Editorial - Interventional Cardiology (2015) Volume 7, Issue 2
Use of the Baylis radiofrequency trans-septal needle to create an atrial communication in hypoplastic left heart syndrome
- Corresponding Author:
- Alejandro J Torres
Division of Pediatric Cardiology, Children’s Hospital of New York-Presbyterian
Columbia University Medical Center, New York, NY, USA
E-mail: at2109@cumc.columbia.edu
Abstract
Keywords
Atrial septostomy, congenital heart disease, hypoplastic left heart syndrome, radiofrequency perforation, transcatheter therapy, trans-septal puncture
Intact or restrictive atrial septum (RS) is identified in about 6% of newborns with hypoplastic left heart syndrome (HLHS). Although survival has improved in recent decades, mortality remains high, and immediate intervention to open the atrial septum is required to relieve pulmonary venous obstruction [1,2]. A variety of methods have been described to create an atrial communication, including surgical and hybrid procedures. However, a transcatheter approach remains the first line of treatment in most centers [3,4,5]. Perforation of the septum using radiofrequency (RF) energy with the Nykanen RF (NRF) wire and Baylis RF generator (Baylis Medical, Montreal, Canada), followed by static balloon septoplasty and/or stent placement, has become the most popular technique to create an adequate atrial communication in these patients [6,7]. The disadvantages of this technique include difficulty in properly positioning the RF catheter against the septum and the need for several catheter exchanges in order to achieve stable wire position across the atrial communication. The use of the Brockenbrough trans-septal needle for this purpose offers the advantage of being a stiffer system but carries a high-risk of left atrial free wall perforation. In this report, we present an alternate experience using the Baylis NRG™ RF (BRF) trans-septal needle (Baylis Medical) for atrial septal perforation in two patients with HLHS–RS.
Case 1
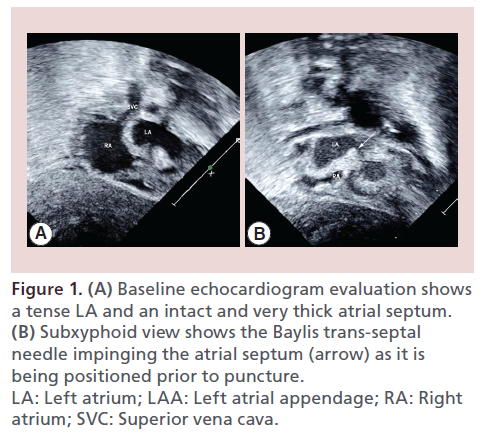
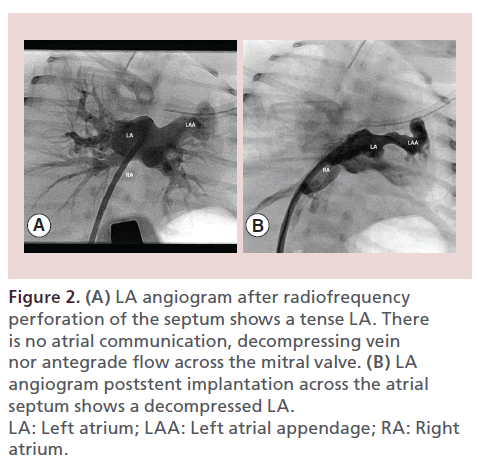
A 3.2-kg term neonate with prenatally diagnosed HLHS/intact atrial septum was transferred at 15 min of life to the catheterization laboratory. Apgar scores were 4 at both 1 and 5 min. The fetal echocardiogram had shown HLHS with severe mitral stenosis, aortic atresia and a thick, intact atrial septum with no evidence of a decompressing vein. Postnatal transthoracic echocardiogram confirmed the diagnosis (Figure 1A). Upon arrival to the catheterization laboratory, systemic O2 saturation was less than 40%. Femoral venous access was obtained. At 20 min of life, a venous blood gas showed a pH of 6.8 and a lactate of 8. Fluoroscopy showed complete whiteout of the lung fields. A 6-Fr, 64-cm trans-septal sheath (St. Jude Medical, MN, USA) with a 71-cm BRF needle was advanced into the right atrium (RA) and positioned against the atrial septum, which was confirmed by transthoracic echocardiography (Figure 1B). The BRF needle was connected via the side port to the pressure transducer, and via the connector cable to the Baylis RF generator (Baylis Medical). RF was applied at 5 W for 2 s and the needle easily perforated into the left atrium (LA). Mean LA pressure was 29 mmHg. The dilator of the trans-septal sheath was then advanced over the needle into the LA. An angiogram showed a tense LA with no evidence of atrial communication or decompressing vein (Figure 2A). The internal diameter of the trans-septal sheath dilator is 0.032″. Therefore, the tip of a 0.032″ J wire (Cook Medical, IN, USA) was curled into the LA, but the dilator and the wire prolapsed back into the RA as we attempted to advance the sheath, over the dilator, through the very thick septum. On echo, only a trivial residual communication was noted despite the fact that the sheath dilator had been across the septum. The BRF needle was repositioned, and the septum was easily crossed again using the same RF settings. We were then able to advance the dilator and the sheath into the LA. The dilator was removed and a 0.035″ Rosen wire (Cook Medical) was positioned in the large atrial appendage. An 8-mm premounted Genesis PG1880 stent (Cordis, NJ, USA) was advanced to the tip of the trans-septal sheath. The sheath was retracted and the stent was successfully dilated straddling the septum, resulting in an immediate improvement in the systemic saturation up to 93% (Figure 2B). Repeat hemodynamics showed a mean LA pressure of 9 mmHg, with a nonrestrictive atrial communication. The patient remained hemodynamically stable and underwent Norwood/ Sano procedure at 1 week of life.
Figure 1: (A) Baseline echocardiogram evaluation shows a tense LA and an intact and very thick atrial septum. (B) Subxyphoid view shows the Baylis trans-septal needle impinging the atrial septum (arrow) as it is being positioned prior to puncture. LA: Left atrium; LAA: Left atrial appendage; RA: Right atrium; SVC: Superior vena cava.
Figure 2: (A) LA angiogram after radiofrequency perforation of the septum shows a tense LA. There is no atrial communication, decompressing vein nor antegrade flow across the mitral valve. (B) LA angiogram poststent implantation across the atrial septum shows a decompressed LA. LA: Left atrium; LAA: Left atrial appendage; RA: Right atrium.
Case 2
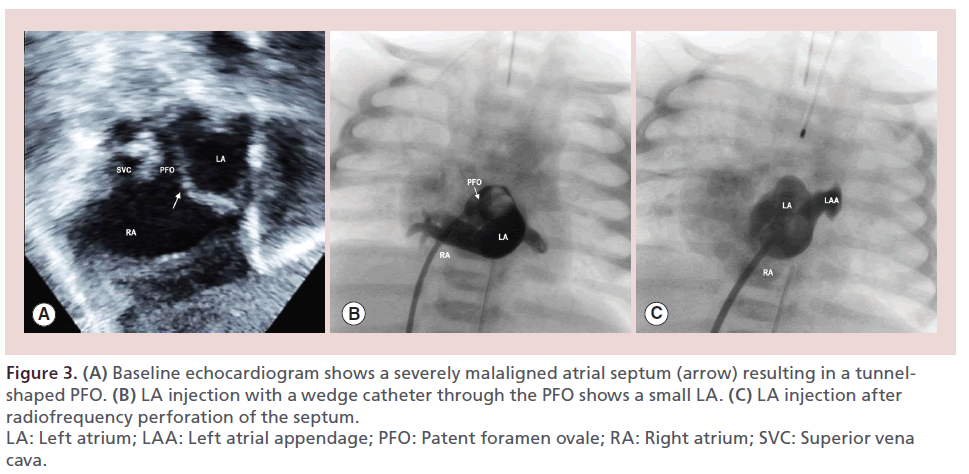
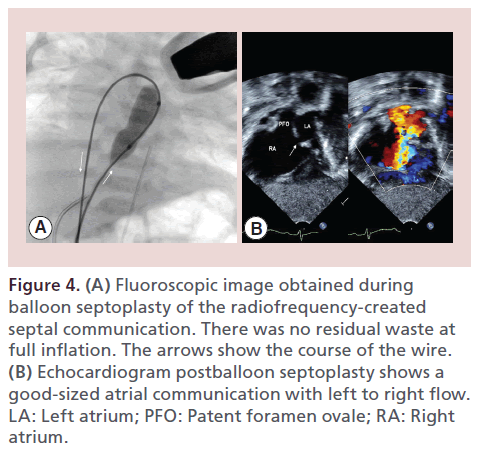
A 3.6-kg neonate with prenatally diagnosed HLHS and high likelihood of RS was transferred to the catheterization laboratory at 90 min of life for left atrial decompression. Delivery was via elective caesarean section. Apgar scores were 8 at both 1 and 5 min. Although the patient initially seemed stable, at 30 min of life he became progressively more tachypneic with respiratory rates of 70–80/min and with systemic saturation falling to the high 70s to low 80s. Chest x-ray showed increased pulmonary vascular markings. Echocardiogram confirmed the diagnosis of HLHS and showed a severely malaligned septum primum, with typical creation of a long, restrictive patent foramen ovale (PFO) tunnel exiting at the roof of the LA with a mean Doppler gradient of 15 mmHg (Figure 3A). As the patient’s hemodynamic condition was deteriorating, the decision was made to decompress the LA. Traditional balloon septostomy, static balloon angioplasty or stent implantation of long tunnel PFO due to a malaligned septum primum are usually ineffective. Therefore, creation of an additional atrial communication was indicated. In the catheterization laboratory, the patient was intubated and a 5-Fr sheath was placed in the right femoral vein (RFV). A 5-Fr wedge catheter was advanced through the PFO into the LA. LA mean pressure was 27 mmHg, with a simultaneous RA mean pressure of 3 mmHg. Angiography showed a somewhat small LA (Figure 3B). The 5-Fr short sheath was exchanged for a 6-Fr, 64-cm conventional trans-septal sheath. A 71-cm BRF needle was introduced into the sheath and the entire system was positioned in the RA. The BRF needle was connected to the pressure transducer and Baylis RF generator. Under echocardiographic and fluoroscopic guidance, the system was maneuvered until the midportion of the septum was clearly ‘tented’ on transthoracic echo. RF energy was delivered at 5 W for 2 s. The needle was seen crossing the septum by echo, which was confirmed by a change in the waveform tracing and pressure. The dilator was easily advanced over the needle into the LA (Figure 3C). The BRF needle was removed and the curled tip of a 0.032″ J wire was looped in the LA. As the dilator was removed, echocardiogram showed the wire crossing a good-sized communication (2–3 mm) with left-toright shunting. As wire position was deemed suboptimal, a 4-Fr multipurpose catheter (Cordis Corporation) was easily advanced into the LA to improve wire position. Due to the orientation of the newly created communication, it was not possible to enter a pulmonary vein, despite multiple attempts with different wires. However, a 0.035″ Glide wire (Terumo Medical Corporation, NJ, USA) was easily advanced from the LA back through the PFO into the RA and then into the inferior vena cava (IVC), forming a loop. The Multipurpose catheter was exchanged for a 4-Fr, 65-cm angled Glide catheter (Terumo Medical Corporation, NJ, USA), which was advanced over the loop into the IVC. The Glide wire was exchanged for a 0.035″, 180 cm Rosen wire. Then a 10 mm × 2 cm OptaPro balloon (Cordis) was positioned straddling the newly created atrial communication. The balloon was inflated up to 10 ATM, with no residual waste noted at full inflation (Figure 4C). Hemodynamics obtained following balloon inflation demonstrated LA and RA mean pressures of 9 and 6 mmHg, respectively, which correlated with a mean Doppler gradient of 5 mmHg across the septal communication by echo (Figure 4). Despite the wide-open atrial communication, systemic saturation remained in the mid-80s for the first hour after the procedure and increased to the mid-90s within hours. The patient underwent an uneventful Norwood procedure at 4 days of life.
Figure 3: (A) Baseline echocardiogram shows a severely malaligned atrial septum (arrow) resulting in a tunnelshaped PFO. (B) LA injection with a wedge catheter through the PFO shows a small LA. (C) LA injection after radiofrequency perforation of the septum. LA: Left atrium; LAA: Left atrial appendage; PFO: Patent foramen ovale; RA: Right atrium; SVC: Superior vena cava.
Figure 4: (A) Fluoroscopic image obtained during balloon septoplasty of the radiofrequency-created septal communication. There was no residual waste at full inflation. The arrows show the course of the wire. (B) Echocardiogram postballoon septoplasty shows a good-sized atrial communication with left to right flow. LA: Left atrium; PFO: Patent foramen ovale; RA: Right atrium.
Discussion
Creation of an atrial communication in HLHS–RS patients is one of the most challenging procedures for interventional pediatric cardiologists. Different approaches have been utilized, including surgical atrial septostomy, early Norwood procedure, fetal balloon septoplasty and transcatheter septoplasty (blade or Brockenbrough trans-septal needle), all with variable results [4,5]. Extracardiac histotripsy may have a role in the future [8]. The use of the RF perforating system has become the most popular approach in most institutions, after several reports have described its advantages for this indication [6,7]. The procedure consists of advancing a stiff guiding catheter (usually a Judkins right curve) into the RA aiming toward the atrial septum. A coaxial injectable catheter (Baylis Medical) containing an NRF wire is advanced to the tip of the guiding catheter and positioned against the atrial septum. RF energy is delivered using the Baylis RF generator, which is usually set at 5 W for 2–5 s. Output and time can be increased if the perforation is unsuccessful. After the NRF wire is seen entering the LA, the coaxial catheter is advanced over the wire. The NRF wire is exchanged for a 0.014″ or 0.018″ wire, which is advanced into the LA or into a pulmonary vein. This is followed by serial dilations of the communication using cutting balloon ± regular balloon dilatation and/or stent implantation depending on operator preference.
We have encountered a number of difficulties and technical failures associated with this technique. In our experience, the RF wire has frequently failed to deliver energy or perforate the septum, despite increasing the energy output and delivery time. Other operators have reported similar difficulties [7], which are likely not related to malfunctioning NRF wires or generators but to technical problems including suboptimal contact with the septum by the NRF wire. In order to work properly, the tip of the NRF wire should be perpendicular to the plane of the atrial septum. This can be challenging in patients with HLHS–RS due to the pronounced convex shape of the septum due to the high LA pressure. If the NRF wire is not perpendicularly aligned, it tends to slide along the surface of the septum primum into the PFO, instead of perforating into the LA, as mild forward tension is exerted during RF delivery. Other less common sources of failure include creation of a track within the wall of the thick atrial septum in which the RF wire fails to completely perforate the septum in repeated RF applications, or formation of a clot around the tip of the wire, which may prevent RF energy from being delivered directly to the wall of the septum. Repositioning the guiding catheter and changing the NRF wire should correct these two situations. Once the coaxial catheter is advanced into the LA, the NRF wire is removed and a 0.014″ or 0.018″ wire is advanced through the coaxial catheter. Keeping the soft coaxial catheter in position, getting the wire into a pulmonary vein, or curling a significant portion within a small LA in order to have a firm segment of wire across the atrial septum is challenging. In addition, because the atrial septal defect created by the RF wire/coaxial catheter is very small, crossing the communication even with small balloons is often difficult and may require significant manipulation despite an acceptable wire position.
Using the BRF needle, as we described, overcomes some of these difficulties. The needle comes in different lengths (56, 71, 89 and 98 cm) and curves (C0 and C1, the 56 cm comes only with the C0 curve) similar to conventional trans-septal needles. The tip of the BRF needle has a radiopaque marker and two side holes, which allow for measuring pressure or injecting contrast through a side port to confirm position. However, it does not allow advancing a 0.014″ wire through it, as with the conventional trans-septal needle. The curve of the distal end of the needle can be straightened by hand, but we do not recommend doing this with the very distal tip of the needle, as it may damage the RF mechanism. Of note, the Baylis connector cable that connects the needle to the generator is different than the one used by the NRF wire. Maneuvering the BRF needle is similar to a conventional trans-septal needle. Because it is a stiffer and more steerable system than the NRF wire, positioning the needle at the desired area of the septum is done without difficulty, and tenting of the septum is easily seen on transthoracic echocardiogram. As RF energy is delivered, the needle usually slides into the LA with minimal forward force. Since a wire cannot be introduced into the needle, the dilator has to be advanced over the needle into the LA. Although this was easily achieved in our limited experience, even in the first patient with a very thick septum, we recognize this may potentially be challenging in some patients. Advancing the dilator into the LA can create a fair size communication, without needing to advance the sheath, which can allow subsequent advancement of a catheter or balloon over the wire into the LA. Alternatively, the defect can be dilated with a small diameter balloon to facilitate the advancement of the sheath. In our second patient, it was easy to cross the resulting defect with a multipurpose catheter. In this patient we were unable to achieve a stable wire position within the LA or pulmonary vein but were able to advance the wire back through the PFO into the RA and IVC, creating a very stable loop with a stiff wire, which facilitated advancing a balloon across the atrial septum.
Electrosurgical energy in combination with a conventional trans-septal needle has been reported to create an atrial communication in HLHS–RS [9]. In this report, a Brockenbrough needle was used in conjunction with an electrosurgical generator. An atrial communication was successfully created using 45 W (compared with the 5–10 W usually delivered by the Baylis generator). In addition to using less power, the Baylis system offers the advantage that it is readily available in most pediatric catheterization laboratories and most interventional cardiologists are familiar with its use. Thus, no investment in additional rarely used equipment is required. For those working in combined Adult–Pediatric Cath facilities, the Baylis equipment is a staple for adult trans-septal interventions including mitral valve interventions, and left atrial appendage closures.
Conclusion
This is the first report of the use of the BRF needle for the creation of an atrial communication in patients with HLHS–RS. The BRF needle is a viable option that overcomes some of the shortcomings of BRF wire system. It is a stiffer, more reliable system that is easier to maneuver and requires fewer catheter exchanges in order to achieve stable wire position across the atrial septum.
Future perspective
Neonatal mortality in patients with HLHS–RS remains elevated despite the significant medical and technological advances of the last decades. Different approaches have been described for the creation or enlargement of an atrial communication to decompress the LA. As of today, RF is the most common technique utilized for this purpose in most centers. Accurate prenatal identification of an RS and inventive use of newer technologies when performing the septostomy in the catheterization laboratory should lead to decreased presurgical morbidity and mortality and improved long-term outcome of this very high-risk subset of patients with HLHS. Prenatal static balloon septoplasty or stent implantation to decompress the LA in utero has been performed in some centers. More experience is necessary to determine the outcome of this intervention.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Informed consent disclosure
The authors state that they have obtained verbal and written informed consent from the patient/patients for the inclusion of their medical and treatment history within this case report.
Executive summary
Case reports
• Two newborns with hypoplastic left heart syndrome and restrictive atrial septum were transferred to the catheterization laboratory for urgent septostomy.
• The thick interatrial septum was easily crossed using the Baylis NRG™ radiofrequency (BRF) trans-septal needle (Baylis Medical, Montreal, Canada).
• In both procedures an atrial communication was successfully created without complications.
• In the first patient a stent was implanted and the second one underwent static balloon septoplasty.
• Both patients underwent Norwood palliation.
Discussion
• The BRF needle is a stiff and steerable system, which facilitates maneuvering within the atrium and alignment against the septum.
• It is easily seen on echo, thus positioning at the desired area of the septum is done without difficulty.
• Only minimal forward force is necessary to cross the septum as radiofrequency energy is delivered.
• Fewer exchange of catheters are required to establish a stable wire position in the left atrium.
Conclusion
• The use of the BRF trans-septal needle is a novel and reliable technique to create an atrial communication in hypoplastic left heart syndrome–restrictive atrial septum.
• It facilitates the procedure and overcomes some of the difficulties of previous techniques.
References
Papers of special note have been highlighted as: • of interest; •• of considerable interest
- Rychik J, Rome JJ, Collins MH et al. The hypoplastic left heart syndrome with intact atrial septum: atrial morphology, pulmonary vascular histopathology and outcome. J. Am. Coll. Cardiol. 34(2), 554–560 (1999).
- Hoque T, Richmond M, Vincent JA et al. Current outcomes of hypoplastic left heart syndrome with restrictive atrial septum: a single-center experience. Pediatr. Cardiol. 34(5), 1181–1189 (2013).
- Hoque T, Richmond M, Vincent JA et al. Current outcomes of hypoplastic left heart syndrome with restrictive atrial septum: a single-center experience. Pediatr. Cardiol. 34(5), 1181–1189 (2013).
- Hill K, Fudge JC, Barker P et al. Novel transatrial septoplasty technique for neonates with hypoplastic left heart syndrome and an intact or highly restrictive atrial septum. Pediatr. Cardiol. 31(4), 545–549 (2010).
- Marshall AC, Levine J, Morash D et al. Results of in utero atrial septoplasty in fetuses with hypoplastic left heart syndrome. Prenat. Diagn. 28, 1023–1028 (2008).
- Javois AJ, Van Bergen AH, Cuneo BF et al. Novel approach to the newborn with hypoplastic left heart syndrome and intact atrial septum. Catheter. Cardiovasc. Interv. 66(2), 268–272 (2005).
- Du Marchie Sarvaas GJ, Trivedi KR, Hornberger LK et al. Radiofrequency-assisted atrial septoplasty for an intact atrial septum in complex congenital heart disease. Catheter. Cardiovasc. Interv. 56(3), 412–415 (2002).
- Xu Z1, Owens G, Gordon D et al. Noninvasive creation of an atrial septal defect by histotripsy in a canine model. Circulation 121(6), 742–749 (2010).
- Gordon BM, Levi DS, Shannon KM. Electrosurgical energy in combination with a transseptal needle: a novel method for the creation of an atrial communication in hypoplastic left heart syndrome with intact atrial septum. Catheter. Cardiovasc. Interv. 73(1), 113–116 (2009).
•• Describes the high mortality of hypoplastic left heart syndrome (HLHS) associated with intact atrial septum.
• One institution’s experience with HLHS–restrictive atrial septum (RS) is presented. It describes the progress on outcome over the years.
• Description of different transcatheter techniques performed on the atrial septum of HLHS patients.
• Reports the use of a hybrid technique for creation of an atrial communication in HLHS–RS.
• Early results of prenatal atrial septoplasty in HLHS–RS are presented.
• Case report of the use of radiofrequency in HLHS–RS. It highlights the current technical difficulties associated with the use of radiofrequency in these patients.
• Describes the use of radiofrequency energy for trans-septal perforation in three patients with HLHS–RS.
• Describes the creation of an atrial septal defect in a live canine model with extracardiac histotripsy.
•• Describes the use of electrosurgical energy in combination with a conventional trans-septal needle to create an atrial communication.