Case Report - International Journal of Clinical Rheumatology (2017) Volume 12, Issue 2
A young lady with seronegative systemic lupus erythematosus
- *Corresponding Author:
- De Zoysa HDJ
Teaching Hospital, Jaffna, Sri Lanka
E-mail: jeewakadezoysa@yahoo.com
Abstract
Systemic lupus erythematosus (SLE) is a chronic inflammatory autoimmune disease. It is a multisystem disease which can involve any organ in the body. Most of the SLE cases are seropositive which depend on positive test for antinuclear antibody (ANA), Lupus erythematous (LE) cells, and antibody to DNA but seronegative SLE cases also rarely can present with complications.
Keywords
systemic lupus erythematosus, antinuclear antibody, PRES syndrome
Introduction
Systemic lupus erythematosus (SLE) is a chronic inflammatory autoimmune disease that may affect any organ of the body such as the skin, joints, kidneys, nervous system, heart, lungs and the serous membranes [1]. This disease is characterized by the production of antibodies to components of the cell nucleus. It shows broad spectrum of clinical and immunological manifestations. Disease is common in female with child bearing age group. Antinuclear antibody (ANA) and anti-double stranded DNA (anti ds-DNA) antibody are usually associated with SLE. But it is not essential for the diagnosis. ANA negative SLE was first introduced by Koller et al. with five cases with clinical features similar to SLE [2]. Here we report a young lady presented with pyrexia of unknown origin which was complicated with acute renal impairment and altered level of consciousness and later diagnosed as seronegative SLE.
Case report
A 27 years old female patient with past history of primary subfertility presented with on and off fever for 6 months duration. It was associated with intermittent episodes of non-migratory asymmetrical large and small joint pain and swelling. Patient had loss of appetite and 10 kg weight reduction within that period. She did not have any bowel or bladder symptoms. There was no contact history with chronic diseases such as Tuberculosis.
On examination, patient was febrile and ill looking. She was wasted and body mass index (BMI) was 16.3 kg/m2. Patient had alopecia and generalized lymphadenopathy. There was a photosensitive diffuse popular rash on forehead and upper chest (Figure 1). Cardiovascular, respiratory and neurological examinations were normal. She had proximal interphalangial arthritis but no joint deformity.
But 13th day of second hospital admission patient suddenly became restless and confused. She developed reduced urine output. Even though she had fever, there were no episodes of fits. Patient’s Glasgow coma scale (GCS) was 12/15 but there was no papilledema or neck stiffness. She did not have any focal neurological signs such as long tract signs or cranial nerve palsy. BP was 180/120 mmHg on two occasions on that day even though other BP readings were normal prior to this event.
Our initial differential diagnoses for her presentation were connective tissue diseases such as SLE, pulmonary tuberculosis, hemophagocytic histiocytosis, hematological malignancies such as leukaemia and lymphoma, other infections such as Ebstein Barr Virus (EBV) and kikuchi disease.
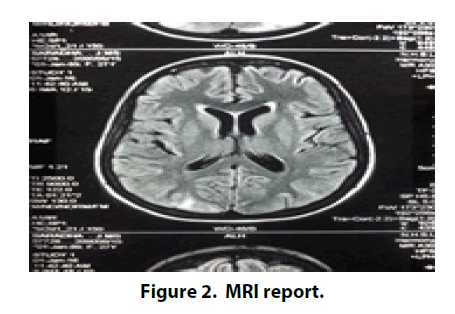
Full Blood Count (FBC) showed mild leucopenia and microcytic hypochromic anaemia with Haemoglobin (Hb) 8.3 g/dl. Patient’s initial urine analysis was abnormal with red cells and red cell casts. Erythrocyte sedimentary rate was 106 mm/1st h and C reactive protein was 65 mg/dl on admission. Except total protein, rest of the liver function was normal. Albumin was low throughout the hospital admission with reversed albumin and globulin ratio. Renal functions were normal on admission but rising after the admission. Serum creatinine reached the maximum value of 345 mg/dl by 20th day. But it started to come down with treatment. Chest X ray, abdominal ultrasound and 2D echocardiography were normal. Septic screening was normal. ANA, ds-DNA and Rheumatoid factor were negative. Mantoux test and 3 sputum samples were negative. Lymph node biopsy showed reactive lymph node with prominent interfollicular cells. Bone marrow aspiration showed a reactive marrow. There were T2W and FLAIR hyper intensities seen in bilateral parieto-occipital lobes in MRI scan of the head. MRI was reported as appearances were likely due to posterior reversible leukoencephalopathy (Figure 2).
After considering above clinical manifestations and investigation findings, seronegative SLE complicated with posterior reversible encephalopathy syndrome (PRESS) was diagnosed according to the 1997 American College of Rheumatology (ACR) criteria for SLE [3]. This patient had cutaneous manifestations, non-erosive arthritis, cerebral lupus, lupus nephritis and leucopenia for the SLE diagnosis.
Patient was initially treated with intravenous pulse methylprednisolone 1 g/day for 3 days followed by oral prednisolone 1 mg/kg/day. She improved significantly with steroids. Her anaemia was treated with 3 pints of blood transfusions followed by oral haematinics. After the steroid was tailed off, Hydroxychloroquine 200 mg bd and Azathioprine 50 mg daily were started as steroid sparing immunosuppressive drugs.
Discussion
SLE is a multi-system auto immune disorder with varied clinical presentations. It is of unknown etiology and manifests by the deposition of pathologic autoantibodies and immune complexes into the tissues and cells. 90- 95% of SLE patients are positive for ANA and its titre is one of the key diagnostic criteria for SLE. But ANA positivity is not mandatory for the diagnosis [4]. Sero-negativity in lupus patients may be due to technical failure or entrapment of ANA in circulating immune complexes.
The concept of ANA-negative lupus was first introduced by Koller et al. Cutaneous manifestation, particularly photosensitivity was the predominant feature in first few cases of seronegative SLE.
The diagnosis of SLE can be made by combining clinical and laboratory findings but there is no criterion available at the moment for early identification of the disease. The 1997 American college of Rheumatology (ACR) criteria [3] and its complimentary criteria; the 2012 systemic lupus international collaborating clinic (SLICC) criteria [5] are designed for classification of SLE but not for the diagnosis. The 2012 SLICC criteria is very complex and it can be used when the ACR criteria cannot classify SLE.
SLE is still a disease with significant morbidity and mortality. More recent studies have shown that latest 5 year survival is now nearer 90- 95% and that 70-85% patients have 10 year survival [6]. In most studies, patient with renal involvement had poor prognosis compared to patient without it.
CRP usually parallels disease activity in inflammatory conditions as it is an acute phase reactant produced by liver. But SLE is an exception. Patient with active SLE display only modestly elevated or even normal CRP level despite active disease. Marked elevation of CRP in SLE patients indicates infection and serositis [7]. Our patient also had modestly elevated CRP during the admission; this may be due to co-existing infection in this patient as she did not have clinical features of serositis.
Our patient had developed a rare neuropsychiatric complication called posterior reversible leucoencephalopathy syndrome (PRES). It usually present with rapid onset symptoms consisting of headache, seizures, altered consciousness and visual disturbance. It is strongly associated with diseases that co-exist in patient with renal diseases such as Hypertension, autoimmune and vascular diseases, exposure to immunosuppressive drugs such as cyclophosphamide and cyclosporine, and organ transplantation [8]. It should be considered in any patient who develops rapid neurological symptoms in the background of any renal disease.
Steroids such as Prednisolone have dual therapeutic actions in SLE. It has both anti-inflammatory and immunosuppressive actions. It is usually used to treat major organ complications such lupus nephritis and cerebral lupus. Steroid sparing other immunosuppressive agents such as Azathioprine, cyclophosphamide and mycophenolate mofetil should be considered if it is used for long term. When the required daily dose of Prednisolone exceeds 60 mg/day, Intravenous route in the form of Methylprednisolone pulse therapy (30 mg/Kg, maximum 1 g/day) should be used. Hydroxychloroquine (HCQ) 200-400 mg/day protects against the disease flare and used to treat dermatological and joint manifestations of SLE.
There are no clinical trials evaluated the management of PRES at the moment. But removal of the predisposing conditions including aggressive blood pressure management, withdrawing of the offending drugs or delivery in eclampsia fastens the recovery and prevents complications [8].
In conclusion, this patient initially presented with pyrexia of unknown origin complicated with renal impairment and cerebral involvement despite seronegativity, she was diagnosed as SLE [9]. If patient fulfil criteria for SLE despite seronegativity, diagnosis should not be delayed as 5-10% of SLE patient are seronegative.
References
- Man BL, Mok CC. Serositis related to systemic lupus erythematosus prevalence and outcome. Lupus. 14(10), 822–826 (2005).
- Koller SR, Johnston CL Jr, Moncure CW. Lupus erythematosus cell preparation-antinuclear factor incongruity. A review of diagnostic tests for systemic lupus erythematosus. Am. J. Clin. Pathol. 66(3), 495–505 (1976).
- Hochberg MC. Updating the American College of Rheumatology of revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 40(9), 1725 (1997).
- Berden JHM. Lupus nephritis. Kidney Int. 52, 538–558 (1997).
- Petri M, Orbai AM, Alarcons GS et al. Derivation and validation of the systemic lupus international clinic collaborating criteria for systemic lupus erythematosus. Arthritis Rheum. 64(8), 2677–2686 (2012).
- Trager J, Ward MM. Mortality and causes of death in systematic lupus erythematosus. Curr. Opin. Rheumatol. 13(5), 345–351 (2001).
- Honig S, Gorevic P, Weisssmann G. C-reactive protein in systemic lupus erythematous. Arthritis Rheum. 20(5), 1065–1070 (1977).
- Fugate JE, Claassen DO, Cloft HJ et al. Posterior reversible encepahalopathy syndrome: associated clinical and radiological findings. Mayo. Clin. Proc. 85(5), 427–432 (2010).
- Tsakonas E, Joseph L, Esdalie JM et al. A long term study of hydroxychloroquine withdrawal on exacerbations in systemic lupus erythematosus. The Canadian Hydroxychloroquine study Group. Lupus 7(2), 80–85 (1997).