Research Article - Interventional Cardiology (2021) Volume 13, Issue 4
Speckle tracking right ventricular myocardial strain post-percutaneous closure of atrial septal defects in children
- Corresponding Author:
- Fatma Aboalsoud Taha
Department of Cardiology,
Tanta University,
Algesh Street,
Tanta,
Gharbeya,
Egypt ,
E-mail: fatmastaha@yahoo.com
Received date: May 31, 2021; Accepted date: June 14, 2021; Published date: June 21, 2021
Abstract
Background: Atrial Septal Defects (ASDs) can induce Right Ventricular (RV) volume overload and dysfunction. The RV has complex morphology; thus makes the quantitative assessment of its function challenging. Speckle tracking Global Longitudinal Strain (GLS) could be applied to estimate RV function. This study aimed to evaluate the changes in RV myocardial function by 2D speckle tracking global longitudinal strain in children with secundum ASD pre- and 3-month post-percutaneous device closure.
Methods and findings: Thirty-one children who underwent percutaneous ASD closure were prospectively examined. LV Ejection Fraction (EF), Estimated Systolic Pulmonary Artery Pressure (ESPAP), Tricuspid Annulus Plane Systolic Excursion (TAPSE), Fractional Area Change (FAC), and RV-GLS were calculated and analyzed prior- and 3-month after device closure. The mean age of patients was 8.15 ± 3.43 years with a mean weight of 17.31 Kg. ± 6.17 Kg. Sixteen (51.61%) patients were females. The pulmonary to systemic blood flow (QP/QS) ratio was 1.6 ± 0.56. The vertical, horizontal, and oblique diameters of the ASD were 15.06 mm ± 4.95 mm, 12.84 mm ± 3.12 mm, and 16.17 mm ± 4.29 mm respectively, and the device diameter was 16.94 mm ± 4.80 mm. After 3-month, there was a significant decrease in RA diameters, RV diameters, and ESPAP (P<0.001). TAPSE increased significantly from 14.32 mm ± 1.44 mm to 20.32 mm ± 1.57 mm (P<0.001), FAC enhanced significantly from 33.31% ± 11.14% to 39.15% ± 18.17 %, and RVGLS improved significantly from -17.26% ± 2.32% to -24.79% ± 3.41% (P<0.001). There were negative correlations between RV-GLS with RA diameters, RV diameters, and ESPAP (P<0.05), and positive correlations between RV-GLS with TAPSE, and FAC (P<0.05).
Conclusion: Speckle tracking-based GLS is a quantitative calculator of the subtle RV function impairment in children with ASDs that showed significant improvement to normal values in mid-term 3-month follow-up post-percutaneous device closure. Such a validated tool can be used in volume overloaded conditions to predict early ventricular dysfunction and to guide the initiation of percutaneous closure management strategy.
Keywords
Right ventricular myocardial strain • Speckle tracking echocardiography • Speckle strain in children • The global longitudinal strain of the right ventricle • Percutaneous atrial septal defect closure
Introduction
Atrial Septal Defects (ASDs) are common congenital heart defects in children. Ostium secundum ASDs are the most common type of ASDs, accounting for 70% of all ASDs and 6%-10% of all Congenital Heart Diseases (CHDs) [1]. Large ASDs, with a leftto- right shunt, are the most common cause of volume overload of the Right Ventricle (RV) and can induce RV dysfunction. Also, the Right Atrial (RA) diameters and volume are augmented in ASD patients with volume overload [2].
Mostly, secundum ASDs are centrally located and are bounded by rims that often make these defects suitable for percutaneous device closure that becomes a routine intervention in children with secundum ASDs [3]. Transcatheter implantation of an occluder in the atrial septum is associated with improvement in RV dimensions, morphology, remodeling, contraction, and function, especially in younger children [4,5].
RV has a complex anatomy and morphology; thus, quantitative assessment of RV function is challenging and problematic, and therefore not included in daily clinical practice. Two-dimensional (2D) Speckle Tracking Echocardiography (STE) has developed as a valuable tool to assess global and regional myocardial deformation [6,7]. 2D Myocardial speckle tracking Strain (S) and Strain Rate (SR) are consistent Doppler and angle-independent techniques that measure ventricular geometry and myocardial deformation. This echocardiographic technique permits noninvasive and quantitative assessment of global and regional myocardial function [8-10]. Myocardial Global Longitudinal Strain (GLS) can be able to assess RV myocardial function. While this method has been frequently used to estimate LV function, it has rarely been used to examine the RV function. However, RV myocardial function is important to be assessed to judge prognosis in patients with congenital heart disease [10,11].
This study aimed to evaluate the changes in right ventricular myocardial function by 2D speckle tracking global longitudinal strain in children with secundum ASD pre- and 3-month postpercutaneous device closure.
Materials and Methods
Patients
This is a prospective controlled study that started from November 2017 to October 2019. The study enrolled forty-one children <14 years old, with amenable ostium secundum ASDs for device closure and who had significantly hemodynamic left-to-right shunt, RV volume overload, or shunt-related symptoms. Children with other CHDs, sinus venosus ASDs, primum type ASDs, coronary sinus defects, insufficient atrioventricular rim <7 mm, and severe pulmonary hypertension were excluded from the study.
All patients in this study were evaluated by clinical, echocardiographic examinations before and 3 months after the percutaneous ASD device closure with different septal occluders. This study has been performed in accordance with Helsinki Declaration of the World Medical Association in 1975 as revised in 2008 concerning Human Rights under the approval of the ethics committee. Informed written consent was obtained from all patients’ guardians before the procedure, and, also, informed consent for participation was obtained.
Echocardiography
All patients underwent complete transthoracic echocardiography (TTE) examinations according to the American Society of Echocardiography (ASE) guidelines [12] using an ultrasound system; the General Electric (GE) VIVID 9 ultrasound (Horten, Norway) equipped with a multifrequency transducer probe (3 MHz-8 MHz). The echocardiographic examination was done at rest and children who were unable to completely rest during imaging were given light sedation.
The suitability for transcatheter closure was examined by a thorough examination of the six rims surrounding the defect; the Superior Vena Cava (SVC) rim, the Inferior Vena Cava (IVC) rim, the aortic anterior rim, the posterior rim, the superior rim towards the Right Upper Pulmonary Vein (RUPV), and the atrioventricular (AV) rim towards AV valves. At least a 5 mm length of all rims in all planes, besides a 7 mm distance from the mitral valve to the defect was required. The diameters of ASD were determined; the vertical diameter between SVC and IVC rims in subcostal bicaval view, the horizontal diameter between the anterior aortic and the posterior rims in parasternal short-axis view, and the oblique diameter between the superior and atrioventricular rims in apical four-chamber view.
The left to right shunt was assessed by the ratio of total pulmonary blood flow to total systemic blood flow (QP/QS) ratio and was calculated by two-dimensional echocardiography. QP/QS ratio was measured by the equation; Pulmonary Valve Annulus (PVA) × Pulmonary artery velocity time integral (PVTI)/Aortic Valve Annulus (AVA) × Aorta velocity integral (AOVI). Initially, patients with a QP/QS ratio of ≥ 1.5 underwent catheterization. Automated left ventricular Ejection Fraction (EF) was obtained by the modified biplane Simpson’s rule. Estimated Systolic Pulmonary Artery Pressure (ESPAP) was evaluated by Doppler measuring of Tricuspid Regurgitation (TR) jet velocity by applying the modified Bernoulli equation to convert this value into pressure values, followed by adding estimated Right Atrial Pressure (RAP) to this obtained value [ESPAP=TR gradient+RA pressure (RAP)]. The long- and short-axis diameters of the RA and the RV were estimated in the apical four-chamber view. RV Tricuspid Annulus Plane Systolic Excursion (TAPSE) was defined as the excursion of the tricuspid annulus from the base to the apex in systole and was calculated using M-mode in the apical 4-chamber view with the cursor positioned on the lateral aspect of the tricuspid valve at the RV free wall. Fractional Area Change (FAC) was estimated by subtracting where RV End-Systolic Area (RVESA) from RV End-Diastolic Area (RVEDA) and dividing it by RVEDA [FAC=RVEDA-RVESA/RVEDA].
Speckle tracking strain curves
Electrocardiogram was contacted to the patient’s chest till proper adjustment of the heart rate recording on the echocardiography machine. A frame rate of 80-100 frames/sec was utilized for storage and analysis. At least three consecutive cardiac cycles of 2D apical four-chamber images were recorded at each plane and were imported into the GE EchoPAC (BT 09, Horten, Norway) workstation to select the best speckle tracking analysis images. The images were optimized to visualize the myocardial walls.
Two-dimensional speckle tracking offline analysis software was automatically tracked the endocardial, epicardial borders, and the myocardial movement of the RV frame by frame, thus delineating a region of interest composed of six segments including apical, mid-, and basal free wall and apical, mid-, and basal septal walls. The analysis was established when adequate tracking was ensured by visual inspection and by the software. If the RV endocardium tracking was unsatisfactory, manual modification of the region of interest size was achieved to confirm optimum tracking. RV longitudinal strain curves were created for each segment by the software. Once approved, the software displayed an average of the strain curves of the six RV segments, which is the GLS to assess the global RV myocardial function automatically [11,13,14]. All echocardiographic measures were performed before device closure and 3-months after device implantation and then reported and analyzed.
Percutaneous ASD closure procedure
All procedures were carried out under general anesthesia utilizing fluoroscopic and TTE guidance. In those patients with a poor echo window, Trans Esophageal Echocardiography (TEE) was done to delineate the ASD rims and to guide the transcatheter procedure.
Firstly, the magnitude of the left to right shunt was assessed by invasively estimated QP/QS ratio to ensure significant volume overload (Invasively estimated QP/QS ratio=Aorta saturation- SVC saturation/pulmonary veins saturation-pulmonary artery saturation). Patients with a non-significant shunt; QP/QS ratio <1.5, despite undergoing percutaneous closure, were excluded from the study.
Different septal occluders were used; Amplatzer™ septal Occluder (Abbott), Occlutech® Figulla® Flex II Septal Occluder (Jena, Germany), Hyperion™ ASD Occluder (Comed), Cocoon Septal Occluder (CSO), and Cera Flex™ ASD Occluder. The septal occluder size was 2 mm larger than the largest diameter of the ostium secundum ASD. Post-interventional treatment included 5 mg/kg/day of acetylsalicylic acid for 6 months.
Statistical analysis
Statistical analysis was approved with the SPSS statistical package (Version 25; SPSS Inc., Chicago, IL, USA). Quantitative data were expressed as mean ± Standard Deviation (SD), and Qualitative data were expressed using numbers and percentages. Differences between baseline and follow-up data were analyzed by the paired sample t-test. Pearson’s correlation was employed to determine the relationship between RV-GLS and other echocardiographic parameters. A P-value <0.05* was considered statistically significant at a confidence interval of 95%.
Results
Demographic and clinical characteristics
Despite the non-invasive QP/QS ratio was 1.7 ± 1.69 by echocardiography and lead 41 children to undergo percutaneous device closure, ten of them were excluded from the study because they displayed a non-significant hemodynamic left to right shunt with an invasive QP/QS ratio <1.5. In this study, we report on the remaining 31 children, with a mean invasively estimated QP/ QS ratio of 1.6 ± 0.56. The mean age of the included patients was 8.15 ± 3.43 years, the mean weight was 17.31 ± 6.17 Kg, and the mean Body Surface Area (BSA) was 0.71 m2 ± 0.12 m2. Sixteen (51.61%) patients were females and 15 (48.39%) patients were males. Twenty-one (67.74%) patients presented with dyspnea grade II-IV, 8 (25.81%) patients presented with repeated attacks of chest infection, and 2 (6.45%) patients presented with low weight for age, with no patient exhibited arrhythmias. Most, 27 (87.1%) patients had ejection systolic murmur on the second left intercostal space. There was an increased heart rate with a mean of 117 bpm ± 11 bpm. The demographic and the clinical characteristics of the studied children were shown in Table 1.
| Characteristics | N=31 patients |
|---|---|
| Age (years) | 8.15 ± 3.43 |
| <5 years | 6 (19.35%) |
| 5 - 10 years | 14 (45.16%) |
| 10-14 years | 11 (35.48%) |
| Gender | |
| Male | 15 (48.39%) |
| Female | 16 (51.61%) |
| Weight (kg) | 17.31 ± 6.17 |
| Body surface area (BSA) (m2) | 0.71 ± 0.12 |
| Presentation | |
| Dyspnea grade II-IV | 21 (67.74%) |
| Repeated attacks of chest infection | 8 (25.81%) |
| Low weight for age | 2 (6.45%) |
| Arrhythmias | 0 (0%) |
| Ejection systolic murmur on the second left intercostal space | 27 (87.1%) |
| Heart rate (bpm) | 117 ± 11 |
Table 1: Demographic and clinical characteristics of the studied patients.
Echocardiographic data
The mean native diameters of the secundum ASD on color Doppler echocardiographic evaluation were 15.06 mm ± 4.95 mm, 12.84 mm ± 3.12 mm, and 16.17 mm ± 4.29 mm for vertical, horizontal, and oblique diameters respectively. Most 24 (77.42 %) patients had sufficient all ASD rims >5 mm for each, except 4 (12.9 %) patients had deficient posterior rims and 3 (9.7 %) patients had deficient superior rims.
By the end of the 3-month follow-up, there was a significant fall of ESPAP; from 31.55 mmHg ± 3.17 mmHg to 20.71 mmHg ± 3.24 mmHg, with a P-value<0.001*. However, LVEF showed no significant change with a pre-closure measure of 67.44% ± 4.64% vs. a post-closure measure of 67.74% ± 4.78%, with a P-value of 0.071.
Three-month post-percutaneous closure, RA diameters decreased significantly; 35.83 mm ± 4.39 mm vs. 31.90 mm ± 3.70 mm for long axis (P<0.001*), and 31.11 mm ± 3.94 mm vs. 25.41 mm ± 3.83 mm for short axis (P<0.001*). Also, RV end-diastolic diameters were decreased significantly; 46.24 mm ± 7.15 mm vs. 38 mm ± 4.60 mm for long axis (P <0.001*), and 30.19 mm ± 3.83 mm vs. 25.46 mm ± 3.47 mm for short axis (P<0.001*). Three-month post-percutaneous closure, TAPSE increased significantly from 14.32 mm ± 1.44 mm to 20.32 mm ± 1.57 mm (P<0.001*), also, FAC increased significantly from 33.31% ± 11.14% to 39.15% ± 18.17% (P<0.001*). The echocardiographic measurements pre and 3-month post-percutaneous ASD device closure were provided in Table 2.
| Pre-procedure | 3-month Post-procedure | P-value of paired sample t-test | P-value of Pearson’s correlation test | |
|---|---|---|---|---|
| ASD diameters (mm) | ||||
| Vertical | 15.06 ± 4.95 | |||
| Horizontal | 12.84 ± 3.12 | |||
| Oblique | 16.17 ± 4.29 | |||
| ASD rims (mm) | ||||
| Sufficient all rims | 24 (77.42 %) | |||
| Deficient posterior rim | 4 (12.9 %) | |||
| Deficient superior rim | 3 (9.7 %) | |||
| QP/QS ratio by echocardiography | 1.7 ± 1.69 | |||
| LVEF (%) | 67.44 ± 4.64 | 67.74 ± 4.78 | 0.071 | 0.067 |
| ESPAP (mmHg) | 31.55 ± 3.17 | 20.71 ± 3.24 | <0.001* | 0.025* |
| RA diameters (mm) | ||||
| Long axis | 35.83 ± 4.39 | 31.90 ± 3.70 | <0.001* | 0.012* |
| Short axis | 31.11 ± 3.94 | 25.41 ± 3.83 | <0.001* | 0.017* |
| RV end-diastolic diameters (mm) | ||||
| Long axis | 46.24 ± 7.15 | 38.74 ± 4.60 | <0.001* | 0.001* |
| Short axis | 30.19 ± 3.83 | 25.46 ± 3.47 | <0.001* | 0.001* |
| TAPSE (mm) | 14.32 ± 1.44 | 20.32 ± 1.57 | <0.001* | 0.003* |
| FAC (%) | 33.31 ± 11.14 | 39.15 ± 18.17 | <0.001* | <0.001* |
| RV global longitudinal strain (GLS) (%) | -17.26 ± 2.32 | -24.79 ± 3.41 | <0.001* | |
Abbreviations: ASD: Atrial Septal Defect; ESPAP: estimated systolic pulmonary artery pressure; FAC: Fractional Area Change; GLS: Global Longitudinal Strain; LVEF: Left Ventricular Ejection Fraction; QP/QS ratio: Total pulmonary blood flow/Total systemic blood flow ratio, RV: Right Ventricle, TAPSE: Tricuspid Annulus Plane Systolic Excursion, *: Significant P-value <0.05.
Table 2: Echocardiographic parameters and right ventricular (RV) global longitudinal strain (GLS) pre and 3-month post Atrial Septal Defects (ASDs) closure of the studied patients.
Speckle tracking global longitudinal strain analysis
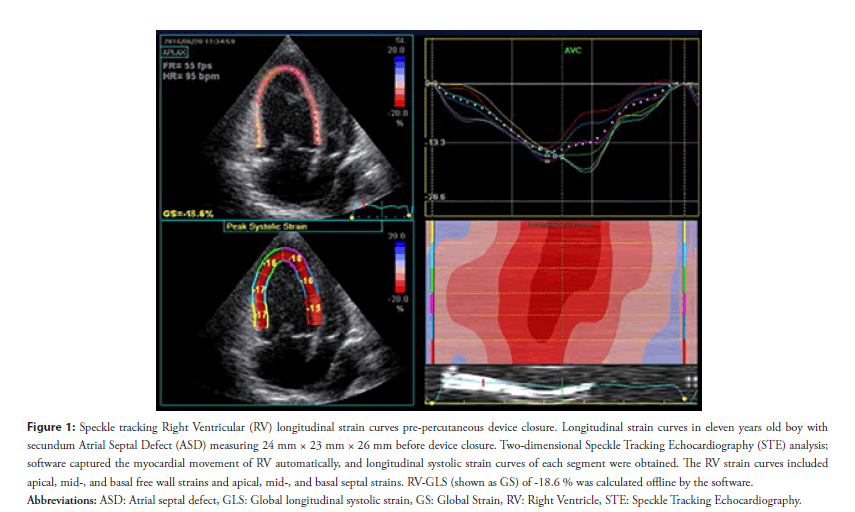
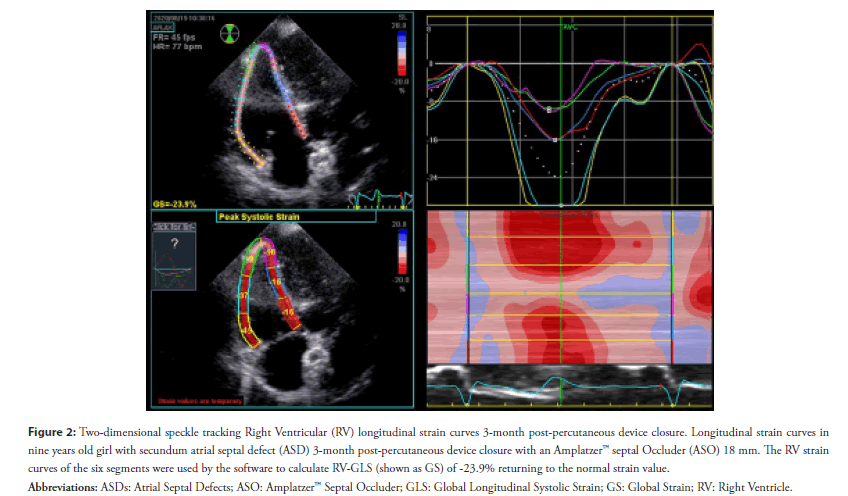
Three-month post ASD device closure, RV-GLS improved significantly from -17.26% ± 2.32% to -24.79% ± 3.41% (P<0.001*) [Figure (1), and Figure (2) showed speckle tracking RV global longitudinal strain in two children with secundum ASDs pre and 3-month post device closure respectively]. Correlation analysis was measured using those changes post- and pre-ASD parameters. The correlation analysis showed a significant negative correlation between RV-GLS with RA diameter (P=0.012* for long axis, and 0.017* for short axis), RV diameter (P<0.001* for long and short axes), and ESPAP (P=0.025*). Also, there was a significant positive correlation between RV-GLS with TAPSE (P=0.003*) and FAC (P<0.001). However, there was no significant correlation among RV-GLS with LV Ejection Fraction (LVEF) (P=0.067) (Table 2).
Figure 1: Speckle tracking Right Ventricular (RV) longitudinal strain curves pre-percutaneous device closure. Longitudinal strain curves in eleven years old boy with
secundum Atrial Septal Defect (ASD) measuring 24 mm × 23 mm × 26 mm before device closure. Two-dimensional Speckle Tracking Echocardiography (STE) analysis;
software captured the myocardial movement of RV automatically, and longitudinal systolic strain curves of each segment were obtained. The RV strain curves included
apical, mid-, and basal free wall strains and apical, mid-, and basal septal strains. RV-GLS (shown as GS) of -18.6 % was calculated offline by the software.
Abbreviations: ASD: Atrial septal defect, GLS: Global longitudinal systolic strain, GS: Global Strain, RV: Right Ventricle, STE: Speckle Tracking Echocardiography
Figure 2: Two-dimensional speckle tracking Right Ventricular (RV) longitudinal strain curves 3-month post-percutaneous device closure. Longitudinal strain curves in
nine years old girl with secundum atrial septal defect (ASD) 3-month post-percutaneous device closure with an Amplatzer™ septal Occluder (ASO) 18 mm. The RV strain
curves of the six segments were used by the software to calculate RV-GLS (shown as GS) of -23.9% returning to the normal strain value.
Abbreviations: ASDs: Atrial Septal Defects; ASO: Amplatzer™ Septal Occluder; GLS: Global Longitudinal Systolic Strain; GS: Global Strain; RV: Right Ventricle.
Procedural data
Percutaneous secundum ASD closure was performed successfully in all patients. The mean diameter of the ASD devices used was 18.14 mm ± 4.90 mm; <15 mm devices were used in 11 (35.5%) patients, 15 mm-20 mm devices were used in 11 (35.5%) patients, and >20 mm devices were used in 9 (29.0%) patients. There was no residual ASD observed in any of the patients on echocardiographic evaluations immediately and at 3-month post device closure.
Amplatzer™ septal Occluder (Abbott) was used in 11 (35.5%) patients, Hyperion™ ASD Occluder (Comed) was used in 6 (19.4%) patients, Occlutech® Figulla® Flex II Septal Occluder (Jena, Germany) was used in 5 (16.1%) patients, Cocoon Septal Occluder (CSO) was used in 5 (16.1 %) patients, and Cera Flex™ ASD Occluder was used in 4 (12.9%) patients. The catheterization and the procedural data of the studied patients were shown in Table 3.
| Parameter | N=31 |
|---|---|
| Invasively estimated QP/QS ratio | 1.6 ± 0.56 |
| Septal Occluder (ASD device) type | |
| AMPLATZER™ (ASO) | 11 (35.5 %) |
| Hyperion™ ASD Occluder Comed | 6 (19.4%) |
| Occlutech® Figulla® Flex II ASD | 5 (16.1 %) |
| Cocoon (CSO) | 5 (16.1%) |
| Cera Flex™ ASD | 4 (12.9%) |
| Septal Occluder (ASD device) size (mm) | 18.14 ± 4.90 |
| <15 | 11 (35.5 %) |
| 15-20 | 11 (35.5 %) |
| >20 | 9 (29.0 %) |
Abbreviations: ASD: Atrial Septal Defect, ASO: AMPLATZER™ Septal Occluder, CSO: Cocoon Septal Occluder; QP/QS ratio: Total pulmonary blood flow/Total systemic blood flow ratio.
Table 3: Catheterization and procedural data of the studied patients.c
Discussion
Changes in right heart volumes
Assessment of the RV myocardial volume and function is greatly important to determine prognosis and is an independent predictor of cardiovascular morbidity and mortality in patients with left to right intra-cardiac shunts and pulmonary arterial hypertension [15].
This study demonstrated a significant reduction in RV and RA dimensions at 3-month follow-up and this was in the conjunction with the following studies: Ding, et al, found that RV volumes markedly decreased in the first month after transcatheter ASD closure [16]. Also, Akula, et al, showed that RV volumes significantly diminished one month after ASD device closure and returned to near normal values within the first 6 months [17]. Veldtman, et al. found that right heart morphology experienced rapid improvement in the first month after percutaneous ASD closure [18]. Atashband, et al. showed that percutaneous ASD closure in adults is effective with reverse remodeling and better functional capacity [19]. ThileÌn, et al. found that cardiac remodeling was completed within the first 6 months after closure [20]. This can be explained by the reduction of the left to right shunt overload on the RV after transcatheter device closure of atrial septal defect that subsequently reduces RV dimensions and volumes in the mid-term outcome.
Changes in right ventricular Global Longitudinal Strain (GLS)
As the quantitative assessment of the RV function is challenging and problematic and with the comparison to the assessment of global LV myocardial function by two-dimensional (2D) Speckle Tracking Echocardiography (STE), there was some evidence in support of the use of RV-GLS calculation for the RV free wall with a normal reference value of >-20% [21-23]. STE has the advantage of measuring actual tissue deformation within the myocardium, and so, global and regional myocardial function [19]. Despite, speckle tracking-based strain echocardiography is a modality that improves the understanding of cardiac functions; the parameters for assessment are yet to be standardized for the pediatric age group [21].
In this study, we estimated the changes in RV myocardial function by 2D speckle tracking GLS in children with secundum ASD pre- and 3-month post-percutaneous device closure. There was a statistically significant improvement in RV-GLS to near normal values at 3-month post percutaneous ASD device closure. The reduction of the RV dimensions post-percutaneous ASD closure, allowed the RV strains to improve and return to the near-normal values. Our study was in agreement with Ozturk and colleagues who showed that volume overload-induced by ASD was associated with worsened strain values, which returned to normal in shortterm follow-up after closure with a significant reduction in RV volumes and a significantly improved RV longitudinal strain [24]. However, their research objects were adults, and the examinations were performed shortly 1 month after the ASD procedure. In our study, we examined the children’s age group and further explored the changes to 3 months post device closure.
Few studies used STE to evaluate RV deformation in children. The results of our current study were in agreement with Ko, et al, who recognized the occurrence of RV free wall longitudinal deformation in a relatively accepted number of children with ASD. They found that the basal segment deformation values in pre-closure ASD children were impaired than the post-closure values and that these post-closure results were not different from controls [25]. Also, Agha and colleagues who estimated changes in RV dimensions and function after transcatheter ASD device closure in children with secundum ASD, stated that there was a significant decrease in the RVEDV (from 54.65 mL ± 10.05 mL to 15.73 mL ± 8.67 mL) and a significant improvement in the RVGLS (from -20.17% ± 3.14% to -25.86% ± 5.02%, p<0.0001) 6 months post-ASD closure [26].
In the current study, we did not examine the immediate or the 24 hours changes in RV volumes and function. Some studies showed an acute worsening of RV-GLS 24 hours after ASD device closure that returns to normal or near-normal values in short-term followup. This can be explained by the increased contractility from RV volume loading before ASD closure that decreased immediately with an acute and temporary reduction of RV-GLS. Bussadori, et al. studied 18 children who underwent percutaneous ASD closure and showed worsening of RV-GLS 24 hours after ASD closure [27]. Also, Xu, et al. who studied 30 children with percutaneously closed ASD, demonstrated that the implantation of the occluder in the atrial septum causes an acute decrease in deformation of all RV wall motion and RV-GLS, which improved after 3-month of follow-up [28].
In this study, there was a positive correlation between RV-GLS with TAPSE and FAC. Also, we found a negative correlation between RV-GLS with RV diameters, RA diameters, and ESPAP. A previous study had also demonstrated similar findings but in adult patients with secundum ASD [24].
Finally, our findings can lead to the evolution of the GLS as a non-invasive tool for the objective assessment of the subtle RV myocardial deformation in children with ASD that can predict early RV dysfunction and can guide the initiation of percutaneous closure management strategy. Being an objective assessment, this non-invasive method is free from performance variability among echocardiographers conferring it a universally accepted tool in detecting changes in the RV function during short- and mid-term follow-up of children with ASDs.
Conclusion
In children with ASDs, the long-term volume overload was accompanied by decreased strain values and RV function. Twodimensional (2D) speckle-tracking Global Longitudinal Strain (GLS) measurement was able to estimate the subtle impairment in the global RV myocardial function that showed significant improvement to normal values in mid-term 3-month follow-up post-percutaneous device implantation. Therefore, GLS can be considered a quantitative and objective calculator of global RV myocardial function in children with ASDs. Such a validated tool can be used in volume overloaded conditions to predict early ventricular dysfunction and to guide the initiation of percutaneous closure management strategy.
Study Limitations
There are some limitations to this study. The sample size was unable to perform a subgroup analysis of RV function based on ASD size and shunt magnitude. Finally, more cases are warranted in future studies to validate our findings and evaluate the effect of the device closure on RV function in children.
Conflict of Interest
No conflicts of interest.
Human Rights and Informed Consent
This study has been performed in accordance with Helsinki Declaration of the World Medical Association in 1975 as revised in 2008 concerning Human Rights under the approval of the ethics committee. Informed written consent was obtained from all patients’ guardians before the procedure, and, also, informed consent for participation was obtained.
References
- Hijazi ZM, Hellenbrand WE. The right ventricle in congenital heart disease. Cardiol Clin. 10: 91-110 (1992).
- Bhatt AB, Landzberg MJ, Wu FM. Atrial Septal Defect. In: Craw-ford MH, DiMarco JP, Paulus WJ, editors. Cardiology. 3rd ed. Philadelphia p.1441-6 (2010).
- Ueda H, Yanagi S, Nakamura H, et al. Device closure of atrial septal defect: Immediate and mid-term results. Circ J. 76(5): 1229-34 (2012).
- Walker RE, Moran AM, Gauvreau K, et al. Evidence of adverse ventricular interdependence in patients with atrial septal defects. Am J Cardiol. 93(11): 1374-7 (2004).
- Stern H, Baurecht H, Luechinger R, et al. Does the amplatzer septal occluder device alter ventricular contraction pattern? A ventricular motion analysis by MR tagging. J Magn Reson Imaging. 35(4): 949-56 (2012).
- Friedberg MK, Mertens L. Tissue velocities, strain, and strain rate for echocardiographic assessment of ventricular function in congenital heart disease. Eur J Echocardiogr. 10(5): 585-93 (2009).
- Chow PC, Liang XC, Cheung EW, et al. New two-dimensional global longitudinal strain and strain rate imaging for assessment of systemic right ventricular function. Heart. 94(7): 855-9 (2008).
- Pettersen E, Fredriksen PM, Urheim S, et al. Ventricular function in patients with transposition of the great arteries operated with arterial switch. Am J Cardiol. 104: 583-9 (2009).
- Knirsch W, Dodge-Khatami A, Kadner A, et al. Assessment of myocardial function in pediatric patients with operated tetralogy of Fallot: preliminary results with 2D strain echocardiography. Pediatr Cardiol. 29(4): 718-25 (2008).
- Perk G, Tunick PA, Kronzon I. Non-Doppler two-dimensional strain imaging by echocardiography-from technical considerations to clinical applications. J Am Soc Echocardiogr. 20(3): 234-43 (2007).
- Vitarelli A, Sardella G, Di-Roma A, et al. Assessment of right ventricular function by three-dimensional echocardiography and myocardial strain imaging in adult atrial septal defect before and after percutaneous closure. Int J Cardiovasc Imaging. 28(8): 1905-16 (2012).
- Lopez L, Colan SD, Frommelt PC, et al. Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr. 23(5): 465-95 (2010).
- Voigt JU, Pedrizzetti G, Lysyansky P, et al. Definitions for a common standard for 2D speckle tracking echocardiography: Consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. J Am Soc Echocardiogr. 16(1): 1-11 (2015).
- Aslan M, Erturk M, Turen S, et al. Effects of percutaneous closure of atrial septal defect on left atrial mechanical and conduction functions. Eur Heart J Cardiovasc Imaging. 15(10): 1117-24 (2014).
- Favot M, Courage C, Ehrman R, et al. Strain echocardiography in acute cardiovascular diseases. West J Emerg Med. 17(1): 54-60 (2016).
- Ding J, Ma G, Wang C, et al. Acute effect of transcatheter closure on right ventricular function in patients with atrial septal defect assessed by tissue Doppler imaging. Acta Cardiol. 64(3): 303-9 (2009).
- Akula VS, Durgaprasad R, Velam V, et al. Right ventricle before and after atrial septal defect device closure. Echocardiography. 33(9): 1381-8 (2016).
- Veldtman GR, Razack V, Siu S, et al. Right ventricular form and function after percutaneous atrial septal defect device closure. J Am Coll Cardiol. 37(8): 2108-13 (2001).
- Atashband A, Lakkis N. First comprehensive analysis of outcomes in adult patients after percutaneous closure of isolated secundum atrial septal defects. Cardiovasc Hematol Agents Med Chem. 13: 63-9 (2015).
- ThileÌn U, Persson S. Closure of atrial septal defect in the adult. Cardiac remodeling is an early event. Int J Cardiol. 108(3): 370-5 (2006).
- Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 16(3): 233-70 (2015).
- Kjaergaard J, Sogaard P, Hassager C. Quantitative echocardiographic analysis of the right ventricle in healthy individuals. J Am Soc Echocardiogr. 19(11): 1365-72 (2006).
- Jategaonkar SR, Scholtz W, Butz T, et al. Two-dimensional strain and strain rate imaging of the right ventricle in adult patients before and after percutaneous closure of atrial septal defects. Eur J Echocardiogr. 10(4): 499-502 (2009).
- Ozturk O, Ozturk U, Zilkif M. Assessment of right ventricle function with speckle tracking echocardiography after the percutaneous closure of atrial septal defect. Acta Cardiol Sin. 33(5): 523-9 (2017).
- Ko HK, Yu JJ, Cho EK, et al. Segmental analysis of right ventricular longitudinal deformation in children before and after percutaneous closure of atrial septal defect. J Cardiovasc Ultrasound. 22(4): 182-8 (2014).
- Agha HM, Mohammed IS, Hassan HA, et al. Left and right ventricular speckle tracking study before and after percutaneous atrial septal defect closure in children. J Saudi Heart Assoc. 32(1): 71-8 (2020).
- Bussadori C, Oliveira P, Arcidiacono C, et al. Right and left ventricular strain and strain rate in young adults before and after percutaneous atrial septal defect closure. Echocardiography. 28(7): 730-7 (2011).
- Xu Q, Sun L, Zhou W, et al. Evaluation of right ventricular myocardial strains by speckle tracking echocardiography after percutaneous device closure of atrial septal defects in children. Echocardiography. 35(8): 1183-8 (2018).