Editorial - Interventional Cardiology (2013) Volume 5, Issue 5
Access route for coronary chronic total occlusion: femoral or radial approach?
- Corresponding Author:
- Giampaolo Niccoli
Institute of Cardiology, Catholic University of the Sacred Heart
Largo Francesco Vito, 1, 00168, Rome, Italy
Tel: +39 0630154187
Fax: +39 063055535
Abstract
Keywords
chronic total occlusion, device compatibility, transfemoral approach, transradial approach
Percutaneous coronary intervention (PCI) of coronary chronic total occlusions (CTO) has historically been limited by technical success rates of 50–70%, despite being performed in highly selected cases. Currently, however, operators and programs with greater experience of CTO interventions and modern techniques and technologies can consistently achieve technical success rates of >80% in a more unselected and complex population of CTO patients [1–3]. The transfemoral approach (TFA) represents the most extensively used access route for CTO treatment. However, recently there has been growing interest in using the transradial approach (TRA) to perform PCI for CTO [4,5].
In this editorial, we analyze the pros and cons of selecting the TFA or TRA when approaching a CTO.
Why select a TFA for CTO interventions?
TFA is the most extensively used access route for CTO treatment. Most experts use the femoral approach for the target CTO vessel (90% in Europe) and it has not been shown that either access is preferable, except for approximately 10% of the cases, in which even experienced radial operators select the femoral route [3,4].
The selection of the access route for approaching a CTO may depend on both the vascular characteristics of the individual patient (e.g. the presence of a severe peripheral vascular disease may preclude a TFA) and on the operator’s preference [6]. According to the standard practice of the majority of CTO-dedicated centers and operators, PCI on CTO is attempted using large guiding catheters (GCs; 7–8 F) by TFA, allowing for free CTO technique selection in the course of the CTO PCI procedure. On the contrary, GC size is limited from the radial approach, as radial operators often select 6-F GCs for CTO PCI in order to avoid excessive injury to the small sized radial artery.
In particular, when approaching a CTO, a good passive support to push wires, microcatheters and balloons across the occlusive lesion is crucial, and passive support is greater with larger GCs (7 and 8 F). Thus, when the need of high support from the GC is anticipated, the possibility to electively select a TFA should be considered. This approach is especially important for proximal or ostial occlusions, where the active support deriving from a deep GC engagement is not possible, and a good passive support is crucial.
Moreover, in the setting of CTO interventions, operators adopting the TRA should pay more attention on the materials’ compatibility compared with operators using systematically large GCs by TFA. This issue is complicated by the fact that same materials (e.g., same size balloons) of different manufacturers may have different widths, thus influencing their possibility to be inserted in GCs together with other devices. It is evident that the selection of 6-F GCs may profoundly limit the freedom to select some CTO techniques, so that 7 F are required when some complex, specific techniques are needed. In particular, a 7-F GC is required to perform a parallel wire technique when both wires are supported by a microcatheter and an over-the-wire balloon, and a 8-F GC when both wires are supported by two over-the-wire balloons [7]. Indeed, when complex techniques are performed, such as controlled antegrade and retrograde subintimal tracking (CART) and reverse-CART techniques, which require the simultaneous use of multiple devices, larger size GCs are recommended. Moreover, a 7-F GC is required to perform an intravascular ultrasound guidance with a simultaneous microcatheter inside, or when planning to use a Rotablator® 2.0–2.25 mm (Boston Scientific, MN, USA) or a Laser 1.7–2.2 mm [6,7]. Finally, large GCs allow better visualization of the collaterals originating from the donor vessel.
Owing to the procedural relevance of a stable coronary cannulation during the long CTO procedures, TFA operators are increasingly using long, armored sheaths for both antegrade and retrograde access. Such an approach results in a larger femoral artery hole and may have implications for postprocedural hemostasis. Nevertheless, in the expert hands of European and Japanese operators practicing mainly TFA for CTO, the rate of access site complications has been reported to be acceptable.
Why select a transradial approach for CTO interventions?
It is standard practice for the majority of CTOdedicated centers and operators to adopt a large GC in the femoral artery as the preferred strategy to start a PCI on a CTO lesion. However, it is well known that the use of femoral artery access is associated with higher rates of hemorrhagic and vascular entry site complications compared with the TRA [8]. Moreover, the TRA allows patients to be mobilized earlier and reduces hospital costs, compared with the TFA [9], and as demonstrated in recent observational reports, may also result in a more favorable clinical outcome [10–12]. For these reasons, there is a growing interest worldwide regarding the replacement of TFA with TRA for coronary and peripheral interventions [13–17]. Furthermore, both the miniaturization of CTO-dedicated devices and the improvement of techniques for complex PCI is going to provide an improved armamentarium for interventional cardiologists to successfully approach CTO PCI by radial access. Indeed, as double arterial access and long procedures are often required, one benefit may be anticipated with radial-associated reduction of vascular complications in CTO PCI. However, the issue of vascular complications in the TFA CTO PCI studies is by far underestimated [18,19], as vascular complications are usually not reported. Another point in favor of TRA use in CTO PCI comes from the literature where, even if the data come exclusively from observational studies comparing TRA and TFA in treating CTO lesions [20–24], the PCI success rate in the TRA group is not significantly inferior to the TFA group in all of the studies with a significant reduction of access site complications in TRA [21,24].
On the other hand, TRA is not as ‘easy’ to adopt because it is associated with some specific technical issues and, as a consequence, with the need of a learning curve for all operators. This concept is evident when looking at the literature data on PCI in CTO lesions treated by the radial approach and by expert radialists. Four single-center observational studies on TRA for PCI in CTO lesions provided data regarding the comparison of TRA PCI success rate between a first and a later period of the study, demonstrating that it significantly improves in the second period of the study with an increased operator experience after a first period of learning curve [20,25–27].
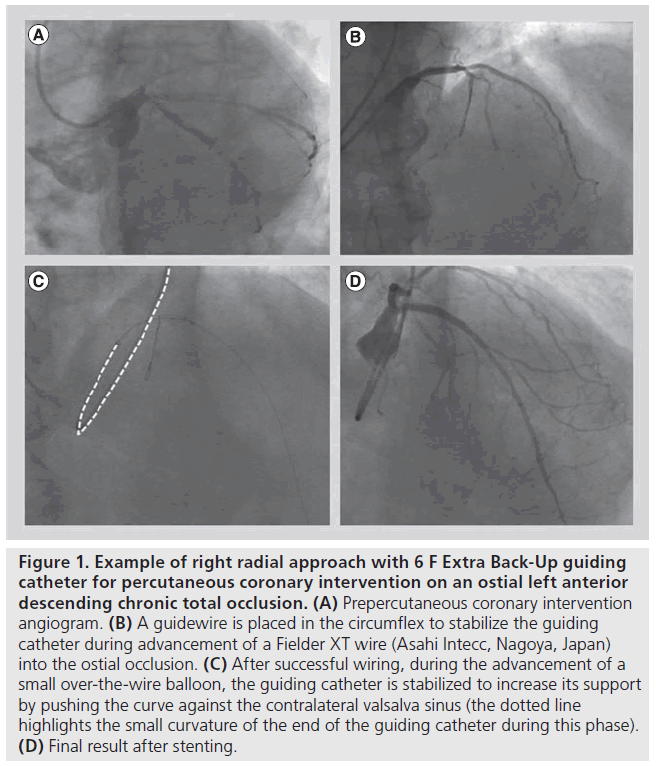
The main differences between TRA and TFA in CTO PCI (requiring a learning curve) are the knowledge of the techniques to improve back-up by the GC and the full knowledge of materials’ compatibility with different sizes of GCs [7]. Indeed, the small radial artery diameter allows the use of large sized GCs (such as 8 F in only a proportion of patients) [28], while only 5–6 F GC may routinely be used in transradial PCI. This is supported by the literature demonstrating that radialist operators approaching a CTO lesions by TRA select a 6-F GC in more than 70% of cases (see Figure 1 for example of 6 F GC for ostial left anterior descending CTO intervention) [20–27,29,101,102]. As a consequence, the radial operator is commonly more focused on the material compatibility and the technical plan of CTO PCI [7]. Regarding the issue of GC support, the interventional cardiologist adopting the TRA for CTO usually tries to gain the maximal ‘active’ back-up from small GCs (for instance, liberally adopting the deep intubation technique) and reserves the usage of large GCs, with their better passive back-up, only for specific techniques which require bulky materials [30]. When looking for the best active support, a useful trick is to select the best radial artery entry site in order to achieve a stable GC cannulation. For these reasons the left radial artery is better for right coronary artery CTOs and the right radial artery is better for left coronary artery CTOs (see Figure 1 for an example of ‘supportive’ seating of extra backup GC in the aortic root during left radial CTO PCI in the ostial left anterior descending artery) [26]. Besides the previously mentioned deep intubation technique, other possibilities to increase active back-up are the anchoring balloon technique and the ‘five in six technique’ (or ‘motherand- child technique’) [31], greatly facilitated by dedicated devices (Terumo Heartrail™ catheter, Terumo Corp., Tokyo, Japan; or the novel GuideLiner™, Vascular solutions, MN, USA).
Figure 1: Example of right radial approach with 6 F Extra Back-Up guiding catheter for percutaneous coronary intervention on an ostial left anterior descending chronic total occlusion. (A) Prepercutaneous coronary intervention angiogram. (B) A guidewire is placed in the circumflex to stabilize the guiding catheter during advancement of a Fielder XT wire (Asahi Intecc, Nagoya, Japan) into the ostial occlusion. (C) After successful wiring, during the advancement of a small over-the-wire balloon, the guiding catheter is stabilized to increase its support by pushing the curve against the contralateral valsalva sinus (the dotted line highlights the small curvature of the end of the guiding catheter during this phase). (D) Final result after stenting.
A further improvement in the technical armamentarium that may facilitate some TRA CTO, will be provided by the recent introduction of a new family of GC specific for radial arteries that do not require the insertion of a sheath, commonly called ‘sheathless’ GC (first available type: Eaucath, Asahi Intecc, Nagoya, Japan) allowing (in the 7.5-F size) an inner lumen larger than the 7-F GC, with an outer diameter smaller than a 6-F sheath [7].
Conclusion
Treatment of CTO is attempted with higher success rates in the last few years owing to both increased experience and better availability of devices. The choice of the access route may be important, as in other types of lesions, in order to lower the rate of access site complication, especially when anticoagulation is as prolonged as in CTOs. Radial access, known to be associated with lower access site complications, is emerging as an alternative to femoral access for treating CTO. We may expect that the development of dedicated devices may widen the use of such an approach, even if the femoral route may still be the preferred approach for complex CTO cases, where the need of multiple devices in the coronary artery is anticipated.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- Prasad A, Rihal CS, Lennon RJ, Wiste HJ, Singh M, Holmes DR Jr. Trends in outcomes after percutaneous coronary intervention for chronic total occlusions: a 25-year experience from the Mayo Clinic. J. Am. Coll. Cardiol. 49, 1611–1618 (2007).
- Mehran R, Claessen BE, Godino C et al. Long-term outcome of percutaneous coronary intervention for chronic total occlusions. JACC Cardiovasc. Interv. 4, 952–961 (2011).
- Galassi AR, Tomasello SD, Reifart N et al. In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. EuroIntervention 7, 472–479 (2011).
- Rao SV, Ou F, Wang TY et al. Trends in the prevalence and outcomes of radial and femoral approaches to percutaneous coronary intervention. JACC Cardiovasc. Interv. 1, 379–386 (2008).
- Bertrand OF. Radial versus femoral approach for chronic total occlusion: pushing the envelope further! Catheter. Cardiovasc. Interv. 73, 888–889 (2009).
- Sianos G, Werner GS, Galassi AR et al.; EuroCTO Club. Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention 8(1), 139–145 (2012).
- Burzotta F, De Vita M, Lefevre T, Tommasino A, Louvard Y, Trani C. Radial approach for percutaneous coronary interventions on chronic total occlusions: Technical issues and data review. Catheter.Cardiovasc. Interv. doi:10.1002/ccd.25118(2013) (Epub ahead of print).
- Agostoni P, Biondi-Zoccai GG, de Benedictis ML et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures; systematic overview and meta-analysis of randomized trials. J. Am. Coll. Cardiol. 44(2), 349–356 (2004).
- Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am. Heart J. 157, 132–140 (2009).
- Chase AJ, Fretz EB, Warburton WP et al. Association of the arterial access site at angioplasty with transfusion and mortality: the M.O.R.T.A.L study (Mortality benefit Of Reduced Transfusion after percutaneous coronary intervention via the Arm or Leg). Heart 94, 1019–1025 (2008).
- Pristipino C, Trani C, Nazzaro MS et al.; Prospective REgistry of Vascular Access in Interventions in Lazio Region Study Group. Major improvement of percutaneous cardiovascular procedure outcomes with radial artery catheterisation: results from the PREVAIL study. Heart 95, 476–482 (2009).
- Sciahbasi A, Pristipino C, Ambrosio G et al. Arterial access-site-related outcomes of patients undergoing invasive coronary procedures for acute coronary syndromes (from the ComPaRison of Early Invasive and Conservative Treatment in Patients With Non-ST-ElevatiOn Acute Coronary Syndromes [PRESTO-ACS] Vascular Substudy). Am. J. Cardiol. 103, 796–800 (2009).
- Burzotta F, Hamon M, Trani C, Kiemeneij F. Direct coronary stenting by transradial approach: rationale and technical issues. Catheter. Cardiovasc. Interv. 63(2), 215–219(2004).
- Burzotta F, Trani C, Hamon M, Amoroso G, Kiemeneij F. Transradial approach for coronary angiography and interventions in patients with coronary bypass grafts: tips and tricks. Catheter. Cardiovasc. Interv. 72(2), 263–272 (2008).
- Trani C, Tommasino A, Burzotta F. Transradial renal stenting: why and how. Catheter. Cardiovasc. Interv. 74(6), 951–956(2009).
- Trani C, Burzotta F, Tommasino A, Giammarinaro M. Transradial approach to treat superficial femoral artery in-stent restenosis. Catheter. Cardiovasc. Interv. 74(3), 494–498 (2009).
- Trani C, Burzotta F, Coroleu SF. Transradial carotid artery stenting with proximal embolic protection. Catheter. Cardiovasc. Interv. 74(2), 267–272 (2009).
- Suero JA, Marso SP, Jones PG et al. Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J. Am. Coll. Cardiol. 38(2), 409–414 (2001).
- Ivanhoe RJ, Weintraub WS, Douglas JS Jr et al. Percutaneous transluminal coronaryangioplasty of chronic total occlusions. Primary success, restenosis, and long-term clinical follow-up. Circulation 85(1), 106–115 (1992).
- Saito S, Tanaka S, Hiroe Y et al. Angioplasty for chronic total occlusion by using tapered-tip guidewires. Catheter. Cardiovasc. Interv. 59(3), 305–311 (2003).
- Rathore S, Hakeem A, Pauriah M, Roberts E, Beaumont A, Morris JL. A comparison of the transradial and the trans-femoral approach in chronic total occlusion percutaneous coronary intervention. Catheter. Cardiovasc. Interv. 73(7), 883–887 (2009).
- Yang CH, Guo GB, Chen SM et al. Feasibility and safety of a transradial approach in intervention for chronic total occlusion of coronary arteries: a single-center experience. Chang Gung Med. J. 33(6), 639–645 (2010).
- Ferrante G, Louvard Y, Hayashida K et al. Radial versus femoral access for percutaneous coronary interventions in patients with chronic total occlusions. J. Am. Coll. Cardiol. 60N(7 Suppl. B), 128 (2012).
- Asgedom S, Bjornstad P, Patten R, McAdam B, Sheahan R, Foley D. Radial approach to CTO recanalization is as successful and safer than femoral: single centre observational study. J. Am. Coll. Cardiol. 60N(7 Suppl. B), 131 (2012).
- Kim JY, Lee SH, Choe HM, Yoo BS, Yoon J, Choe KH. The feasibility of percutaneous transradial coronary intervention for chronic total occlusion. Yonsei Med. J. 47(5), 680–687 (2006).
- Burzotta F, Trani C, Tommasino A et al. Impact of operator experience and wiring technique on procedural efficacy of trans-radial percutaneous chronic total occlusion recanalization performed by dedicated radialists. Cardiol J. doi:10.5603/ CJ.a2013.0063 (2013) (Epub ahead of print).
- Wu CJ, Fang HY, Cheng CI et al. The safety and feasibility of bilateral radial approach in chronic total occlusion percutaneous coronary intervention. Int. Heart J. 52(3), 1312–138 (2011).
- Saito S, Ikei H, Hosokawa G, Tanaka S. Influence of the ratio between radial artery inner diameter and sheath outer diameter on radial artery flow after transradial coronary intervention. Catheter. Cardiovasc. Interv. 46(2), 173–178 (1999).
- Liu W, Wagatsuma K, Toda M et al. Short- and long-term follow-up of percutaneous coronary intervention for chronic total occlusion through transradial approach: tips for successful procedure from a single-center experience. J. Interv. Cardiol. 24(2), 137–143 (2011).
- Ikari Y, Masuda N, Matsukage T et al. Backup force of guiding catheters for the right coronary artery in transfemoral and transradial interventions. J. Invasive Cardiol. 21(11), 570–574 (2009).
- Takahashi S, Saito S, Tanaka S et al. New method to increase a backup support of a 6 French guiding coronary catheter. Catheter. Cardiovasc. Interv. 63(4), 452–456 (2004).
- Quesada R. Transradial approach to CTO: techniques, results and why. www.tctmd.com/show.aspx?id=398&ref_ id=71432
- Katsuki T. Is the transradial approach a reasonable option for most CTOs? www.tctmd.com/show.aspx?id=398&ref_ id=84448
▪ Websites