Mini Review - Archives of Nursing and Care (2022) Volume 5, Issue 7
A Systematic Review: Prognostic value of severity indicators and Predictors of Mortality for Nursing Home-Acquired Pneumonia elderly patients
Mark Danial*
Carolina Population Center, University of North Carolina at Chapel Hill, 104 CPC South, Chapel Hill, NC 27516, USA
Carolina Population Center, University of North Carolina at Chapel Hill, 104 CPC South, Chapel Hill, NC 27516, USA
E-mail: markdanial@unisa.edu.au
Received: 02- August 2022, Manuscript No. oanc-22-73608; Editor assigned: 04- August -2022, PreQC No. oanc-22-73608 (PQ); Reviewed: 18-August-2022, QC No. oanc-22-73608; Revised: 23-August -2022, Manuscript No. oanc-22-73608 (R); Published: 30-August-2022 DOI: 10.37532/oanc.2022.5(7).75-78
Abstract
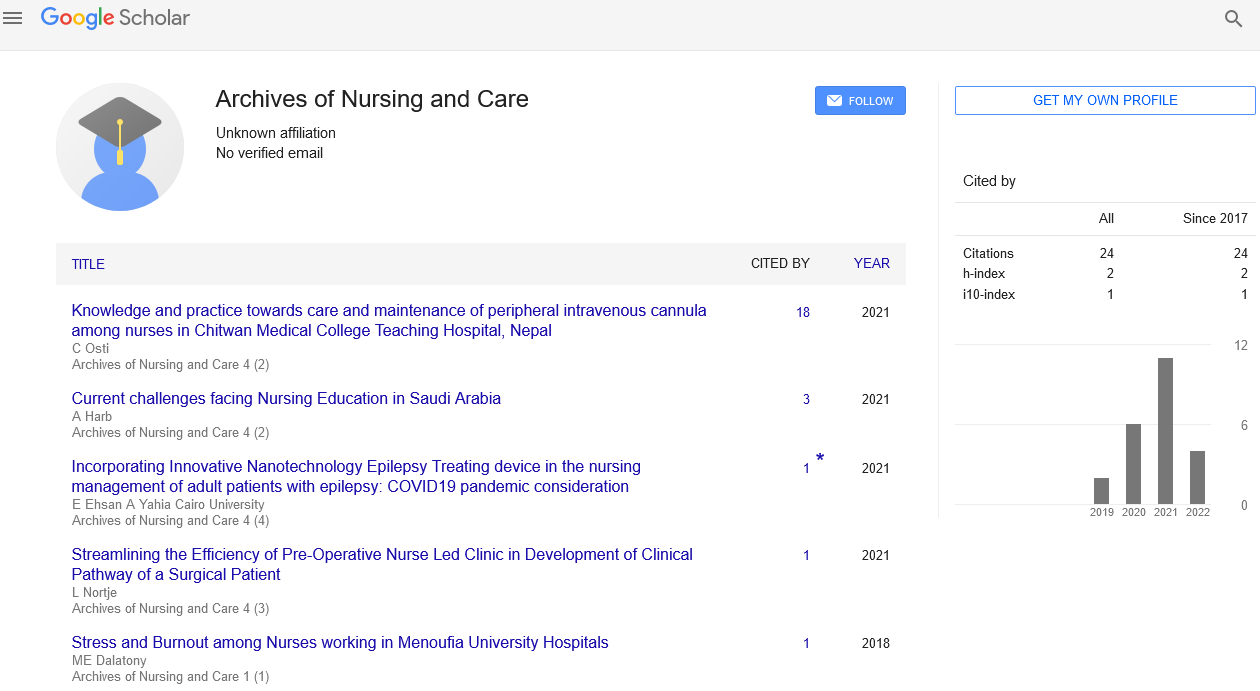
Current risk stratification tools, primarily used for CAP, are suboptimal in predicting nursing home acquired pneumonia (NHAP) outcome and mortality. We conducted a systematic review to evaluate current evidence on the usefulness of proposed predictors of NHAP mortality. PubMed (MEDLINE), EMBASE, and CINAHL databases were searched for articles published in English between January 1978 and January 2014. The literature search elicited a total of 666 references; 580 were excluded and 20 articles met the inclusion criteria for the final analysis. More studies supported the Pneumonia Severity Index (PSI) as a superior predictor of NHAP severity. Fewer studies suggested CURB-65 and SOAR (especially for the need of ICU care) as useful predictors for NHAP mortality. There is weak evidence for biomarkers like C-reactive protein and copeptin as prognostic tools. The evidence supports the use of PSI as the best available indicator while CURB-65 may be an alternative prognostic indicator for NHAP mortality. Overall, due to the paucity of information, biomarkers may not be as effective in this role. Larger prospective studies are needed to establish the most effective predictor(s) or combination scheme to help clinicians in decision-making related to NHAP mortality
Keywords
Radiography • Clinical • Copeptin • Gram-negative
Introduction
The rate of growth in the elderly population around the world has led to the estimate that 40% of adults around the world will reside in a long-term care (LTC) facility for some time before death, over the next 30 years. Nursing home-acquired pneumonia (NHAP) is currently the second most common type of infection among patients in LTC facilities in the USA. NHAP is also responsible for a majority of emergency department transfers [1]. Several patient characteristics predispose nursing home patients to pneumonia, including chronic diseases, impaired functional abilities, malnourishment, diminished cough reflex, lack of elastic tissue, and decreased immunoglobulin A. Additionally, attributes of the nursing home setting including the lack of immunizations, presence of multi-drug-resistant organisms, and widespread use of antibiotics also contribute to a greater risk of pneumonia. Thus, pneumonia represents 13–48% of all infections in nursing home settings [2]. Importantly, NHAP has the highest rates of morbidity and mortality among all the infections that occur in nursing homes, with rates of mortality reported to reach 55%. In some countries such as South Korea, NHAP is the leading cause of mortality in long-term residents. The incidence of pneumonia is estimated to be 10 times greater in nursing homes compared to individuals living in the community. The hospitalization rates of NHAP, however, are estimated to be almost 30 times that of CAP [3]. The significance of NHAP mortality is illustrated by the fact that NHAP mortality rates are higher than those related to community-acquired pneumonia (CAP), ranging from 5 to 40% according to some accounts. While traditionally the excess mortality of NHAP was thought to be due to multi-drug-resistant (MDR) organisms, current research has pointed to the presence of comorbidities in the nursing home setting as a major reason for the higher mortality than CAP. An important issue that has been raised is whether it is necessary to hospitalize all NHAP patients. There is a clear need for a clinical tool that can predict mortality and functional deterioration due to hospitalization in NHAP patients. Such a tool would enhance patient outcomes and enable better allocation of healthcare resources. Additionally, a predictive tool may influence decisions for ICU admission for NHAP patients presenting to the emergency department setting. This systematic review sought to explore the current literature on NHAP risk stratification and specific predictors for disease severity that may serve as a clinical judgment tool for clinicians and inform decisions of prioritizing care, hospitalization, ICU admissions, and administering prophylactic antibiotics.
Preface of the Book
The literature search elicited a total of 666 references, from which 491 were duplicates and another 89 were excluded [4]. A total of 86 articles were reviewed in full text; 20 articles met the inclusion criteria for the current systematic review.
A literature search utilized several databases: PubMed, EMBASE, and CINAHL. Studies were selected based on preset inclusion and exclusion criteria. Systematic search was restricted to studies including humans and published in English, from January 1978 to January 2014. An experienced librarian in electronic search methods performed the literature search. The search strategy and keywords employed in this study are summarized.
Study Selection and Data Collection Process. All abstracts were read and articles of potential interest were reviewed in detail by authors Michael Khalili and Naveen Dhawan to decide on inclusion or exclusion from this systematic review [5]. In cases of disagreement, both authors reviewed and discussed the study and a final decision was made through consensus. The authors investigated NHAP with the goal of identifying predictors of mortality from this disease. The study methodology conformed to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement for systematic reviews.
Discussion
NHAP naturally affects the ancient patient population that has multiple comorbidities. Several inquests that have probed NHAP in attended cases show mean times to be 74 – 82 generations, while the 30- day mortality is reported to range from16.8 to24.7. The youngish subject group( lower than 65 times of age) showed two times lower mortality than those 65 or over. Importantly, Klapdor etal. showed that patient age was a significant determinant in donation and prognostic of NHAP cases. In old cases, typical symptoms of pneumonia matching as slaver thing, cough, and fever are constantly absent. They also start that the immature cases altogether presented with fever. Importantly, roughly two- thirds of those with NHAP display temperatures over100.4 degrees Fahrenheit; nursing home cases have lower genesis temperatures and lower peak temperatures behaving from infection. The opinion of pneumonia is frequently complicated due to delayed recognition stemming from preexisting and habitual conditions and comorbidities( i.e., stroke and madness); hence, there's a evolved rate of mortality in ancient cases. Further, it has been shown that the prognostic for NHAP is worse for men than women [6].
| Statistical Procedure (n = 1025) | Finding |
| Comparative Fit Index (CFI) | 0.932 |
| Standardized Root Mean Square (SRMR) | 0.048 |
| Cronbach’s Alpha Reliability Coefficients: | |
| NCAT Total Score | 0.94 |
| NCAT Subscale Scores: | |
| Expectations | 0.85 |
| Behaviors | 0.71 |
| Teamwork | 0.91 |
| Communication | 0.79 |
| Satisfaction | 0.82 |
| Professional Commitment | 0.91 |
Table 1. The Nursing Culture Assessment Tool’s (NCAT) Comparative Fit Index, Standardized Root Mean Square, and Reliability Estimates
The microbial infective etiology of NHAP remains controversial [7]. A particular challenge in determining microbial etiology lies in obtaining adequate sputum samples, since only as estimated 50–70% of nursing home patients are unable to produce decent sputum samples. While antigen testing of respiratory secretions is useful in diagnosing viruses such as RSV and influenza, urinary antigen testing for Legionella pneumophila serotype 1 and Streptococcus pneumonia remains challenging due to limited knowledge regarding the susceptibility to antibiotics [8]. The infective agents in NHAP also vary throughout the world. For instance, in a recent prospective cohort study of 488 nursing home resident patients hospitalized for pneumonia, over half (55.9%) of NHAP cases were due to a viral infection [9]. Yet, in a recent prospective study of 217 nursing home residents, 56.3% of NHAP cases were due to Enterobacteriaceae. In the USA, NHAP most commonly stems from bacteria yet the specific cause is often unknown.While Streptococcus pneumoniae has been identified as the most common infective agent, in more severe NHAP resulting in hospitalization Staphylococcus aureus and the enteric Gram-negative agents appear more commonly than Streptococcus pneumonia. In a recent study, Staphylococcus aureus was reported to account for the highest mortality. According to one study, Staphylococcus spp. were the most common agent in the USA comprising 52% of cases, while Streptococcus pneumoniae was the most prominent in Europe and Latin America (it was found in 46% of cases in Europe and 25% in Latin America). The large presence of multi-drug-resistant agents in NHAP patients in the USA has been documented. Typical bacterial agents in NHAP in the USA include Staphylococcus aureus, Pseudomonas, Klebsiella, Proteus mirabilis, and E coli. Typical community-acquired organisms that cause pneumonia include Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma, Legionella, and Chlamydia. The antibiotics used in CAP include azithromycin, macrolides, fluoroquinolones (i.e., levofloxacin), and a combination of a beta-lactam and a cephalosporin. Common causative organisms of NHAP in the USA[10]. The infective etiology differs, however, in countries such as Poland. In a recent prospective study of 217 patients age 65 or above, 56.3% of microorganisms are comprised of Enterobacteriaceae, 25% Pseudomonas aeruginosa, and Staphylococcus aureus 12.5%, and Candida albicans is comprised of 6.3%. Thus, NHAP and CAP share many features in their microbial infective etiology including the emergence of drug resistant bacteria. Ma et al. suggested that NHAP should not be treated as healthcare-associated pneumonia instead of community-acquired pneumonia (CAP). The researchers found that, in both NHAP and CAP, multi-drug-resistant bacteria were not common. Importantly, NHAP can also be caused by a viral etiology. Respiratory syncytial virus (RSV) and influenza remain the most common sources of respiratory disease and fatality in nursing homes.
Conclusion
Our study showed that the current evidence points to PSI as having superior predictive value compared to other clinical tools in determining NHAP mortality, with CURB-65 also validated as another very useful tool. The next best tool supported by evidence is SOAR, which may have particular benefit in identifying patients in need of ICU admissions. The evidence in support of biomarkers for predicting NHAP mortality is not completely conclusive, but CRP appears to be the biomarker with the most concrete support. Additionally, copeptin may serve as a reliable predictor of 30-day mortality in NHAP, but more studies are needed to validate its effects and use. No single set of clinical characteristics, prognostic scoring tools, or biomarkers have overwhelming support in their use with NHAP; further prospective studies are warranted in large samples that can delineate the most effective predictor or combination scheme of predictors to ultimately aid clinicians in determining relative likelihood of NHAP mortality.
Conflict of Interest
The authors report no conflict of interest.
References
- Mintz AH, Kestle J, Rathbone MP et al. A randomized trial to assess the efficacy of surgery in addition to radiotherapy in patients with a single brain metastasis. Cancer.78, 1470–1476(1996).
- Zimm S, Wampler GL, Stablein D et al. Intracerebral metastases in solid-tumor patients: natural history and results of treatment. Cancer .48,384–394(1981).
- Grunfeld E, Coyle D, Whelan T et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ .170, 1795–1801(2004).
- Brouwers MC, Chambers A, Perry J et al Neuro-oncology Disease Site Group. Can surveying practitioners about their practices help identify priority clinical practice guideline topics? BMC Health Serv Res. 3, 23-25(2003).
- Lee ST, Lui TN, Chang CN et al. Prophylactic anticonvulsants for prevention of immediate and early postcraniotomy seizures. Surg Neurol .3, 361–364(1989).
- Kraneiukaite D, Rastenyte D, Jureniene K et al. Persirgusiųjų galvos smegenų insultu gyvenimo kokybe. (Quality of life in stroke survivors.) Medicina (Kaunas). 43,736-745(2007).
- Lederer W, Feichtner A, Medicus E et al The palliative treatment plan as basis for informed decisions in palliative or emergency care. Wien Med Wochenschr. 161, 543–547(2011).
- Detering KM, Hancock AD, Reade MC et al. The impact of advanced care planning on end of life care in elderly patients: Randomised controlled trial. BMJ. (2010).
- Sulmasy DP, Terry PB, Weisman CS et al. The accuracy of substituted judgments in patients with terminal diagnoses. Ann Intern Med.128, 621–629(1998).
- Rodríguez Molinero A, López Diéguez M, Tabuenca AI et al. Physicians’ impression on the elders’ functionality influences decision making for emergency care. Am J Emerg Med. 28, 757–765(2010).
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref