Case Report - International Journal of Clinical Rheumatology (2017) Volume 12, Issue 1
Subcutaneous panniculitis-like T cell lymphoma in a patient with juvenile idiopathic arthritis treated with Abatacept
- Corresponding Author:
- Stephen Boyle
Department of Rheumatology
Western General Hospital, Edinburgh
E-mail: boyledoc@yahoo.co.uk
Abstract
Subcutaneous panniculitis-like T-cell Lymphoma (SPTL) is a rare extranodal lymphoma that accounts for less than 1% of all Non-Hodgkin Lymphomas. We describe SPTL in a patient with Juvenile Idiopathic Arthritis (JIA) receiving Abatacept.
Keywords
subcutaneous panniculitis, like T cell lymphoma, abatacept, juvenile idiopathic arthritis
Case Report
A 35 year old female with JIA was diagnosed at eighteen months, initially oligoarticular, extending to a polyarticular pattern, with steroid dependent bilateral anterior uveitis necessitating immunosuppression. She received Abatacept infusions between December 2012 and July 2013. She had received numerous previous disease modifying agents including Sulfasalazine, Methotrexate, Hydroxychloroquine, Gold, Leflunamide, Adalimumab and Infliximab, which had been discontinued due to either intolerance or inefficacy.
In July 2013, she presented with a 3 month history of an enlarging anterior abdominal wall mass with no previous trauma and noted not to be a recent injection site and a swelling of similar consistency in the region of the right parotid gland. On examination she had a 2 × 4 cm non-tender, irregular lump on the lower left side of her abdomen, tethered to skin but mobile to underlying musculature. The 2 × 1 cm right parotid swelling was non-mobile and non-tender. There was no lymphadenopathy. An ultrasound showed normal parotid and submandibular salivary glands with the swelling within the fat layer with oedema and a slight increase in vascularity suggesting focal panniculitis.
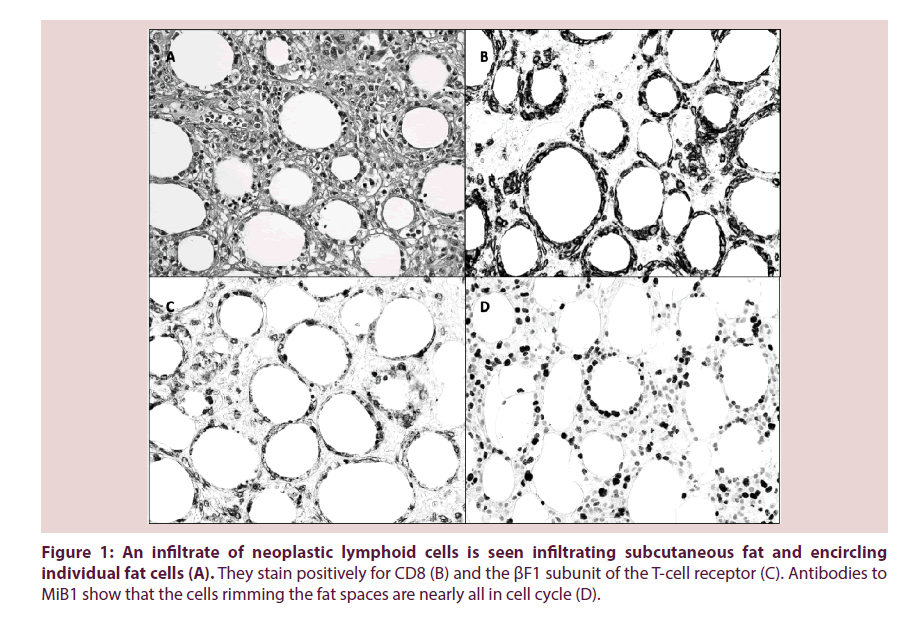
Biopsy of the abdominal mass showed characteristic features of SPTL (Figure 1).
Figure 1: An infiltrate of neoplastic lymphoid cells is seen infiltrating subcutaneous fat and encircling individual fat cells (A). They stain positively for CD8 (B) and the ßF1 subunit of the T-cell receptor (C). Antibodies to MiB1 show that the cells rimming the fat spaces are nearly all in cell cycle (D).
Bone marrow examination showed a reactive T-cell infiltrate, with no evidence of lymphomatous involvement. A Computerized Tomography (CT) scan of chest, abdomen and pelvis showed mild splenomegaly at 16 cm but no significant lymphadenopathy. A Positron Emission Tomography (PET) scan showed Fluorodeoxyglucose (FDG) avid disease in relation to the two masses only.
Treatment with prednisolone 60 mg daily resulted in size reduction of both masses. Repeat CT scan after 8 weeks showed almost complete resolution of the masses. A PET scan 6 weeks post steroids showed no evidence of active residual disease.
A period of watchful waiting was undertaken during which time the patient’s eye and joint disease had improved, however since discontinuation of prednisolone, her arthritis had become more active. She was treated with Rituximab.
SPTL, first described in 1991 by Gonzalez et al., occurs primarily in young adults but can arise at any age, more commonly in females [1]. Presentation is with subcutaneous nodules, usually localised to the extremities and trunk. Many patients display constitutional symptoms including weight loss, fever and fatigue. Splenomegaly may be present but is usually not due to lymphomatous involvement. 20% of patients have a pre-existing autoimmune disease, most commonly systemic lupus erythematosus [2], and a haemophagocytic syndrome is encountered in 15% to 20% [1-3].
Histologically, a lymphoid infiltrate is present in the subcutaneous tissue, predominantly in a lobular pattern. Dermal invasion is usually minimal or absent [3]. The neoplastic lymphocytes possess irregular hyperchromatic nuclei and indistinct cell borders, and typically encircle individual adipocytes. Admixed benign histiocytes, often containing nuclear debris, are usually present but plasma cells and neutrophils are rare or absent.
SPTL is a tumour of cytotoxic CD8+ T-cells with a α/β T cell phenotype. Historical series also included cases with a γ/δ T cell phenotype. However, these are usually negative for CD4 and CD8, often express CD56, are associated with a much poorer prognosis and are now classified as a distinct entity, primary cutaneous γ/δ T-cell lymphoma [2-5]. When such cases are excluded from analysis, SPTL has a relatively indolent course with a favourable prognosis, although the presence of a haemophagocytic syndrome is associated with a poorer outcome [2,3].
Clinically, the differential diagnosis includes reactive panniculitides such as erythema nodosum and erythema induratum. Pathologically, care must be taken to distinguish SPTL from lupus profundus, Borrelia-associated panniculitis and other lymphomas that frequently infiltrate subcutaneous fat, including the aforementioned primary cutaneous γ/δ T-cell lymphoma and extranodal NK/T-cell lymphoma, nasal type.
Treatments vary from radiotherapy, corticosteroids or anthracycline based chemotherapy [3,6]. Our patient was treated with prednisolone only, achieved a complete response and currently remains in remission with 5 months follow-up.
Conclusion
In our patient, concerns were raised regarding the role Abatacept may have played in the development of her SPTL. Abatacept is a soluble fusion protein that selectively modulates the CD80/CD86:CD28 co-stimulatory signal required for full T cell activation. The efficacy and safety of Abatacept has been demonstrated in children and adolescents with JIA [7]. A long term, open-label extension phase of a double blind randomised controlled trial in 190 patients with JIA aged 6-17 years receiving Abatacept for 21 months or more showed a favourable safety profile. No malignancies were reported [8]. Our patient is an adult with JIA who received Abatacept during the 7 months before the SPTL diagnosis, and although the after mentioned paper describes children and adolescents, in the absence of literature regarding Abatacept safety in adults with JIA, we can only infer a similar safety profile.
This case emphasises the importance of maintaining vigilance for new or unusual symptoms on biologics and obtaining a tissue diagnosis where possible.
References
- Gonzalez CL, Medeiros LJ, Braziel RMet al.T cell lymphoma involving subcutaneous tissue: a clinicopathologic entity commonly associated withhemophagocytic syndrome. Am. J. Surg. Pathol. 15, 17-27 (1991).
- Jaffe ES, Gaulard P, Ralfkiaer E et al. Subcutaneous panniculitis-like T-celllymphoma. In: WHO Classification of Tumours of Haematopoietic and LymphoidTissues. Lyon: International Agency for Research on Cancer. 294-295 (2008).
- Willemze R, Jansen PM, Cerroni Let al. Subcutaneous panniculitis-like T-celllymphoma: definition, classification, and prognostic factors: an EORTC CutaneousLymphoma Group Study of 83 cases. Blood. 111, 838-845 (2008).
- Salhany KE, Macon WR, Choi JK et al. Subcutaneous panniculitis-like T-celllymphoma: clinicopathologic, immunophenotypic, and genotypic analysis ofalpha/beta and gamma/delta subtypes. Am. J. Surg. Pathol.22, 881-893 (1998).
- Massone C, Lozzi GP, Egberts Fet al. The protean spectrum of non- Hodgkinslymphomas with prominent involvement of subcutaneous fat. J. Cutan. Pathol. 33, 418-425 (2006).
- Go RS, Wester SM. Immunophenotypic and molecular features, clinical outcomes,treatments, and prognostic factors associated with subcutaneous panniculitis-likeT-cell lymphoma: a systematic analysis of 156 patients reported in the literature. Cancer. 101, 404-413 (2004).
- Ruperto N, Lovell DJ, Quartier P et al. Abatacept in children with juvenileidiopathic arthritis:a randomised, double-blind, placebo-controlled withdrawal trial.Lancet. 372, 383-391 (2008).
- Ruperto N, Lovell DJ, Quartier Pet al. Long-Term Safety and Efficacy ofAbatacept in Children with Juvenile Idiopathic Arthritis. Arthritis. Rheum. 62(6), 1792-1802 (2010).