Case Report - Clinical Practice (2023) Volume 20, Issue 3
When Not All Swellings Are Mucoceles: A Case of Lip Lymphangioma in the Maxillofacial Region
- Corresponding Author:
- Geetha Sridharan
Department of Oral and Maxillofacial surgery, Meenakshi Ammal Dental College and Hospital, Chennai, Tamil Nadu, India
E-mail: drgeethaomfs@gmail.com
Received: 12 July, 2023, Manuscript No. fmcp-23-105831 Editor assigned: 13 July, 2023, PreQC No. fmcp-23-105831 (PQ), Reviewed: 17 July, 2023, QC No. fmcp-23-105831 (Q), Revised: 22 July, 2023, Manuscript No. fmcp-23-105831 (R), Published: 28 July, 2023, DOI. 10.37532/2044-9046.2023.20(3).
Abstract
Lymphangiomas are tumour- like benign, developmental hamartomatous malformations of the lymphatic system which is distinguished by abnormal proliferation of lymphatic vessels. It was first reported by Virchow in 1854. In this article we report a unique case of lymphangioma of the lower lip of a 11-year-old patient who is under orthodontic treatment. A detailed history and clinical evaluation, and histopathology confirmed the diagnosis of lymphangioma.
Keywords
lymphatic malformation, lip, mucocele, oral lymphangiomas
Introduction
Vascular malformations were first described by Redenbacher in the year 1828. Few refer lymphangiomas as hamartomas and other lesions as congenital malformations. Intemperate secretion from the cell lining causes obstruction of lymphatics leading to slow-growing, asymptomatic, pain-free cystic mass causing acute facial abnormality. These conditions are more often predominant during the time of birth or at infancy (50%) and other vascular tumours in children constitute about (25%), which has more female predilection compared to male [1,2].
These are commonly evident in head and neck region about (50%-70%) but they are sparse entity in oral cavity region [3,4]. Frequent sites of occurrence in the oral region are the tongue (dorsum and lateral border), palate, cheeks, floor of the mouth, gingiva and the lips. Other differential hamartomatous lesions are haemangiomas, odontomas, and cherubism etc [3,5].
Case Report
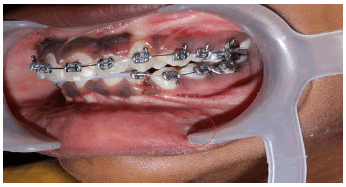
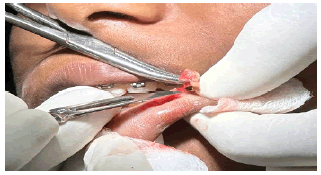
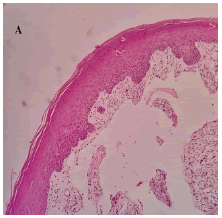
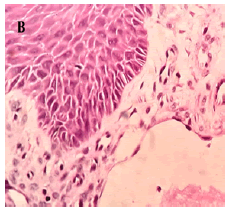
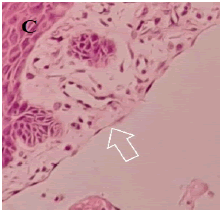
A 11-year, female patient accompanied by parents, reported to our institution with a chief complaint of small swelling on lower lip for 1 year. Upon history of present illness, she was apparently alright a year back when they noticed a small pea size soft and compressible swelling on the lower lip which regresses upon compression with no associated pain. Small pea size swelling resolved on its own 6 months back. Recently 2 months back they again noticed same pea size swelling in the same region which is not associated with pain and not regressing upon compression. Patient was under orthodontic treatment since a year. On local clinical examination, small pea size vermillion colour nodule, non-tender and non-compressible is present on lower lip. Provisionally diagnosed as mucocele of lower lip of size approximately 3 mm × 3 mm (FIGURE 1). Treatment done was excision under local anaesthesia and histopathological examination done upon which final diagnosis came up as lymphangioma of lower lip (FIGURE 2).Upon histopathological examination of the excised specimen, H&E-stained soft tissue section showed dilated lymphatic channels submucosally, lined by widely spaced flattened endothelial cell nuclei and lumen with foci of granulation tissue formation with inflammatory component. The` adjacent area showed a lobule of mucous salivary acini (FIGURE 3.A-3.C). Patient follow up done up to 3 months which showed remarkable healing and no recurrence (FIGURE 4).
Discussion
Lymphangiomas emerge from the segregate of primordial lymphatic cell channels which insistently store lymph but stall to join the larger vessels, leading to lymphatic blockage, thus showcasing a cystic appearance which exhibits a miscellaneous pattern in defining lymphangiomas. In paediatric population lymphangiomas prevails with an incidence of about 1in 16000 live births and are ascribed to about 6-11% of benign maxillofacial tumours [6]. There are two major entities: Acquired lymphangiomas and Congenital lymphangiomas, whereas the other factors like prolonged history of trauma, blockage of lymph vessels due to infection, inflammation, radiotherapy, or surgery are inclined towards acquired lymphangiomas and lymphangiomas associated with haemangiomas,definite chromosomal aberrations like Noo-nan syndrome, Turners syndrome, Down syndrome, Foetal alcohol syndrome, Cardiac anomalies and foetal hydrops are the predisposing factors for congenital lymphangioma [7]. Various rationales have been proposed for the pathogenesis of lymphangiomas. Etiopathogenesis of lymphangioma is depicted in TABLE 1.
TABLE 1. Rationales for pathogenesis of the lymphangioma
| Rationale I | Congenital Lymphangiomas result from sequestration of primordial lymphatics |
|---|---|
| Rationale II | The failure of the lymphatic vessels to drain into the veins causes lymph accumulation and leads to the formation of large cyst-like dilated lymphatics |
| Rationale III | Lymphangiomas may develop through aberrant budding of the lymphatic vessels, thus establishing new anomalous divisions. |
| Rationale IV | Long-standing inflammation may evoke lesion development by triggering the proliferation of lymphatic channels |
| Rationale V | Increased expression of vascular endothelial growth factor-C (VEGF-C) and vascular endothelial growth factor R3 |
Histopathologically, lymphangiomas are characterized by the presence of dilated lymphatic vessels and cysts, lined by flattened endothelial cells, and separated by fibrous septae containing lymphoid aggregates and lymphoid follicles. The cysts are usually filled with a clear lymphatic fluid, which is rich in lymphocytes, macrophages, and plasma cells [5,6]. In the case of lymphangioma of the lip, the histopathological examination would reveal similar findings. The excised specimen would show dilated lymphatic channels submucosally, lined by widely spaced flattened endothelial cell nuclei and lumen with foci of granulation tissue formation with inflammatory component. The adjacent area may show a lobule of mucous salivary acini, but these would be separated from the lymphatic cysts by fibrous septae.
It is important to differentiate lymphangiomas from other cystic lesions, such as mucoceles, as the treatment approach differs [8,9]. Lymphangiomas lack a universally standardized classification; typically, they are categorized into superficial and deep lymphangiomas based on the size and depth of the abnormal lymphatic channels (TABLE 2). Even tumours that appear well-defined clinically do not exhibit encapsulation. In deeper lesions, vessels are observed scattered amidst adipocytes and striated muscle bundles. Lymphangiomas can be subclassified into four types (TABLE 3).
TABLE 2. Clinical classification of lymphangioma
| Type I | Superficial Multicystic type |
|---|---|
| Type II | Deep cavernous type |
| Type III | Cystic Hygroma |
TABLE 3. Histopathological classification of Lymphangioma
| Lymphangioma Simplex | Composed of small, thin-walled lymphatics |
|---|---|
| Cavernous lymphangioma | Comprised of dilated lymphatic vessels with surrounding adventitia |
| Cystic lymphangioma | Consisting of huge macroscopic lymphatic spaces with surrounding fibrovascular tissues and smooth muscle |
| Benign lymphangioendothelioma | Lymphatic channels appear to be dissecting through dense collagenic bundles |
These categories are relatively arbitrary, and numerous lesions exhibit a combination of characteristics from multiple categories [10].
Lesions in the oral cavity may include haemangioma, lingual thyroid, thyroglossal duct cyst, granular cell tumour and cheilitis. Granulomatosis, mucocele/ranula, and cellulitis are all possibilities for differential diagnosis [6,11]. Mucoceles, on the other hand, are common benign lesions that arise from minor salivary glands and are filled with mucin. They typically present as soft, compressible, painless swellings that fluctuate in size and can appear bluish or translucent. Mucoceles are often associated with trauma or injury to the affected area [12,13].
Lymphangiomas are usually diagnosed according to their clinical presentation and corelated with the histopathological report and diagnostic radiographic study which expedite by affirming the diagnosis. The shape, size, site and margins of the lesion are assessed with Ultrasonography (USG) which is a requisite to check whether the lesion is multicystic or unicystic with internal septaes. Ultrasound with colour-flow Doppler aids in identifying the component of the lesion, whereas angiography helps not only to avert the vascular lesions but also to differentiate the entities [14,15]. Nevertheless, Computed tomography and magnetic resonance imaging is indisputable to ultrasonography in identifying the adjacent structures and a delineation of the extent of the lesion [14].
Restoring the functions and preventing any potential problems should be the main goals of the therapeutic techniques. Though there are plethora of treatment options for management of lymphangiomas like laser therapy (carbon-dioxide laser and Nd:YAG, cryotherapy, sclerotherapy (25% Dextrose, hypertonic saline, bleomycin, picibanil (OK-432) [15, 16] , Sodium Tetradecyl Sulphate (STS), ethanol, and corticosteroid [15], electrocautery, intralesional steroids, interferon alpha, therapeutic embolization and ligation, Flashlamp Pulsed Dye Laser (FPDL), radiotherapy but the substantiated treatment is surgical excision of the lesion [16-18].
One such advancement is the use of laser therapy in the treatment of lymphangiomas. Lasers have been shown to be effective in the treatment of vascular malformations, including lymphangiomas, by selectively destroying the abnormal blood vessels while sparing the surrounding normal tissue. Several studies have reported successful outcomes in the treatment of lip lymphangiomas using various types of lasers, including carbon dioxide (CO2 ) laser, neodymium-doped yttrium aluminium garnet (Nd: YAG) laser, and Pulsed Dye Laser (PDL) [18,19].
Based on our case, it is crucial to emphasize that even for lesions displaying typical clinical characteristics, it is essential to conduct additional clinical investigations and complementary examinations, such as biopsy and histopathological analysis, to confirm the diagnosis accurately and determine the appropriate treatment approach.
Conclusion
In conclusion, lymphangiomas should be considered in the differential diagnosis of maxillofacial lesions presenting with clinical features similar to mucoceles. A thorough clinical and histopathological evaluation is essential for accurate diagnosis and appropriate management. Dental professionals should be aware of the clinical and histopathological features of lymphangiomas to avoid misdiagnosis and ensure optimal patient care.
Ethical Approval
Not applicable
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Acknowledgement
Nil
Funding
Nil
Consent to Publish
Written consent to publish was obtained for publication of the patient’s identifiable information.
References
- Mechery R, Kumar M, Arora P, et al. Lymphangioma of lip treated with carbon dioxide laser. J. Dent. Lasers. 10(2), 81(2016).
- de Carvalho FK, Pinheiro TN, da Silva RA, et al. Lymphangioma of the lower lip mimicking a mucocele in children. J. Dent. Child. 82(2),116-9(2015).
[Google Scholar] [Cross ref]
- Bhayya H, Pavani D, Tejasvi MA, et al. Oral lymphangioma: A rare case report. Contemp. clin. dent. 6(4),584(2015).
- Pinto A, Haberland CM, Baker S. Pediatric soft tissue oral lesions. Dent. Clin. 58(2),437-53(2014).
- Sunil S, Gopakumar D, Sreenivasan BS. Oral lymphangioma–Case reports and review of literature. Contemp. clin. dent. 3(1),116(2012).
- Hasan S, Ahmad SA, Kaur M, et al. Lymphangioma of the Lower Lip—A Diagnostic Dilemma: Report of a Rare Case with a Brief Literature Review. Case Rep. Dent., 2,(2022).
- El Hag OA, Ali EA, Osman MA. Clinical profile of lymphatic malformation from one oral and maxillofacial center in Sudan. Open J. Stomatol. 7(8),345-52(2017).
- Neville BW, Damm DD, Allen CM, et al. Oral and maxillofacial pathology. Elsevier Health Sci.; (2015).
[Google Scholar] [Cross ref]
- Das S, Tripathy PK, Panda S, et al. Lymphangioma of lip mimicking mucocele in maxillofacial region - a case report with a review of literature. J Oral Maxillofac. Pathol. S97-S101(2021).
- Sivapathasundharam B, Rajendran A. Shafer's textbook of oral pathology. Elsevier Health Sci.; (2012).
[Google Scholar] [Cross ref]
- Bhayya H, Pavani D, Tejasvi MA, et al. Oral lymphangioma: A rare case report. Contemp. clin. dent. 6(4),584(2015).
- Bindhu PR, Mathew J, Thomas P, et al. Cavernous lymphangioma of lower lip. Health Sci. 2:1-7(2013).
[Google Scholar] [Cross ref]
- Chaitanya P, Praveen D, Reddy M. Mucocele on lower lip: A case series. Indian dermatol. online j. 8(3),205(2017).
- Hasan S, Ahmad SA, Kaur M, et al. Lymphangioma of the Lower Lip—A Diagnostic Dilemma: Report of a Rare Case with a Brief Literature Review. Case Rep. Dent. 2,(2022).
- Rhee SH, Lee JH, Kim HS, et al. Application of laser in oral surgery. J. lasers med. sci.5(3),97(2014).
[Google Scholar] [Cross ref]
- Haidry N, Shivhare P, Vaidyanathan A, et al. Lymphangioma of the Oral and Maxillofacial Region: A Report of Three Cases. Cureus. 14(12), 2022.
- Matharu J, Patel V. Cryotherapy for the management of a lip lymphangioma–a case report and literature review. Oral Surg. 12(3),230-7(2019).
- Zhang J, Wu Y, Wu J, et al. Application of laser in oral surgery. 5(3):97(2014). J Oral Maxillofac Surg., 72,1094-1098(2014).
[Google Scholar] [Cross ref]
- Lai CH, Hanson SG, Mallory SB. Lymphangioma circumscriptum treated with pulsed dye laser. Pediatr. dermatol. 18(6),509-10(2001).