Device Evaluations - Interventional Cardiology (2013) Volume 5, Issue 4
The GuideLiner: an interventionists experience of their first 50 cases: the mostly good, rarely bad, beware of the ugly
- Corresponding Author:
- Peter O’Kane
Dorset Heart Centre, Royal Bournemouth Hospital
Bournemouth, BH7 7DX, UK
Tel: +44 120 270 4333
E-mail: peter.o'kane@rbch.nhs.uk
Abstract
The past two decades have witnessed significant advances in interventional cardiology. Development of new devices, adjunctive techniques and pharmacotheraputics have been necessary to meet the demand of increasingly complex cases that are now routinely referred and accepted for percutaneous coronary intervention (PCI). Chronically occluded vessels, excessively tortuous coronary anatomy and severe calcific coronary disease typically encountered in the elderly population and/or those deemed unsuitable for surgical revascularization present as daily challenges. A contemporary interventional cardiologist must be equipped with the necessary tools and expertise to safely and effectively tackle these demanding cases.
Keywords
coronary artery disease, coronary stents, GuideLiner® catheter, percutaneous coronary intervention
The past two decades have witnessed significant advances in interventional cardiology. Development of new devices, adjunctive techniques and pharmacotheraputics have been necessary to meet the demand of increasingly complex cases that are now routinely referred and accepted for percutaneous coronary intervention (PCI). Chronically occluded vessels, excessively tortuous coronary anatomy and severe calcific coronary disease typically encountered in the elderly population and/or those deemed unsuitable for surgical revascularization present as daily challenges. A contemporary interventional cardiologist must be equipped with the necessary tools and expertise to safely and effectively tackle these demanding cases.
A frequently occurring dilemma encountered in patients with complex coronary anatomy undergoing PCI is failure to deliver balloons and/or stents to the distal target lesion. Various techniques have been adopted to overcome this problem including the use of: more supportive and aggressive guide catheters to facilitate deep intubation of the target vessel; an additional supportive guidewire (‘buddy wire’) to assist with the straightening out of tortuous vessels and improving guide catheter coaxiality [1,2]; the anchor balloon technique to steady the guide catheter and provide more pushability [3]; rotational or laser atherectomy to effectively debulk calcific lesions prior to stent delivery; and newer, improved stent designs with better overall deliverability. Nonetheless, despite these useful adjunctive techniques and devices, stent delivery failure is still encountered in approximately 5% of cases, leading to procedural failure, incomplete revascularization and poor clinical outcomes [4].
Of the above techniques, deep seating of the guide catheter is often tempting when resistance to device delivery is encountered, but caution must be applied in view of the significant risk of proximal vessel dissection. This is the main catalyst that led to the development of guide catheter extensions whereby a smaller lumen ‘inner’ catheter can be advanced within the guide catheter to take up a distal position in the vessel, thus providing extra backup support without traumatizing the proximal vessel. There are a number of systems available including the GuideLiner® catheter (Vascular Solutions, MN, USA) [5-12], the Heartrail® II catheter (Terumo Corporation, Tokyo, Japan) [13,14] and the Proxis™ device (St Jude Medical, MN, USA) [15,16].
The GuideLiner catheter is a soft-tipped, coaxial guide catheter extension that is specifically designed to be deeply intubated into the target coronary artery to permit safe and effective delivery of balloons and/or stents within challenging coronary anatomy where conventional techniques have failed. The major advantage of this device over its competitors is that it can be passed through the proximal guide catheter hemostatic valve without disconnection, resulting in relatively simple manipulation and rapid exchange.
Until recently, the only published literature on the GuideLiner catheter was relatively small case series. However, de Man et al. have just reported their experience of 65 consecutive cases in the Twente GuideLiner registry performed by five interventional cardiologists over an 8-month period in a high-volume PCI center. A third of the cases in this series were transradial and the authors concluded that the GuideLiner catheter was associated with high procedural success (93%) and no major complications [12].
The purpose of this article is to report the experience of the GuideLiner catheter in 50 complex PCI cases undertaken and/or supervised by a single interventional cardiologist resident within the highest-volume nonsurgical PCI center in the UK. Between October 2010 and June 2012, consecutive PCI cases where the GuideLiner catheter was utilized are included. The primary interventional operator has performed over 2200 PCI procedures in the last 5 years and is a supervisor to interventional fellows within the center. In this 20-month period, the operator performed and/or supervised 897 interventional cases, 83% of which were performed transradially. The case mix included rotational atherectomy in 65 (7%) patients and laser atherectomy on 29 (3%) patients.
We present: a step-by-step description of the GuideLiner catheter delivery technique; its various clinical indications in our specific case series, including practical ‘tips and tricks’ and an outline of the learning curve; device limitations and specific complications encountered in this series; and modifications of the new and improved GuideLiner catheter. To our knowledge, this is the first published device evaluation of its kind that includes a large series of patients in a single institution treated by one consultant interventional cardiologist, unlike previous published work on this subject that included the collective experience of multiple operators.
Device characteristics
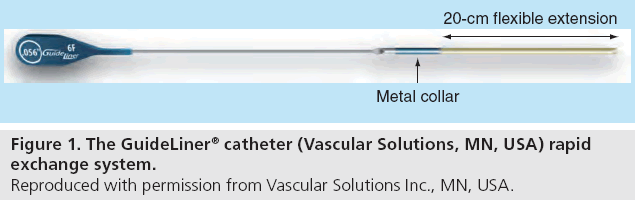
The GuideLiner catheter is a coaxial guide catheter extension that received CE marking for assistance with device delivery during PCI in September 2009. It is composed of a flexible 20-cm guide extension connected via a metal collar to a 125- cm stainless steel shaft (Figure 1).The soft-tipped extension is coated with silicone for lubricity and comprises an inner polytetrafluoroethylene lining surrounded by a stainless steel coil for flexibility and strength.
The GuideLiner is delivered on its monorail system through a standard guide catheter by advancement over the primary guidewire (0.014 inches). It travels through the Y-adaptor hemostasis valve without the need to disconnect the valve from the guide catheter, thereby providing the advantage of rapid exchange. Delivery of the GuideLiner into the target vessel is aided by a radiopaque marker located 0.105 inches (2.667 mm) from the distal tip and two positioning markers located 95 cm (single mark) and 105 cm (double mark) from the distal tip, respectively.
The internal diameter of the GuideLiner extension is approximately 1 Fr size smaller than the guide catheter and is currently available in three sizes: 5-in-6 (0.056-inch internal diameter), 6-in-7 (0.062-inch internal diameter) and 7-in-8 (0.071-inch internal diameter). The manufacturer does not generally recommend the GuideLiner for use in target vessels of less than 2.5 mm in diameter.
GuideLiner technique: step-by-step guide
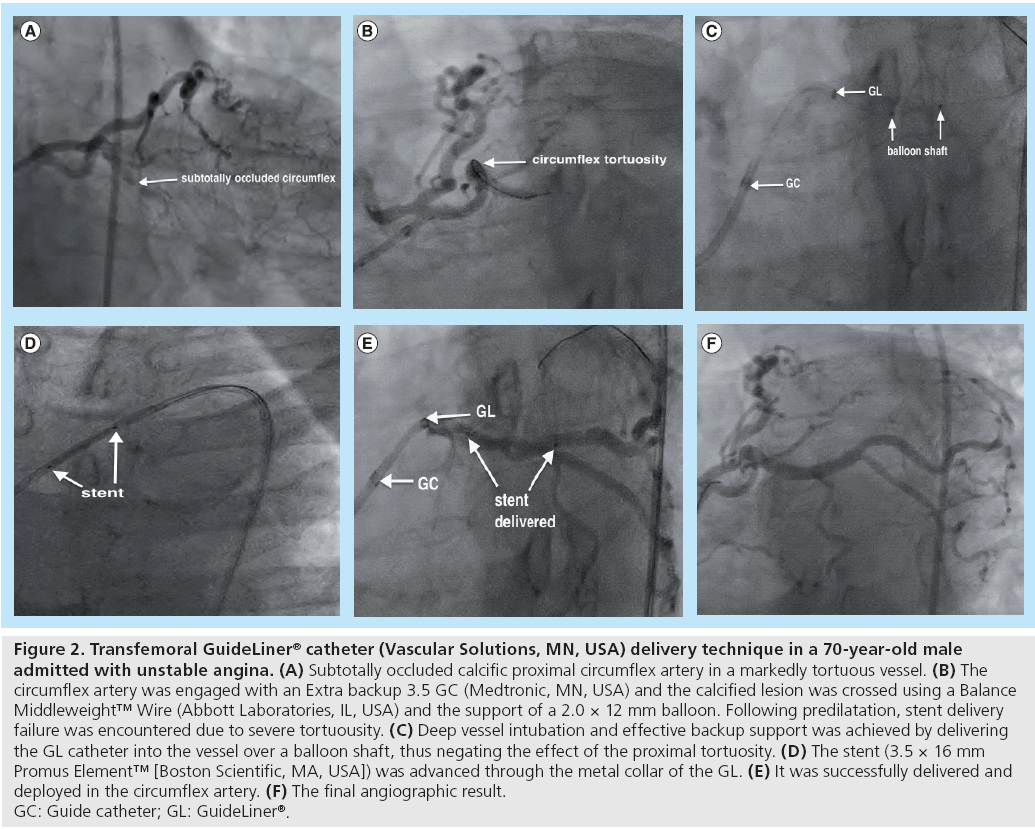
The GuideLiner catheter permits very deep intubation of the target vessel, thus providing backup support to facilitate stent delivery across heavily calcified lesions and/or tortuous vessels. The deeply-engaged extension is always aligned coaxial to the target vessel, and this is particularly useful if the take-off of the coronary ostium impedes coaxial engagement of the guiding catheter. The following is a step-by-step outline of the GuideLiner catheter delivery technique (Figure 2):
Figure 2: Transfemoral GuideLiner® catheter (Vascular Solutions, MN, USA) delivery technique in a 70-year-old male admitted with unstable angina. (A) Subtotally occluded calcific proximal circumflex artery in a markedly tortuous vessel. (B) The circumflex artery was engaged with an Extra backup 3.5 GC (Medtronic, MN, USA) and the calcified lesion was crossed using a Balance Middleweight™ Wire (Abbott Laboratories, IL, USA) and the support of a 2.0 × 12 mm balloon. Following predilatation, stent delivery failure was encountered due to severe tortuousity. (C) Deep vessel intubation and effective backup support was achieved by delivering the GL catheter into the vessel over a balloon shaft, thus negating the effect of the proximal tortuosity. (D) The stent (3.5 × 16 mm Promus Element™ [Boston Scientific, MA, USA]) was advanced through the metal collar of the GL. (E) It was successfully delivered and deployed in the circumflex artery. (F) The final angiographic result. GC: Guide catheter; GL: GuideLiner®.
▪ Flush the lumen of the GuideLiner catheter with heparinized saline solution;
▪Backload the distal tip of the GuideLiner onto the primary guidewire and advance the GuideLiner on its monorail system through the Y-adaptor hemostasis valve;
▪ Under fluoroscopic guidance, advance and position the GuideLiner at the desired location within the vessel (up to a maximum of 10 cm beyond the distal end of the guiding catheter to prevent the metal collar from exiting the guiding catheter). Our experience has been that coaxial deep vessel intubation with the GuideLiner is more easily achieved by first delivering an uninflated balloon over the primary guidewire into the distal vessel, followed by advancement of the GuideLiner;
▪ With the GuideLiner fixed in the optimal position within the vessel, backload the required coronary stent over the primary guidewire;
▪ Under f luoroscopic guidance, carefully advance the stent into the guiding catheter through the metal collar of the GuideLiner, but be wary of resistance to stent advancement at this point (please refer to the ‘Tips and tricks’ section for further details);
▪ The stent should exit the distal end of the GuideLiner with ease and be delivered to the desired location within the vessel;
▪ If further overlapping stents are required proximally, the GuideLiner can either be retracted to a more proximal position, left at the inflow of the delivered stent or advanced carefully into the delivered stent to facilitate overlap of the proximal stent;
▪ On completion of the interventional procedure, gently pull the GuideLiner out under fluroscopic guidance prior to removing the guide catheter from the vessel.
Clinical indications and applications
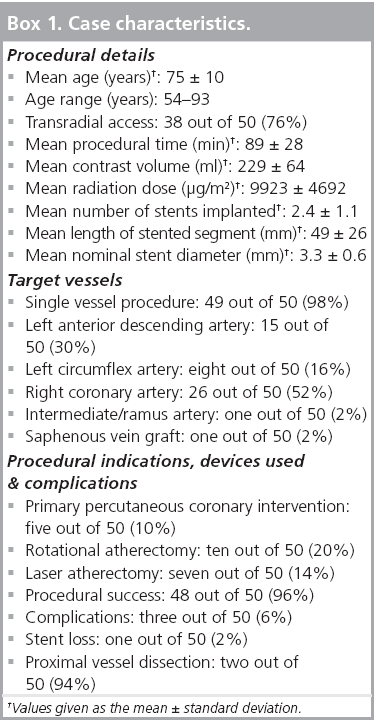
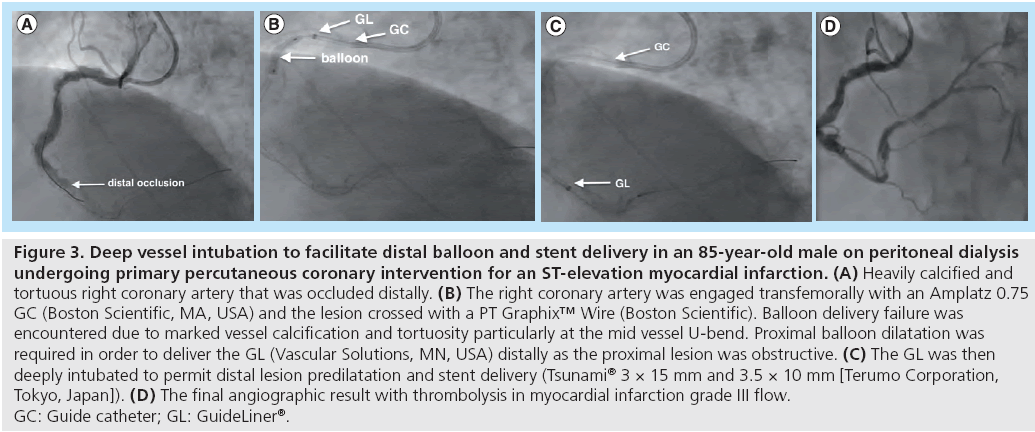
In all 50 PCI cases where the GuideLiner catheter was used, patients received preloading with aspirin (300 mg) and clopidogrel (300–600 mg) or prasugrel (60 mg). Unfractionated heparin (70 IU/kg), bivalirudin and/or abciximab were used during PCI, dependent on clinical presentation. A summary of procedural details for the 50 patients is outlined in Box 1.
We employed the GuideLiner to overcome unfavorable coronary anatomy and/or complex coronary lesions during PCI. In the early cases where the GuideLiner was used, this followed more established techniques for stent delivery in complex lesions, such as the use of an additional supportive ‘buddy’ wire, more aggressive guide catheters and adjunctive devices such as laser or rotational atherectomy. However, as experienced was gained, the GuideLiner was used more as a first-line tool when difficulty was encountered. It should also be highlighted that some of the excellent supportive and deliverable guidewires currently marketed were not available during this case series.
Without the use of the GuideLiner, some cases may not have been successfully completed and others would have entailed unacceptably prolonged procedural times, inadvertently exposing the patient to increased risks associated with high contrast load and radiation dose. The specific procedural indications for using the GuideLiner catheter during PCI can be categorized as follows:
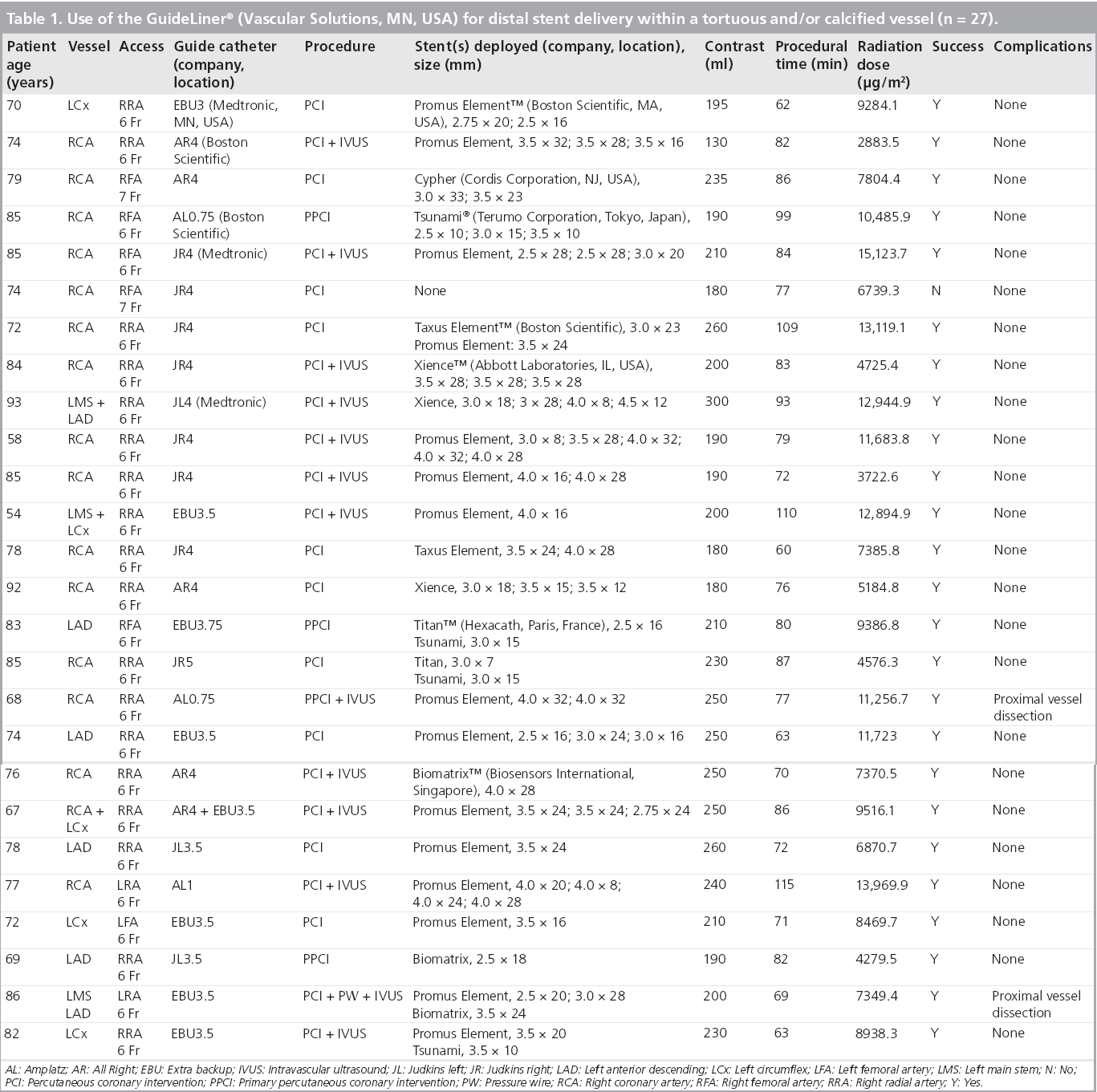
▪ Distal stent delivery within a tortuous vessel and/or calcified vessel: this was the indication for 27 out of 50 cases (Table 1). When conventional techniques fail to deliver a stent distally within a tortuous vessel, the GuideLiner is advanced distally over the guidewire or balloon shaft providing more effective backup support to enable successful delivery of the device (Figure 3);
Figure 3: Deep vessel intubation to facilitate distal balloon and stent delivery in an 85-year-old male on peritoneal dialysis undergoing primary percutaneous coronary intervention for an ST-elevation myocardial infarction. (A) Heavily calcified and tortuous right coronary artery that was occluded distally. (B) The right coronary artery was engaged transfemorally with an Amplatz 0.75 GC (Boston Scientific, MA, USA) and the lesion crossed with a PT Graphix™ Wire (Boston Scientific). Balloon delivery failure was encountered due to marked vessel calcification and tortuosity particularly at the mid vessel U-bend. Proximal balloon dilatation was required in order to deliver the GL (Vascular Solutions, MN, USA) distally as the proximal lesion was obstructive. (C) The GL was then deeply intubated to permit distal lesion predilatation and stent delivery (Tsunami® 3 × 15 mm and 3.5 × 10 mm [Terumo Corporation, Tokyo, Japan]). (D) The final angiographic result with thrombolysis in myocardial infarction grade III flow. GC: Guide catheter; GL: GuideLiner®.
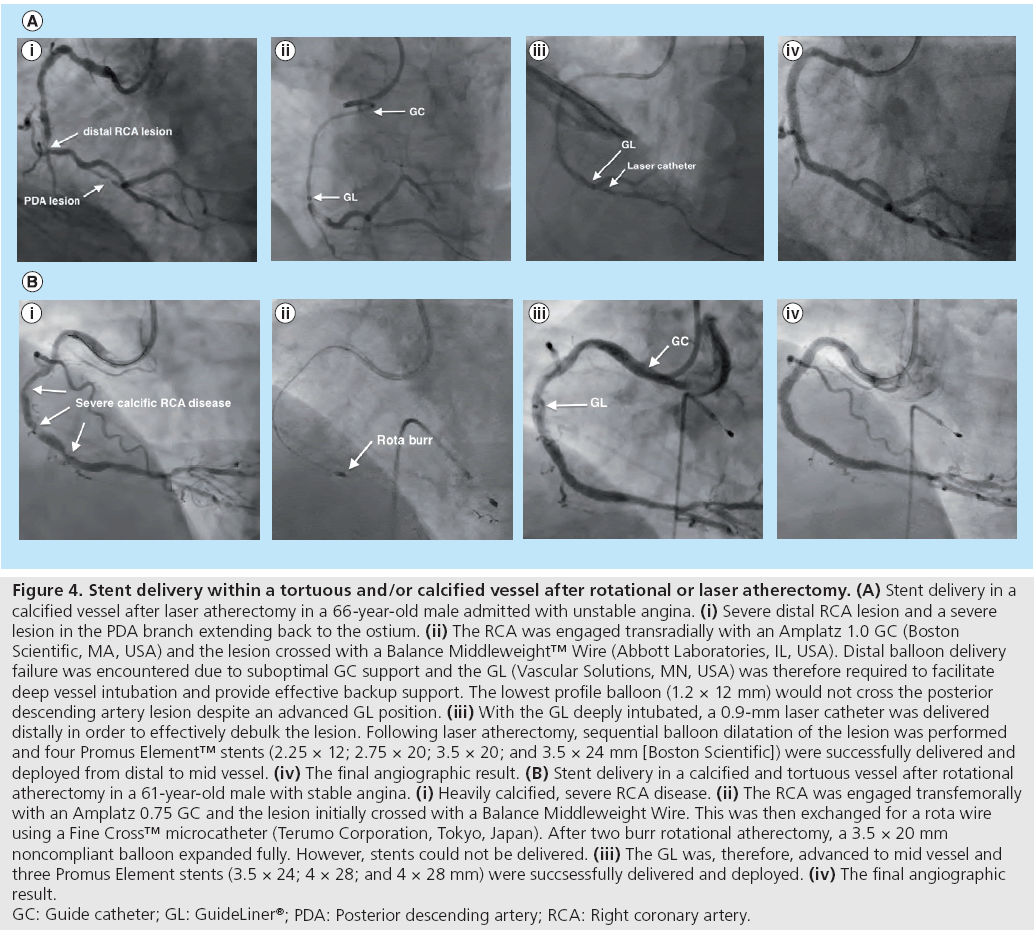
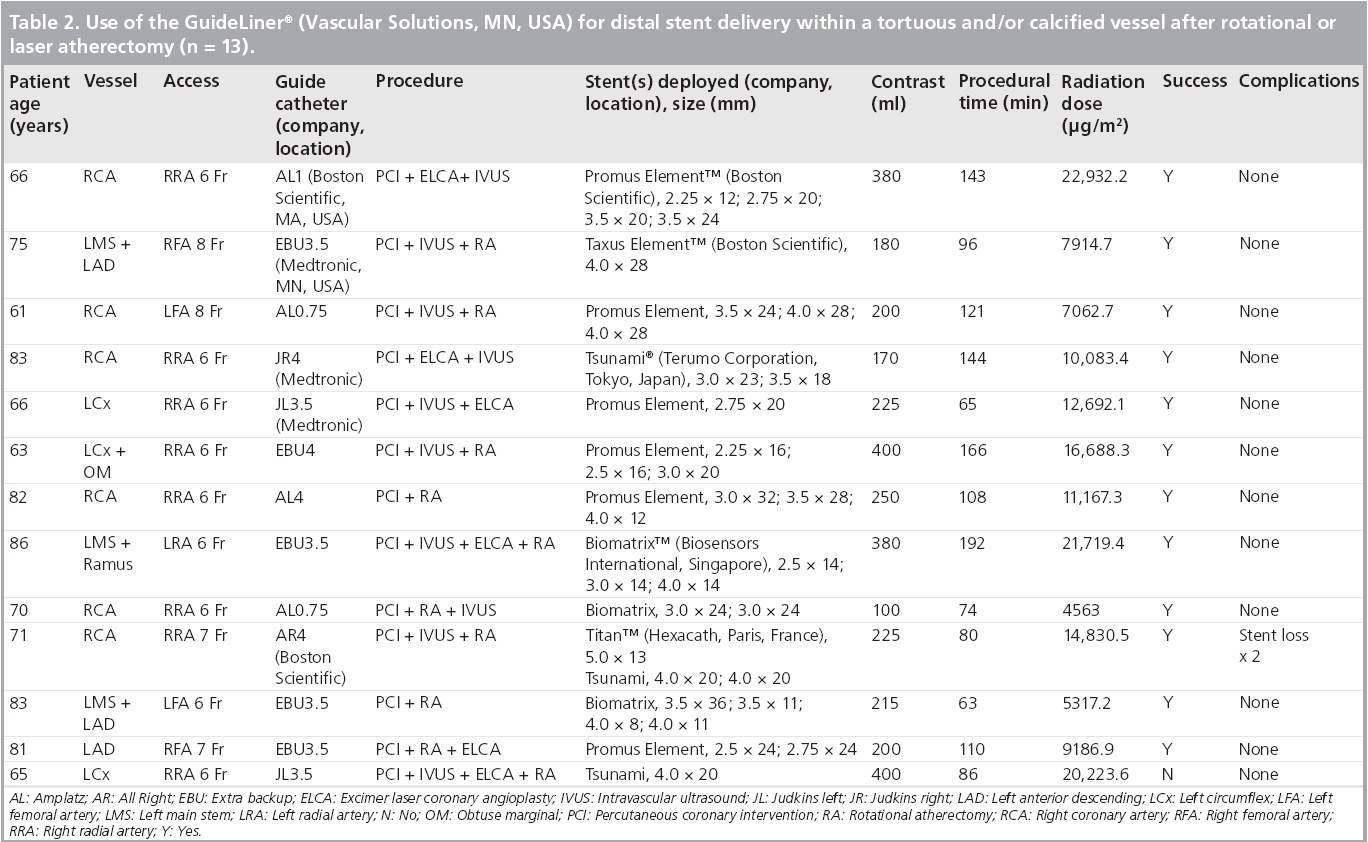
▪ Distal stent delivery within a tortuous vessel and/or calcified vessel after rotational or laser atherectomy: this was the indication for 13 out of 50 cases (Table 2). The GuideLiner can be utilized to facilitate stent delivery in heavily calcified vessels after debulking the lesion with rotational or laser atherectomy (Figure 4);
Figure 4: Stent delivery within a tortuous and/or calcified vessel after rotational or laser atherectomy. (A) Stent delivery in a
calcified vessel after laser atherectomy in a 66-year-old male admitted with unstable angina. (i) Severe distal RCA lesion and a severe
lesion in the PDA branch extending back to the ostium. (ii) The RCA was engaged transradially with an Amplatz 1.0 GC (Boston
Scientific, MA, USA) and the lesion crossed with a Balance Middleweight™ Wire (Abbott Laboratories, IL, USA). Distal balloon delivery
failure was encountered due to suboptimal GC support and the GL (Vascular Solutions, MN, USA) was therefore required to facilitate
deep vessel intubation and provide effective backup support. The lowest profile balloon (1.2 × 12 mm) would not cross the posterior
descending artery lesion despite an advanced GL position. (iii) With the GL deeply intubated, a 0.9-mm laser catheter was delivered
distally in order to effectively debulk the lesion. Following laser atherectomy, sequential balloon dilatation of the lesion was performed
and four Promus Element™ stents (2.25 × 12; 2.75 × 20; 3.5 × 20; and 3.5 × 24 mm [Boston Scientific]) were successfully delivered and
deployed from distal to mid vessel. (iv) The final angiographic result. (B) Stent delivery in a calcified and tortuous vessel after rotational
atherectomy in a 61-year-old male with stable angina. (i) Heavily calcified, severe RCA disease. (ii) The RCA was engaged transfemorally
with an Amplatz 0.75 GC and the lesion initially crossed with a Balance Middleweight Wire. This was then exchanged for a rota wire
using a Fine Cross™ microcatheter (Terumo Corporation, Tokyo, Japan). After two burr rotational atherectomy, a 3.5 × 20 mm
noncompliant balloon expanded fully. However, stents could not be delivered. (iii) The GL was, therefore, advanced to mid vessel and
three Promus Element stents (3.5 × 24; 4 × 28; and 4 × 28 mm) were succsessfully delivered and deployed. (iv) The final angiographic
result.
GC: Guide catheter; GL: GuideLiner®; PDA: Posterior descending artery; RCA: Right coronary artery.
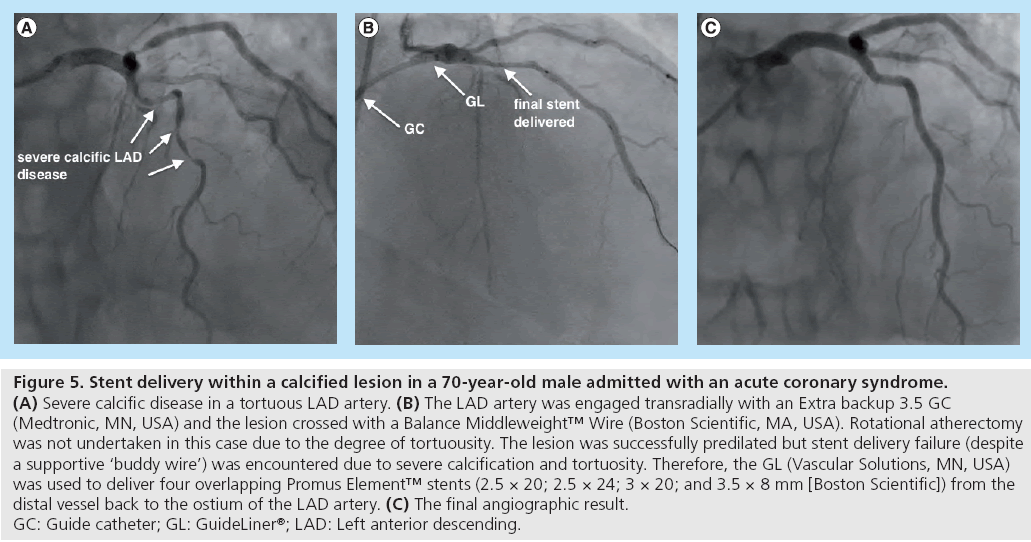
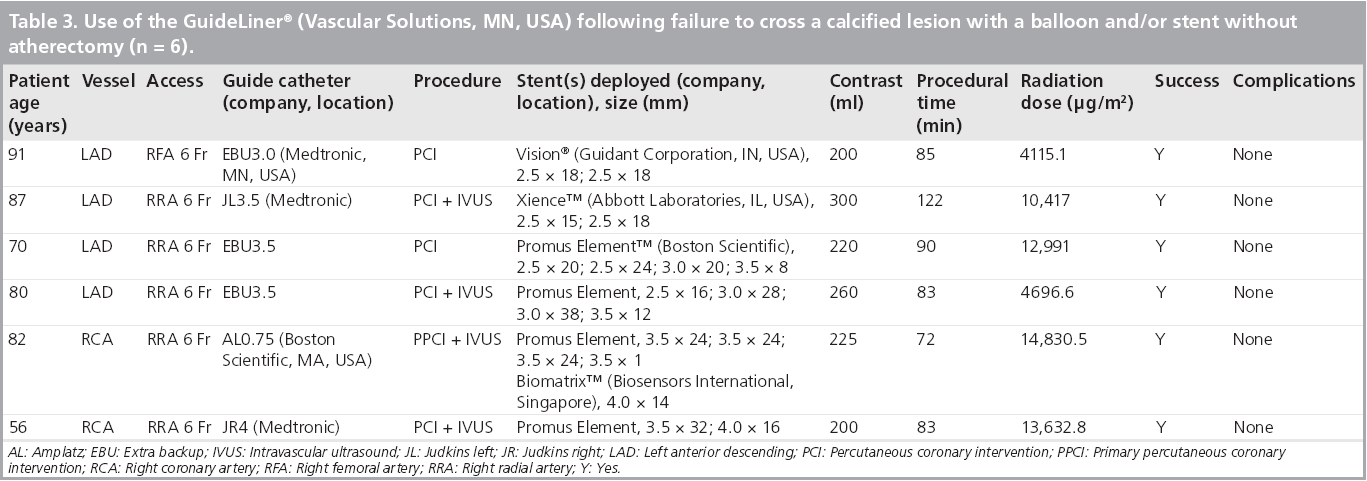
▪ Failure to cross a calcified lesion with a balloon and/or stent without atherectomy: this was the indication for six out of 50 cases (Table 3). In the context of a heavily calcified lesion that is uncrossable with a balloon or stent, the GuideLiner is utilized to facilitate stent delivery when atherectomy is either not feasible or desirable (Figure 5);
Figure 5: Stent delivery within a calcified lesion in a 70-year-old male admitted with an acute coronary syndrome.
(A) Severe calcific disease in a tortuous LAD artery. (B) The LAD artery was engaged transradially with an Extra backup 3.5 GC
(Medtronic, MN, USA) and the lesion crossed with a Balance Middleweight™ Wire (Boston Scientific, MA, USA). Rotational atherectomy
was not undertaken in this case due to the degree of tortuousity. The lesion was successfully predilated but stent delivery failure (despite
a supportive ‘buddy wire’) was encountered due to severe calcification and tortuosity. Therefore, the GL (Vascular Solutions, MN, USA)
was used to deliver four overlapping Promus Element™ stents (2.5 × 20; 2.5 × 24; 3 × 20; and 3.5 × 8 mm [Boston Scientific]) from the
distal vessel back to the ostium of the LAD artery. (C) The final angiographic result.
GC: Guide catheter; GL: GuideLiner®; LAD: Left anterior descending.
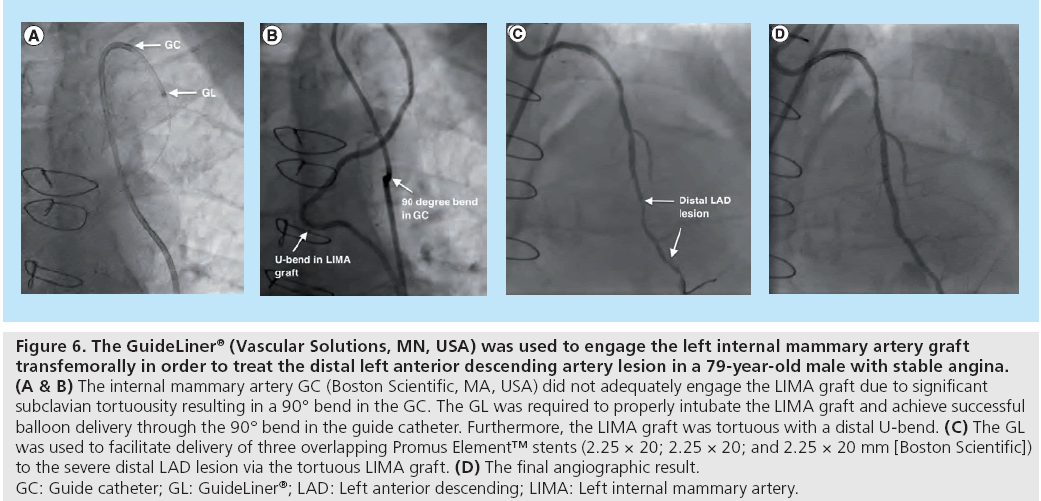
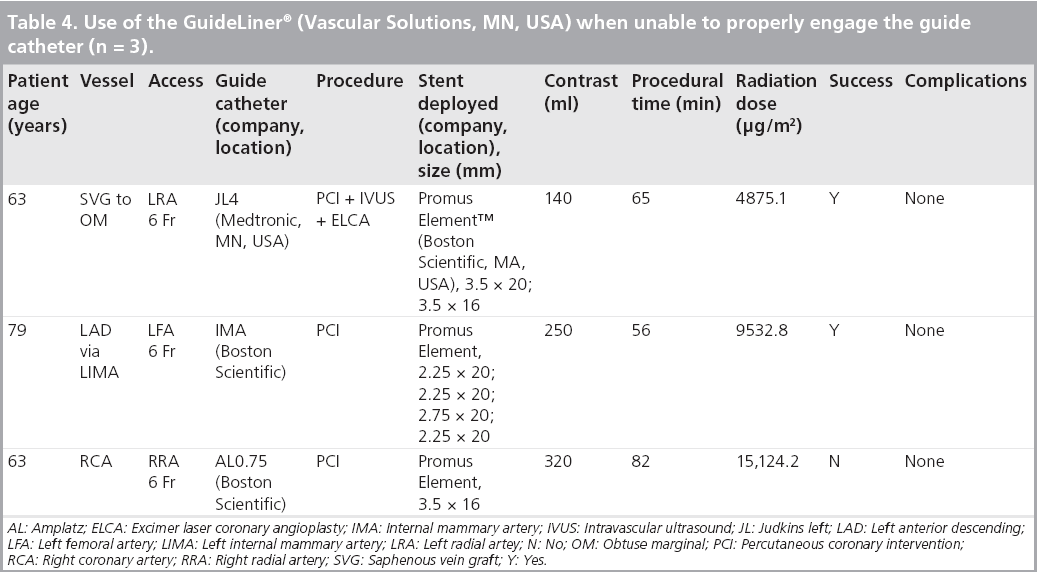
▪ Inability to properly engage the guide catheter: this was the indication for three out of 50 cases (Table 4). In some cases, difficult coronary ostium take-off prevents coaxial engagement of the guiding catheter. The GuideLiner is useful in this situation, particularly when intubating arterial or vein graft ostia (Figure 6);
Figure 6: The GuideLiner® (Vascular Solutions, MN, USA) was used to engage the left internal mammary artery graft transfemorally in order to treat the distal left anterior descending artery lesion in a 79-year-old male with stable angina. (A and B) The internal mammary artery GC (Boston Scientific, MA, USA) did not adequately engage the LIMA graft due to significant subclavian tortuousity resulting in a 90° bend in the GC. The GL was required to properly intubate the LIMA graft and achieve successful balloon delivery through the 90° bend in the guide catheter. Furthermore, the LIMA graft was tortuous with a distal U-bend. (C) The GL was used to facilitate delivery of three overlapping Promus Element™ stents (2.25 × 20; 2.25 × 20; and 2.25 × 20 mm [Boston Scientific]) to the severe distal LAD lesion via the tortuous LIMA graft. (D) The final angiographic result. GC: Guide catheter; GL: GuideLiner®; LAD: Left anterior descending; LIMA: Left internal mammary artery.
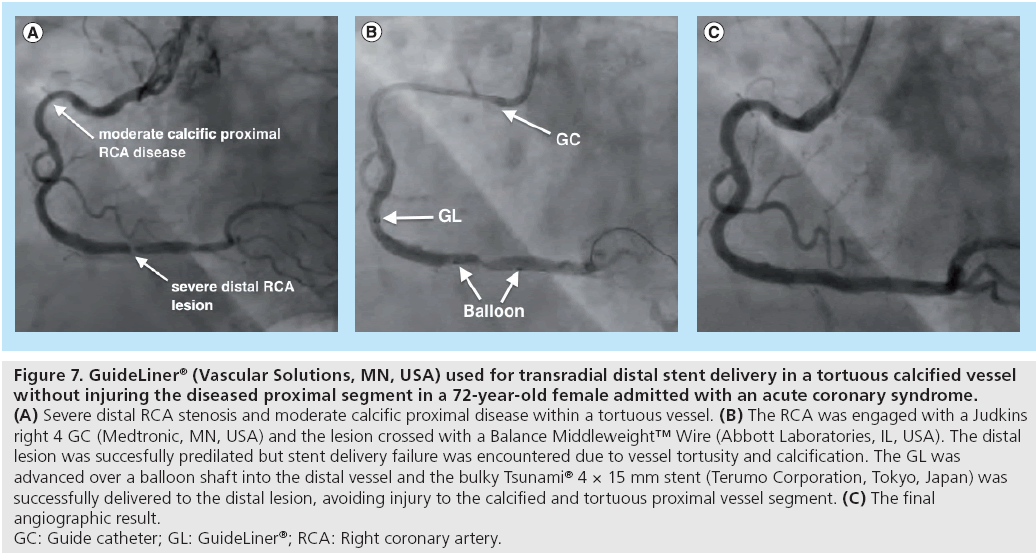
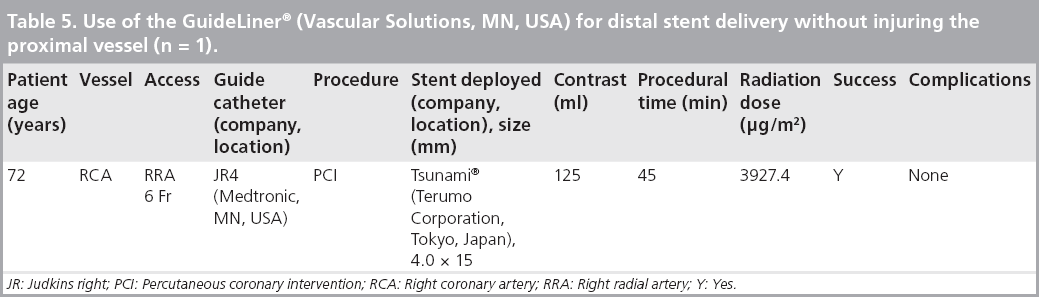
▪ Distal stent delivery without injuring the proximal vessel: this was the indication for one out of 50 cases (Table 5). In some situations, the target lesion is in the distal segment of the vessel and may require a relatively large-diameter stent delivered across a very tortuous and moderately diseased proximal vessel. In this situation, in order to avoid injuring the proximal vessel during stent delivery, the GuideLiner is gently advanced across the tortuous proximal segment resulting in safe and effective delivery of the bulky stent distally (Figure 7);
Figure 7: GuideLiner® (Vascular Solutions, MN, USA) used for transradial distal stent delivery in a tortuous calcified vessel
without injuring the diseased proximal segment in a 72-year-old female admitted with an acute coronary syndrome.
(A) Severe distal RCA stenosis and moderate calcific proximal disease within a tortuous vessel. (B) The RCA was engaged with a Judkins
right 4 GC (Medtronic, MN, USA) and the lesion crossed with a Balance Middleweight™ Wire (Abbott Laboratories, IL, USA). The distal
lesion was succesfully predilated but stent delivery failure was encountered due to vessel tortusity and calcification. The GL was
advanced over a balloon shaft into the distal vessel and the bulky Tsunami® 4 × 15 mm stent (Terumo Corporation, Tokyo, Japan) was
successfully delivered to the distal lesion, avoiding injury to the calcified and tortuous proximal vessel segment. (C) The final
angiographic result.
GC: Guide catheter; GL: GuideLiner®; RCA: Right coronary artery.
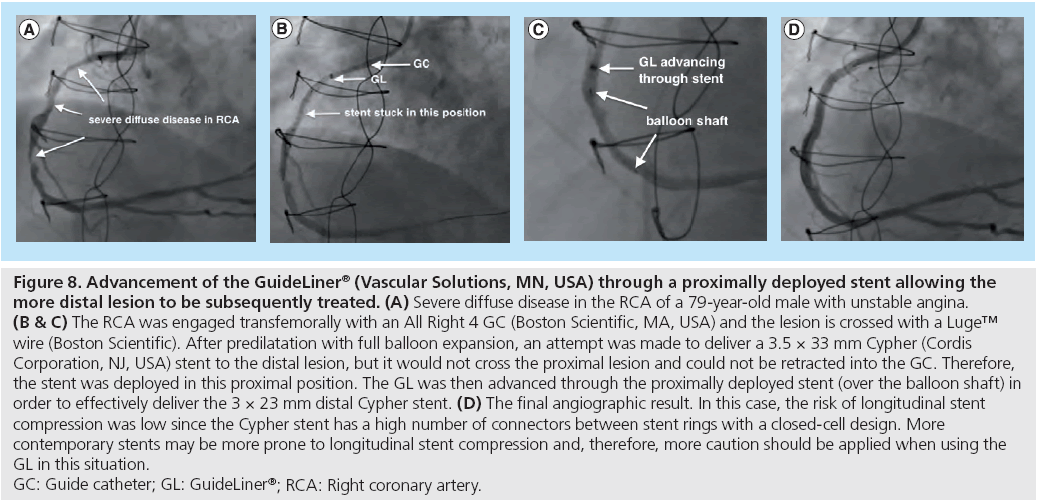
▪ Proximal to distal vessel stenting: although the conventional approach to stenting a long segment of disease is to deliver overlapping stents from distal to proximal vessel, this may not be feasible in certain situations. For example, when a stent is trapped within a proximal lesion and has to be deployed at this position, the GuideLiner can then be used to deliver further stents distally through the proximally deployed stent, allowing for proximal-to-distal vessel stenting. An example of such a case is described in Figure 8. Caution needs to be applied to avoid longitudinal stent compression and this technique is best performed by advancing the GuideLiner over the initial proximal stent balloon.
Figure 8: Advancement of the GuideLiner® (Vascular Solutions, MN, USA) through a proximally deployed stent allowing the
more distal lesion to be subsequently treated. (A) Severe diffuse disease in the RCA of a 79-year-old male with unstable angina. (B and C) The RCA was engaged transfemorally with an All Right 4 GC (Boston Scientific, MA, USA) and the lesion is crossed with a Luge™
wire (Boston Scientific). After predilatation with full balloon expansion, an attempt was made to deliver a 3.5 × 33 mm Cypher (Cordis
Corporation, NJ, USA) stent to the distal lesion, but it would not cross the proximal lesion and could not be retracted into the GC. Therefore,
the stent was deployed in this proximal position. The GL was then advanced through the proximally deployed stent (over the balloon shaft) in
order to effectively deliver the 3 × 23 mm distal Cypher stent. (D) The final angiographic result. In this case, the risk of longitudinal stent
compression was low since the Cypher stent has a high number of connectors between stent rings with a closed-cell design. More
contemporary stents may be more prone to longitudinal stent compression and, therefore, more caution should be applied when using the
GL in this situation.
GC: Guide catheter; GL: GuideLiner®; RCA: Right coronary artery.
Other clinical applications
Other very useful clinical applications of the GuideLiner that have not been used in our case series but have been previously reported include the following:
▪ Treatment of chronic total occlusions using the retrograde technique: the GuideLiner can be used through the anterograde guide positioned at the proximal occlusion to aid externalization of the retrograde wire. This technique can be used routinely or when difficulty is encountered in advancing the retrograde wire all the way into the anterograde guide catheter;
▪ Retrieval of a trapped rotablation burr: in a recently reported case of an entrapped rotablator burr [17], the rotawire and burr were cut proximally to permit advancement of the GuideLiner. Subsequent traction on the burr with counter traction of the GuideLiner at the lesion allowed the burr to be successfully retrieved.
Tips and tricks
When using the GuideLiner catheter, the following ‘tips and tricks’ should be incorporated in order to ensure optimal performance of the device:
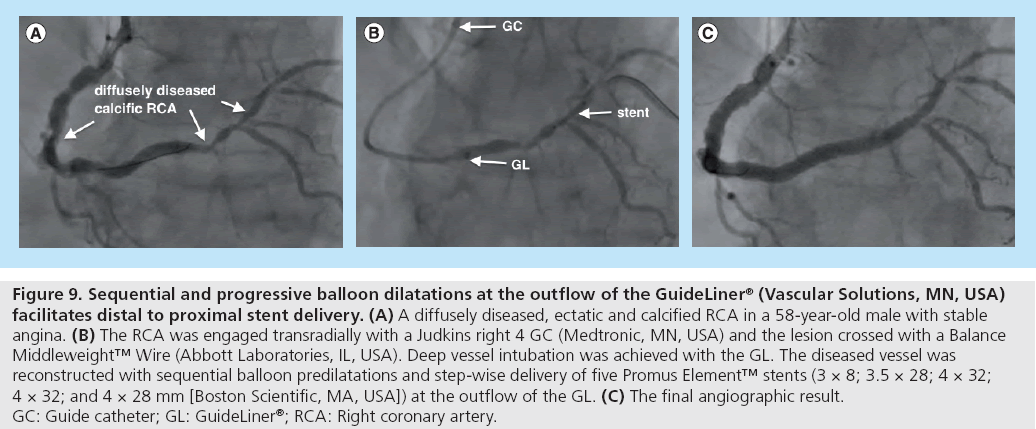
▪ To facilitate coaxial and safe delivery of the GuideLiner within the distal vessel, the GuideLiner is usually best advanced over a balloon so that it runs on the shaft without injuring the vessel and minimizes the risk of proximal vessel dissection. Resistance to advancement can be overcome by inflating the balloon within the distal target lesion followed by gentle traction on the balloon during the advancement of the GuideLiner to create an anchor effect. Alternatively, sequential and progressively increased distal balloon inflations at the outflow of the GuideLiner permit movement to a distal position (Figure 9);
Figure 9: Sequential and progressive balloon dilatations at the outflow of the GuideLiner® (Vascular Solutions, MN, USA) facilitates distal to proximal stent delivery. (A) A diffusely diseased, ectatic and calcified RCA in a 58-year-old male with stable angina. (B) The RCA was engaged transradially with a Judkins right 4 GC (Medtronic, MN, USA) and the lesion crossed with a Balance Middleweight™ Wire (Abbott Laboratories, IL, USA). Deep vessel intubation was achieved with the GL. The diseased vessel was reconstructed with sequential balloon predilatations and step-wise delivery of five Promus Element™ stents (3 × 8; 3.5 × 28; 4 × 32; 4 × 32; and 4 × 28 mm [Boston Scientific, MA, USA]) at the outflow of the GL. (C) The final angiographic result. GC: Guide catheter; GL: GuideLiner®; RCA: Right coronary artery.
▪ Occasionally, when attempting to deliver a distal stent, the stent can become wedged in the proximal lesion and can neither be advanced nor retracted to facilitate deployment in an adequate position. In this situation, the stent has to be deployed in this proximal position. The GuideLiner can then be advanced through the proximally deployed stent allowing the more distal lesion to be subsequently treated. Thus, with the GuideLiner, access to the distal vessel can be achieved safely. However, this must be performed very carefully, without much force and, preferably, over a balloon shaft so as not to cause longitudinal stent compression (Figure 8);
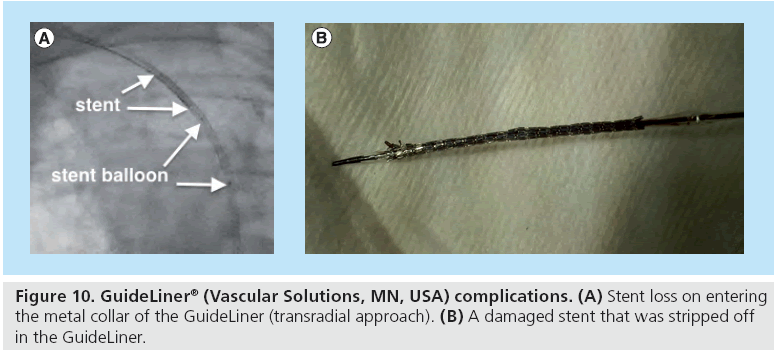
▪ Large-diameter bulky stents can be damaged or stripped off on entering the metal collar of the GuideLiner, particularly when the metal collar is situated within a bend in the guiding catheter. In this situation, gentle retraction of the GuideLiner so as to place the metal collar in a straighter segment of the guiding catheter is required. Alternatively, this problem can potentially be avoided by introducing the stent into the GuideLiner outside of the guide catheter and subsequently advancing both systems together. However, this maneuver may be difficult when an anchor balloon is required for deep-vessel intubation of the GuideLiner. Extreme caution must be exercised when using large-diameter stents and the use of lower profile, less bulky stents should always be considered in the first instance (Figure 10);
▪ When dealing with calcific lesions that require debulking, it is important to bear in mind when planning the intervention strategy that rotational atherectomy cannot be performed through the GuideLiner catheter since even the smallest rotablator burr is too bulky a device. Alternatively, a small-diameter cutting balloon, for example a 2.5 × 10 mm balloon (Boston Scientific, MA, USA), can travel through the 6-in-7 GuideLiner if required, although a 3.0 × 10 mm cannot.
Device limitations and complications
The GuideLiner has few but important limitations. First, the requirement for deep vessel intubation, typically within tortuous or calcific arteries, means there is the potential risk of proximal vessel dissection. In the authors experience, this occurred in two (4%) cases. This complication can be minimized by systematically advancing the GuideLiner over the balloon shaft, as previously described, or using the dedicated GuideLiner Navigation™ catheter (Vascular Solutions). The Navigation catheter is a dilator-like delivery catheter designed to protect the arterial wall during guide deep seating using rapid exchange delivery over a 0.014-inch guidewire. It is not yet distributed in the UK and the authors have, therefore, not experienced its use.
Second, there is the risk of damage to larger, bulkier stents during their passage through the metal collar, particularly when the collar is situated at a bend in the guiding catheter [18,19]. In our series, we encountered two incidences (in one patient) of stent loss in the metal collar, which occurred in a 7 Fr GuideLiner using 5-mm diameter stents. Fortunately, both stents were easily retrieved. As such, caution must be exercised during stent passage through the metal collar and, if significant resistance is encountered, the stent should be immediately withdrawn and carefully examined for damage prior to proceeding with the case. Recent design modifications of the GuideLiner catheter, as described below, will address this particular limitation.
Third, there is the potential for ‘guidewire wrap’ particularly if two or more wires are used. To avoid this complication, the GuideLiner should be advanced without rotation and should only be advanced over the primary guidewire as secondary wires may wrap around the GuideLiner, thus preventing advancement of the balloon or stent.
New device components
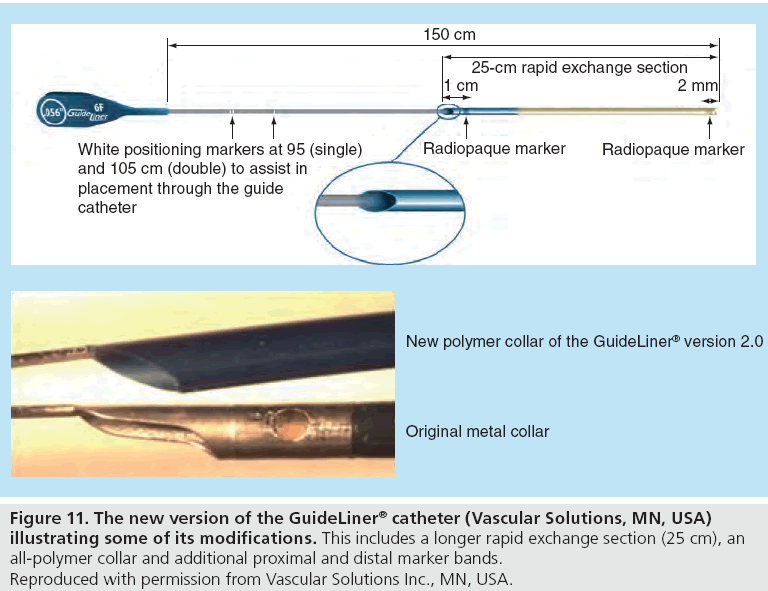
In view of the above limitations, the GuideLiner catheter has been redesigned with the following changes incorporated into the new GuideLiner version 2.0 in order to ensure an improved safety and efficacy profile (Figure 11):
Figure 11: The new version of the GuideLiner® catheter (Vascular Solutions, MN, USA) illustrating some of its modifications. This includes a longer rapid exchange section (25 cm), an all-polymer collar and additional proximal and distal marker bands. Reproduced with permission from Vascular Solutions Inc., MN, USA.
▪ Length of rapid exchange section increased from 20 to 25 cm to allow deeper vessel intubation;
▪ Additional 5.5 Fr size for compatibility for all 6 Fr guiding catheters;
▪ Metal collar changed to an all-polymer collar for improved flexibility, which helps reduce the risk of stent damage or dislodgement;
▪ Added proximal and distal marker bands.
Center-based discussion of the experiences encountered
We have described our experience with the GuideLiner version 1.0 catheter in 50 complex PCI cases undertaken and/or supervised by a single operator at a high-volume center. In our experience, the GuideLiner was successful in 96% of cases and device-related procedural complications were encountered in 4% of cases. Specifically, proximal vessel dissection occurred in two out of 50 patients. As discussed, the risk of this complication occurring can be minimized by very careful advancement of the GuideLiner over a balloon shaft or by using the dedicated GuideLiner Navigation catheter.
Furthermore, in our series, we encountered two incidences of stent loss, both of which occurred during the passage of a 5-mm diameter stent within the metal collar of a 7 Fr GuideLiner. This problem can be attenuated by very careful advancement of the stent through the metal collar and, if any resistance is encountered, the location of the stent in relation to the metallic collar should be established and the stent then withdrawn immediately and inspected for damage. With the new and improved GuideLiner version 2.0, which is now widely available and currently in use at our center, the metal collar has been replaced by an all-polymer collar in order to reduce the risk of stent damage or dislodgement. This has avoided any further incidences of stents being stripped off; however, as with version 1.0, it is important to have the collar in a straight section of the guide catheter to permit easier passage of the device through the collar itself.
The majority of PCI cases undertaken at our center are performed transradially and, in this particular series, 76% of cases were performed via this route. Although the transradial approach is preferable to the transfemoral route owing to the significantly lower risks of bleeding complications, the likelihood of suboptimal guide catheter support is sometimes encountered more frequently with the transradial approach, particularly in the context of brachiocephalic tortuosity [20-22]. Therefore, the GuideLiner catheter is a particularly expedient device in centers, such as ours, that perform the majority of procedures transradially.
Since collecting the cases for this series, the center has used an additional 120 GuideLiner catheters over a 10-month period, which represents approximately 7% of all PCI procedures performed at our center over this time period.
Conclusion
This device evaluation effectively illustrates how the GuideLiner catheter can be successfully used to treat patients with challenging and complex coronary disease/anatomy in a safe and timely manner, either as a ‘bailout’ when conventional techniques have failed or at the start of the case when device delivery failure is anticipated. With the increasing age of the PCI population and the higher complexity of cases undertaken in many interventional centers, balloon and/or stent delivery failure will be encountered more frequently. Thus, the GuideLiner is an essential tool that can be utilized in standard PCI practice to effectively treat coronary lesions that may have previously been considered ‘untreatable’. The new modifications of the device have addressed some of its current limitations.
Future perspective
The GuideLiner has clearly established its position in the armory of the modern PCI operator.
The ease of use accompanied with the safety and efficacy profile have permitted widespread uptake across the world. The indications for use have also expanded and we have attempted to capture the majority in this article but, no doubt, further clinical scenarios will be documented in the future. The utilization of GuideLiner in the setting of retrograde chronically occluded vessels technique is a good example of this, whereby the externalization of the retrograde wire through the anterograde wire can be greatly facilitated.
The GuideLiner catheter is an important development that has certainly played a role in shaping the future of interventional cardiology.
Executive summary
Device characteristics
▪ The GuideLiner® (Vascular Solutions, MN, USA) catheter is a coaxial guide catheter extension, specifically designed for deep intubation of the target coronary artery, thereby permitting safe and effective device delivery during percutaneous coronary intervention.
▪ The soft-tipped extension is silicone coated for lubricity and comprises an inner polytetrafluoroethylene lining surrounded by a stainless steel coil for flexibility and strength.
▪ The GuideLiner travels through the Y-adaptor hemostasis valve without the need to disconnect the valve from the guide catheter, thereby providing the advantage of rapid exchange.
GuideLiner technique: step-by-step guide
▪ Advance the GuideLiner over its monorail system to the desired location within the vessel. Coaxial deep vessel intubation can be achieved by advancement over an uninflated balloon.
▪ Advance the coronary stent(s) into the guide catheter through the GuideLiner but be wary of resistance as the stent travels through the metal collar of the GuideLiner.
▪ Overlapping stents can be deployed from the distal to the proximal or from the proximal to the distal vessel using the GuideLiner.
▪ On completion of the procedure, gently pull the GuideLiner out under fluoroscopic guidance.
Clinical indications and applications
▪ Clinical indications and applications include the following:
– Distal stent delivery within a tortuous and/or calcified vessel.
– Distal stent delivery within a tortuous and/or calcified vessel after rotational or laser atherectomy.
– Failure to cross a calcified lesion with a balloon and/or stent without atherectomy.
– Inability to properly engage the guide catheter.
– Distal stent delivery without injuring the proximal vessel.
– Proximal to distal vessel stenting.
– Treatment of chronic total occlusions using the retrograde technique.
– Retrieval of a trapped rotablation burr.
Tips and tricks
▪ To facilitate coaxial and safe delivery of the GuideLiner within the distal vessel, the GuideLiner is usually best advanced over a balloon (uninflated or inflated).
▪ If a stent cannot advance to a distal position within the vessel and has to be deployed proximally, the GuideLiner can be advanced through the proximally deployed stent allowing the more distal lesion to subsequently be treated.
To avoid bulky stents being damaged or stripped off upon entering the metal collar of the GuideLiner, ensure that the metal collar is not positioned within a bend in the guide catheter.
▪ When dealing with calcific lesions that require debulking, small-diameter cutting balloons can be delivered through the GuideLiner. A rotablator cannot travel through the GuideLiner.
Device limitations and complications
▪ There is risk of:
– Proximal vessel dissection.
– Damage to larger, bulkier stents during their passage through the metal collar.
– Guidewire wrap.
New device components
▪ New device components include the following:
– An increased length of the rapid exchange section to allow deeper vessel intubation.
– An additional 5.5 Fr size.
– The metal collar changed to an all-polymer collar for improved flexibility.
– Additional proximal and distal marker bands.
Center-based discussion of the experiences encountered
▪ The GuideLiner was successful in 96% of cases and device-related procedural complications were encountered in 4% of cases.
▪ Two incidences of stent loss were encountered, both of which occurred during the passage of a 5-mm diameter stent within the metal collar of a 7 Fr GuideLiner.
Conclusion
▪ The GuideLiner catheter is an essential tool that can be successfully used to treat patients with challenging and complex coronary diseases/anatomies, either as a ‘bailout’ when conventional techniques have failed, or at the start of the case when device delivery failure is anticipated.
▪ The new modifications of the device have addressed some of its current limitations.
Future perspective
▪ The ease of use of the GuideLiner catheter, accompanied with its safety and efficacy profile, have permitted widespread uptake globally.
▪ The clinical indications for the GuideLiner are likely to expand in the future.
Financial and competing interests disclosure
P O’Kane is a European Proctor for Spectranetics. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
▪ of interest
▪▪ of considerable interest
- Jafary FH. When one won’t do it, use two-double ‘buddy’ wiring to facilitate stent advancement across a highly calcified artery. Catheter Cardiovasc. Interv. 67, 721–723 (2006).
- Burzotta F, Trani C, Mazzari MA et al. Use of a second buddy wire during percutaneous coronary interventions: a simple solution for some challenging situations. J. Invasive Cardiol. 17, 171–174 (2005).
- Hirokami M, Saito S, Muto H. Anchoring technique to improve guiding catheter support in coronary angioplasty of chronic total occlusions. Catheter Cardiovasc. Interv. 67, 366–371 (2006).
- Nikolsky E, Gruberg L, Pechersky S et al. Stent deployment failure: reasons, implications, and short- and long-term outcomes. Catheter Cardiovasc. Interv. 59, 324–328 (2003).
- Mamas MA, Fath-Ordoubadi F, Fraser DG. Distal stent delivery with Guideliner catheter: first in man experience. Catheter Cardiovasc. Interv. 76, 102–111 (2010).
- Pershad A, Sein V, Laufer N. GuideLiner catheter facilitated PCI – a novel device with multiple applications. J. Invasive Cardiol. 23, E254–E259 (2011).
- Rao U, Gorog D, Syzgula J, Kumar S, Stone C, Kukreja N. The GuideLiner ‘child’ catheter. EuroIntervention 6, 277–279 (2010).
- Kumar S, Gorog DA, Secco GG, Di Mario C, Kukreja N. The GuideLiner ‘child’ catheter for percutaneous coronary intervention – early clinical experience. J. Invasive Cardiol. 22, 495–498 (2010).
- Hanna EB, Dasari TW, Hennebry TA. Use of the GuideLiner catheter for the treatment of a bifurcational total occlusion of the native left anterior descending artery through a tortuous composite venous graft. J. Invasive Cardiol. 23, e40–e42 (2011).
- Wiper A, Mamas M, El-Omar M. Use of the GuideLiner catheter in facilitating coronary and graft intervention. Cardiovasc. Revasc. Med. 1(68), e5–e7 (2011).
- Luna M, Papayannis A, Holper EM, Banerjee S, Brilakis ES. Transfemoral use of the GuideLiner catheter in complex coronary and bypass graft interventions. Catheter Cardiovasc. Interv. 80, 437–446 (2012).
- de Man FH, Tandjung K, Hartmann M et al. Usefulness and safety of the GuideLiner catheter to enhance intubation and support of guide catheters: insights from the Twente GuideLiner registry. EuroIntervention 8, 336–344 (2012).
- Mamas MA, Fath-Ordoubadi F, Fraser D. Successful use of the Heartrail III catheter as a stent delivery catheter following failure of conventional techniques. Catheter Cardiovasc. Interv. 71, 358–363 (2008).
- Mamas MA, Eichhofer J, Hendry C et al. Use of the Heartrail II catheter as a distal stent delivery device; an extended case series. EuroIntervention 5, 265–271 (2009).
- Brilakis ES, Banerjee S. Novel uses of the Proxis embolic protection catheter. Catheter Cardiovasc. Interv. 74, 438–445 (2009).
- Banerjee S, Brilakis ES. Use of the Proxis embolic protection device for guide anchoring and stent delivery during complex saphenous vein graft interventions. Cardiovasc. Revasc. Med. 10, 183–187 (2009).
- Cunnington M, Egred M. GuideLiner, a child-in-a-mother catheter for successful retrieval of an entrapped rotablator burr. Catheter Cardiovasc. Interv. 79, 271–273 (2012).
- Cola C, Miranda F, Vaquerizo B, Fantuzzi A, Bruguera J. The Guideliner™ catheter for stent delivery in difficult cases: tips and tricks. J. Interv. Cardiol. 24, 450–461 (2011).
- Murphy JC, Spence MS. Guideliner catheter – friend or foe? Catheter Cardiovasc. Interv. 80, 447–450 (2012).
- Mamas MA, Ratib K, Routledge H et al. Influence of access site selection on PCI-related adverse events in patients with STEMI: meta-analysis of randomised controlled trials. Heart 98, 303–311 (2012).
- Jolly SS, Yusuf S, Cairns J et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet 377, 1409–1420 (2011).
- Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am. Heart J. 157, 132–140 (2009).
▪▪ Largest Guideliner® (Vascular Solutions, MN, USA) registry providing insights into the feasibility and safety of the device.
▪ First-in-man experience of the Guideliner catheter.
▪ Small GuideLiner case series incorporating tips and tricks for use of the device.