | 0 |
| Frequency error | 18.75 | 8.1 | 15.38 | 7.14 | 0 |
| Drug duplication | 9.3 | 0 | 15.38 | 7.14 | 0 |
| Multiple antimicrobials for unnecessary use | 40.6 | 2.7 | 15.38 | 14.2 | 50 |
| Overdose | 0 | 0 | 0 | 21.4 | 0 |
| Subtherapeutic dose | 3.12 | 0 | 7.69 | 7.14 | 0 |
| Drug without indication | 12.5 | 0 | 38.46 | 0 | 50 |
■ Drug related problems in irrational cases
TABLE 4. Prevalence of DRPs in general medicine| Wrong drug error | Inappropriate duration of therapy | Frequency error | Drug duplication | Multiple antibiotics for unnecessary use | Overdosage | Subtherapeutic dose | Drug without indication |
|---|---|---|---|---|---|---|---|
| 15.60% | 18.75% | 18.75% | 9.30% | 40.60% | 0% | 3.12% | 12.50% |
■ Drug problems in irrational related cases
TABLE 5. Prevalence of DRPs in pulmonology
| Wrong drug error | Inappropriate duration of therapy | Frequency error | Drug duplication | Multiple antibiotics for unnecessary use | Overdosage | Subtherapeut ic dose | Drug without indication | |
|---|---|---|---|---|---|---|---|---|
| 0.729 | 0.4594 | 0.081 | 0 | 0.027 | 0 | 0 | 0 |
TABLE 6. Prevalence of DRPs in paediatrics
| Wrong drug error | Inappropriate duration of therapy | Frequency error | Drug duplication | Multiple antibiotics for unnecessary use | Overdosage | Subtherapeutic dose | Drug without indication |
|---|---|---|---|---|---|---|---|
| 23.00% | 0.00% | 15.38% | 15.38% | 15.38% | 0.00% | 7.69% | 38.46% |
■ Drug related problems in irrational cases
TABLE 7. Prevalence of DRPs in urology
| Wrong drug error | Inappropriate duration of therapy | Frequency error | Drug duplication | Multiple antibiotics for unnecessary use | Overdosag e | Subtherapeutic dose | Drug without indication |
|---|---|---|---|---|---|---|---|
| 92.80% | 28.50% | 7.14% | 7.14% | 14.20% | 21.42% | 7.14% | 0.00% |
■ Drug-related problems in irrational cases
TABLE 8. Prevalence of DRPs in gynaecology
| Wrong drug error | Inappropriate duration of therapy | Frequency error | Drug duplication | Multiple antibiotics for unnecessary use | Overdosage | Subtherapeutic dose | Drug without indication |
|---|---|---|---|---|---|---|---|
| 0.00% | 0.00% | 0.00% | 0.00% | 50.00% | 0.00% | 0.00% | 50.00% |
Conclusion
• In this observational study, antimicrobial prescriptions were collected and assessed from five departments for this report. Among 152 cases, 54 of which were rational and 98 of which were irrational as per AMSP.
• DRPs of antimicrobials were identified and the prevalence of different departments was calculated.
• General Medicine: Multiple antimicrobials for unnecessary use were found to be the most common DRP with the highest prevalence that is 40.6%.
• Pulmonology: Wrong drug error was found to be the most common DRP with the highest prevalence that is 72.97%.
• Paediatrics: Drug without indication was found to be the most common DRP with the highest prevalence that is 38.46%.
• Urology: Wrong drug error was found to be the most common DRP with the highest prevalence that is 92.8%.
• Gynaecology: Drug-related problems(DRPs) were identified, from which 50% were due to multiple antimicrobials for unnecessary use and 50% were due to drug without indication.
In this observational study, we are concluding that the role of the clinical pharmacist is vital in AMSP. With the implementation of AMSP, there is an opportunity for improvements in the appropriate use of antimicrobials without negatively affecting clinical outcomes. It also has a significant impact on reducing antimicrobial use by improving quality of care for patients and preventing the emergence of antimicrobial resistance.
Funding
None
Conflict of interest
The authors declare that there is no conflict of interest
References
- R.S.Satoshkar, Pharmacology and pharmacotherapeutics by 26th edition, Elsevier, 567-645;673-717, (2020).
[Google Scholar] [Crossref]
- World Health Organization. "Antimicrobial stewardship: a competency-based approach." (2018).
[Google Scholar] [Crossref]
- AMSP - Antimicrobial Resistance (icmr.org.in)
[Google Scholar] [Crossref]
- Abbo, L M., and Thomas M. H. "Antimicrobial stewardship and urinary tract infections." Antibiotics 3 174-192 (2014):.
- WHO Antimicrobial Stewardship interventions: a practical guide[Google Scholar] [Crossref]
- Rahbarimanesh, A, et al. "Antimicrobial stewardship program (ASP): an effective implementing technique for the therapy efficiency of meropenem and vancomycin antibiotics in Iranian pediatric patients." Ann Clin Microbiol Antimicrob. 18: 1-7 (2019).
- Hwang, S, and Kwon KT. "Core elements for successful implementation of antimicrobial stewardship programs." Infect Chemother. 53): 421 (2021
- Principi, N, and Esposito S. "Antimicrobial stewardship in paediatrics." BMC Infec diseases 16 (2016): 1-8.
[Google Scholar] [Crossref]
- Surat, G, et al. "Defining the scope of antimicrobial stewardship interventions on the prescription quality of antibiotics for surgical intra-abdominal infections." Antibiotics 10: 73 (2021).
[Google Scholar] [Crossref]
- Rossin, S, et al. "Multistep antimicrobial stewardship intervention on antibiotic prescriptions and treatment duration in children with pneumonia." PLoS One 16.10 (2021): e0257993.
[Google Scholar] [Crossref]
- Francis, Nick A., et al. "C-reactive protein point-of-care testing for safely reducing antibiotics for acute exacerbations of chronic obstructive pulmonary disease: the PACE RCT." Health Technol Assess (Winch Engl.) 24: 1(2020). [Google Scholar] [Crossref]
- Seok, Hyeri, Ji Hoon Jeon, and Dae Won Park. "Antimicrobial therapy and antimicrobial stewardship in sepsis." Infect Chemother. 52.1 : 19 (2020). [Google Scholar] [Crossref]