Case Report - Clinical Practice (2023) Volume 20, Issue 4
An isolated pure dislocation of fifth carpometacarpal joint: Case report and review of literature
- Corresponding Author:
- Daoudi Mohamed
Department of Traumatology, Orthopedics, Avicenna Military Hospital, Marrakech, Morocco
E-mail: daoudimonsa@gmail.com
Received: 17 May, 2023, Manuscript No. FMCP-23-99082; Editor assigned: 19 May, 2023, PreQC No. FMCP-23-99082 (PQ); Reviewed: 02 June, 2023, QC No. FMCP-23-99082; Revised: 18 July, 2023, Manuscript No. FMCP-23-99082 (R); Published: 26 July, 2023, DOI: 10.37532/FMCP.2023.20(4).1-3
Abstract
Dislocation of the carpometacarpal joint of the little finger is an uncommon injury. It is subdivided in ulnopalmar and radiopalmar dislocations. The injury can easily be missed on standard xrays. Closed reduction and K-wire fixation has commonly been used in the treatment, although closed reduction and casting has been reported. This article reports a rare type of injury and discusses its management.
Keywords
Dislocation, Carpometacarpal joint, Uncommon injury, Reduction, Radiopalmar dislocations
Introduction
Isolated dislocation of the Carpometacarpal (CMC) joint of the hand is a rare injury. While the dislocation can be dorsal or palmar, dorsal dislocation is more common. Palmar dislocations can be either ulnopalmar or radiopalmar [1-4]. There are very few reports of isolated radiopalmar dislocations of the fifth CMC joint less than 1% of hand injuries.
Case Presentation
A 58 year old man complained of severe pain on his right hand after a fall when he suffered a direct traumatism over ulnar-dorsal side of the hand. Clinical examination showed localised tenderness and moderate swelling over the fifth metacarpal and along the ulnar side of the hand.
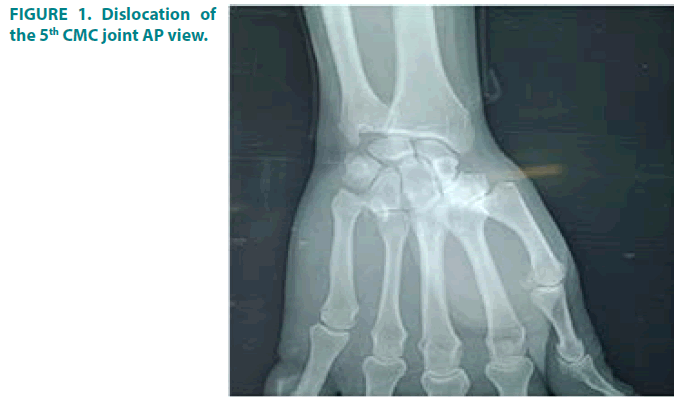
Standard radiographs were obtained which revealed isolated pure dislocation of the fifth carpometacarpal joint without any other associated injury or fracture of other metacarpals or wrist (FIGURE 1).
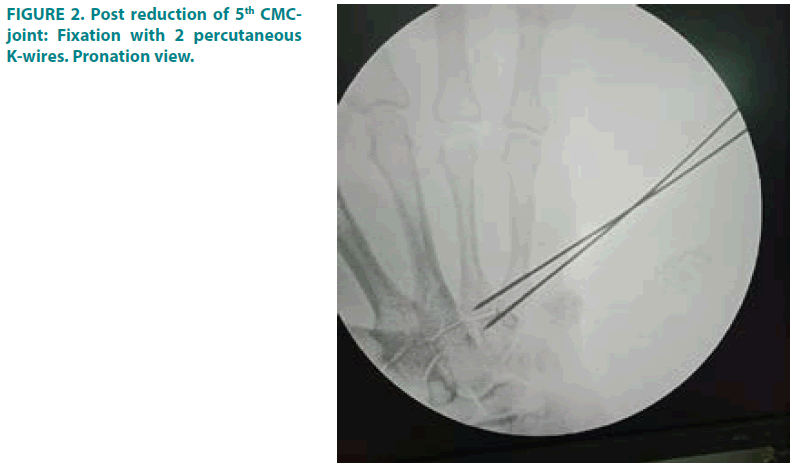
It was decided to reduce the dislocation immediately after the patient was declared fit for surgery. Under axillary block, closed reduction was successful, by longitudinal traction and direct pressure over base of the metacarpal as the reduction was unstable we decided to maintain the position with Kirschner-wires. Two percutaneous K-wires were inserted to fix the base of the 5 metacarpal with the hamate and the base of the 4th metacarpal (FIGURE 2).
The hand was immobilized in a plaster back slab. Plaster and K-wires were removed six weeks postoperatively and physio therapy was started. Four months following injury the patient had full range of movement of the little finger and normal grip strength.
Results and Discussion
Carpometacarpal joint dislocations are uncommon injuries and account for less than 1% of hand injuries [5]. They are classified as dorsal and volar (palmar) dislocations. Dorsal dislocations of the carpometacarpal joints occur more frequently than do volar dislocations, mainly affecting the fourth and fifth digits. Isolated volar or palmar dislocation of the fifth carpometacarpal joint is an uncommon injury that was first reported in 1918 by Mc-Whorter [6].
Stability at the finger carpometacarpal joints is provided by a system of four ligaments. There is a high degree of variation with dorsal, multiple palmar and two sets of interosseous ligaments (only one between the long and ring metacarpals); furthermore, the ECU tendon inserts on the fifth metacarpal base [7]. Dorsal dislocations of the carpometacarpal joints are relatively more frequent as compared to volar, affecting commonly the fourth and fifth fingers [8]. Carpometacarpal dislocations associated with fifth or other metacarpal fracture or hamate fractures are more frequent than pure dislocations. The clinical features of this injury are pain and swelling about the base of the fifth metacarpal and axial deformity of the little finger with apparent shortening.
Anatomical reduction is not difficult to achieve by closed method, but maintaining the reduction of this unstable jointed specially in the presence of swelling can be challenging, so percutaneous Kirsches wire stabilisation is suggested [9]. This treatment is a simple technique that secures anatomic reduction while allowing early motion of the finger. The skeletal fixation should be maintained for six weeks to ensure good healing of the disrupted soft tissues.
In 1918, the first volar CMC dislocation was documented. Since then, the literature has provided a thorough description of CMC dislocations. The rarity of isolated volar fifth CMC dislocations, however, makes them noteworthy for reporting. Depending on whether the fifth CMC joint is displaced dorsally or vertically, dislocations can be categorized. Volar dislocations are less common than dorsal dislocations, which typically afflict the fourth and fifth fingers.
An intricate network of four ligaments, including several palmar, dorsal, and two sets of interosseous ligaments, provides stability at the CMC joints. Only 1 to 3 degrees of motion are permitted by the CMC joints in the index and long fingers, whereas these joints have more lax ligamentous attachments.
The simultaneous dislocation of numerous CMC joints is much more prevalent than the isolated dislocation of any CMC joint. Up to 80% of instances involving multiple CMC joint dislocations include the fifth digit. More frequently than isolated fifth CMC dislocations, occult fifth CMC dislocations arising from fourth metacarpal fractures or hamate fractures happen. Only 1 case of 31 dorsal CMC dislocations of the fifth digit that were the subject of a descriptive investigation happened without a fracture. Additionally, this study discovered that 30% of the cases were initially missing but later discovered [10].
According to the displacement of the fifth metacarpal base, Nalebuff developed two classification schemes for isolated fifth CMC dislocations of the volar subtype: Radial palmar and ulnopalmar. It is called the radial palmar dislocation.
The more frequent subtype is radial palmar dislocation, and in this injury, all ligamentous and tendinous attachments are severed. The flexor carpi ulnaris tendon attachments and the pisometacarpal ligament are both intact in the uncommon ulnopalmar subtype. The fifth metacarpal base is pulled proximally, volarly, and ulnarly by these two attachments. The function of the ulnar nerve must be thoroughly examined because of how close it is to the pisohamate ligament and how easily it can be injured. X-rays of the hand’s Posteroanterior (PA), oblique and lateral surfaces should be taken when CMC dislocation is suspected based on clinical symptoms. The optimal method of diagnosis combines all three perspectives to make the diagnosis. When there is a dislocation on PA plain films, it should be disruption of Gilula arcs, loss of parallelism between CMC joints, or evidence of apparent shortening of the metacarpals.
Open reduction and internal fixation or closed reduction and percutaneous pinning are two surgical techniques for treating CMC dislocations. If the patient doesn’t have any coexisting lesions or has medical reasons why surgery wouldn’t be appropriate, nonsurgical techniques such closure reduction and conservative care with splint immobilization may be recommended. After six weeks of splint immobilization, other examples in the literature have reported great results.
Conclusion
Isolated pure dislocation of the fifth carpometacarpal joint is very rare injury it can be managed conservatively with good outcome if diagnosed early as in our case; however, if the initial reduction is unstable or there is delay in diagnosis or presentation, it is imperative to use K-wires for fixation after closed or open reduction.
Conflicts of interest
Nill
References
- Kumar R, Malhotra R. Divergent fracture-dislocation of the second carpometacarpal joint and the three ulnar carpometacarpal joints. J. Hand. Surg. Am. 26(1),123-9(2001).
[Crossref] [Google Scholar] [PubMed]
- Saleemi AJ, Iqbal MJ. Ulnar dislocation of fifth carpometacarpal joint. Hand. Surg. 10(1),87-0(2005).
[Crossref] [Google Scholar] [PubMed]
- Yamakado K, Hashimoto F, Nagata S, et al. Isolated palmar dislocation of the fifth carpometacarpal joint diagnosed by stress X-rays. Arch. Orthop. Trauma. Surg. 120(9),529-0(2000).
[Crossref] [Google Scholar] [PubMed]
- Fischer JW, Waseem M, Gambhir A, et al. Ulnopalmar dislocation of the fifth carpometacarpal joint: A rare injury. Acta Orthop Belg. 68(2),175–7(2002).
[Google Scholar] [PubMed]
- John G, Horneff III, Park MJ, et al. Acute closed dislocation of the second through fourth carpometacarpal joints: Satisfactory treatment with closed reduction and immobilization. Hand. 8(2),227-1(2013).
[Crossref] [Google Scholar] [PubMed]
- Domingo A, Font L, Saz L, et al. Isolated radial palmar dislocation of the fifth carpometacarpal joint with ulnar neuropathy associated: Successful treatment with closed reduction and internal fixation. Eur. J. Orthop. Surg. Traumatol. 19(2),101-7(2002).
- Syed AA, Agarwal M, Giannoudis PV, et al. Dorsal hamatometacarpal fracture dislocation in a gymnast. Br. J. Sports. Med. 36(5),380-2(2002).
[Crossref] [Google Scholar] [PubMed]
- Nakamura K, Patterson RM, Viegas SF. The ligament and skeletal anatomy of the second through fifth carpometacarpal joints and adjacent structures. J. Hand. Surg. Am. 26(6),1016-9(2001).
[Crossref] [Google Scholar] [PubMed]
- Busa R, Internullo G, Caroli A. Divergent dislocation of the fourth and fifth carpometacarpal joints. J. Hand. Surg. Am. 23(3),529-1(1998).
[Crossref] [Google Scholar] [PubMed]
- Dzwierzynski WW, Matloub HS, Yan JG, et al. Anatomy of the intermetacarpal ligaments of the carpometacarpal joints of the fingers. J. Hand. Surg. Am. 22(5),931-4(1997).
[Crossref] [Google Scholar] [PubMed]