Research Article - Interventional Cardiology (2021)
Right ventricle reverse remodelling following transcatheter and surgical secundum: Atrial septal defect closure in adults by cardiac magnetic resonance imaging
- Corresponding Author:
- Amr Mansour
Department of Cardiology,
Congenital and Structural Heart Disease Unit,
Ain Shams University Hospitals,
Cairo,
Egypt,
E-mail: amrmansour@med.asu.edu.eg
Received date: March 08, 2021 Accepted date: March 22, 2021 Published date: March 29, 2021
Abstract
Background: Securely closed Atrial Septal Defect (ASD) leads to reduction in right cardiac dimensions and improvement of symptoms. Device has become an accepted alternative to surgical closure. CMR is an accurate imaging modality for the assessment of cardiac function and volumes.
Objective: We aimed at studying electrical and mechanical remodeling in RV preclosure and 3 months after transcatheter and surgical closure.
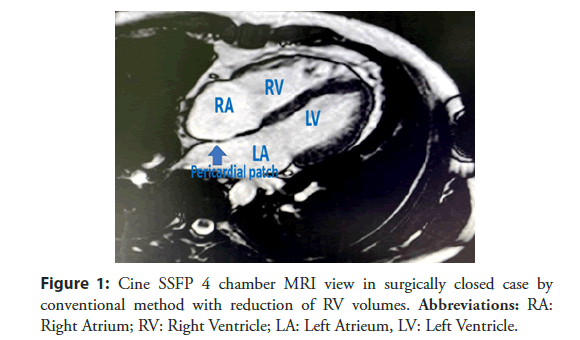
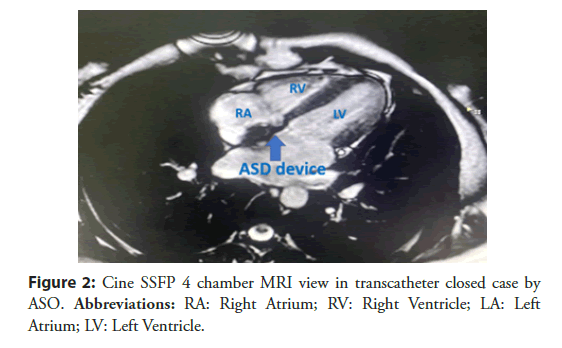
Results: Our prospective study included 30 consecutive adult patients with isolated secundum ASD referred to either transcatheter or surgical ASD closure. There was significant reduction in the QT dispersion among the same group as compared with the baseline values (QTc dispersion was 70.33 ± 24.04 to 60.26 ± 28.56 in device group vs. 80.73 ± 30.38 to 60.27 ± 28.57 in surgical group). There was no significant difference between two groups indicating that transcatheter and surgical closure had led to equivalent value of electrical remodelling (P-value >0.05). In CMR study we measured Right Ventricle End Diastolic Volume (RVEDV), Right Ventricle End Systolic Volume (RVESV), Right ventricle function and Right ventricle mass index. RVEDV and RVESV decreased significantly in both groups as compared to the baseline values (P-value <0.001). Transcatheter closure resulted in more significant reduction in the RVEDV and RVESV than the surgical closure (P-value=0.03 and 0.02 respectively), (Figures 1 and 2). In device closure; RV-function after closure was significantly higher in comparison to surgical closure (60.67 ± 5.12 vs. 52.73 ± 8.62 (%); P<0.001). The RV mass decreased significantly in each group as absolute value from the baseline (P-value (0.001) but it was statistically insignificant different between the two groups (P-value 0.31) while percentage of change was higher in device group (-) 20.38 ± 10.80 versus (-) 16.63 ± 14.91 in surgical group.
Conclusion: Our study showed significant changes from baseline measurements with significant RV mechanical reverse remodeling in the device group but there were no significant changes in electrical remodeling between the two groups.
Keywords
ASD closure; RV reverse remodelling; Cardiac CMR
Abbreviations
ASD: Atrial Septal Defect; ECG: Electrocardiogram; CMR: Cardiac Magnetic Resonance; Pd: P wave dispersion; RA: Right Atrium; RVEDV: Right Ventricle End Diastolic Volume; RVESV: Right Ventricle End Systolic Volume; PAH: Pulmonary Arterial Hypertension; PVR: Pulmonary Vascular Resistance; BSA: Body Surface Area, TEE: Transoesophageal Echocardiography; P-max: P wave maximum; P-min: P wave minimum; Pd: P wave dispersion, QTD: QT Dispersion; SSFP: Steady-State Precession; TTE: Transthoracic Echocardiography, ASO: Amplatzer Septal Occluder
Introduction
ASD is considered the most common congenital heart disease first diagnosed in adults [1]. The fact that most infants and children with ASD are asymptomatic and have unremarkable physical findings is one of the reasons for the delay in diagnosis [2]. Prolonged exposure causes chronic right heart volume overload, which leads to RV dilatation and, as a result, pulmonary hypertension and right heart failure due to increased pulmonary flow [3]. ASD closure leads to electrical and mechanical reverse remodelling after abolishment of the shunt [4]. There have been few comparisons, whether device or surgical closure is more effective in regression of right heart volumes [5]. Transcatheter ASD closure has proven to be a cost-effective alternative to secundum ASD closure, avoiding the complications of surgical closure in the form of cardiac trauma and wound complications [6]. Because of the RV’s fundamentally complex structural geometry, assessing RV function remains difficult [7]. CMR, with its multiplanar imaging capabilities, is used to accurately quantify shunts, RV ventricular volumes, and function [8] (Figure 1 and 2).
Aim
We aimed at studying electrical and mechanical changes in RV preclosure and 3 months after transcatheter and surgical closure.
Materials and Methods
This study was approved by our institutional and local review board, written informed consent was obtained from all of the patients enrolled in this study. 30 consecutive patients were included with isolated secundum ASD, 15 patients underwent successful transcatheter ASD device closure and 15 had surgical closure. All patients were subjected to 12 leads ECG and CMR before the ASD closure, and 3 months later. Patients included in the study were with Secundum ASD with RV volume overload. We excluded Patients with secundum ASD and associated coronary artery disease, patients with Pulmonary Vascular Resistance (PVR) >5 woods units and anomalous pulmonary venous return. A custommade sheet was made for all the patients [12], leads surface ECG as well as CMR assessment were obtained pre closure and 3 months after closure of the ASD.
Electrocardiographic study
ECG machine used was: Electrocardiograph ECG-2250-Nihon Kohden. A 12-leads ECG was recorded at a speed of 50 mm/s and amplitude of 1 mV/cm before and 3 months after ASD closure for evaluation of the following electrical parameters:
QT Dispersion (QTD): Defined as the difference between the longest (QTc max) and the shortest (QTc min) QTc intervals within a 12–leads ECG [9].
Echocardiography either transthoracic (TTE) or transoesophageal (TEE): TTE and TEE were used to assess ASD size, its rims and exclude anomalous pulmonary venous drainage [10].
Cardiac magnetic resonance assessment: All CMR studies were performed with subjects in the supine head first position. Using a 1.5 Tesla MRI scanner (Ingenia Philips) Scanning was performed with ECG gating during end-expiratory breath-holding phase.
Steady-State Precession (SSFP) ECG gated sequences were obtained retrospectively (Image matrix 256 × 150, field of view 380 mm, repetition time 52.05 ms, echo time 1.74 ms and flip angle 70°) [11].
MRI was used to shunt fraction (QP\QS)
For the ventricular image set, the stack of cine SSFP images were acquired in the short axis view from the level of the mitral valve to the left ventricular apex with 8 to 12 slice thickness, and measurements were indexed to the patient’s Body Surface Area (BSA) [12].
Analysis of the RV was performed on per slice basis by manual contouring of the endocardial and epicardial borders. Volumes were calculated based on the Simpson’s method [13]. We included the trabeculations and papillary muscles as part of the RV volume [14].
ASD closure: Percutaneous transcatheter ASD closure was performed when rims were adequate under general anaesthesia with fluoroscopic and TEE guidance. Heparin (100 IU/Kg) was given in every case. To avoid over sizing A 24-mm or 34-mm sizing balloon (AGA Medical Corp) was used to measure the diameter of the defect.
The procedure was done using Amplatzer Septal Occluder (ASO) device, its sizes were 24 ± 6.6 mm ranging from (11-38 mm). Surgical closure was done for patients with defects that were not suitable for transcatheter closure (with inadequate rims) by means of patch technique.
Results
Demographic and clinical data of the study groups
The mean age of patients underwent device closure was 33.73 ± 13.06 years while mean age of those underwent surgical closure was 35.33 ± 15.18 years with insignificant difference between both groups (P=0.75), (Table 1).
| Group 1 (Device closure) (n=15) | Group 2 (Surgical closure) (n=15) | P-value | |
|---|---|---|---|
| Age (years) | 33.73 ± 13.06 | 35.33 ± 15.18 | 0.75 |
| Sex | 0.65 | ||
| Female | 10 (66.7%) | 10 (66.7%) | |
| Male | 5 (33.3%) | 5 (33.3%) | |
| BMI (Kg/m2) | 24.78 ± 2.94 | 24.44 ± 4.02 | 0.79 |
| Heart rate (bpm) | 92 ± 10.14 | 93 ± 9.59 | 0.78 |
Data expressed as frequency (percentage), mean (SD). P-value was significant if <0.05.
Table 1: Demographic date of studied patients.
In both groups, majority (66.7%) of patients were females and less than 40 years old.
There were insignificant differences between both groups as regard HR, BMI.
Clinical criteria among study groups
Thirteen out of fifteen (86.7%) and Twelve out of Fifteen (80%) patients underwent device and surgical closure, respectively had baseline NYHA class II and the majority of patients in both groups had NYHA class I after closure.
All of the patients did not have diabetes or systemic hypertension.
Assessment of the electrical remodelling parameters
Both groups showed significant reduction in QT dispersion after ASD closure when compared to the baseline values with P-value<0.05, (Table 2). However, there was no difference between both groups, (Table 3).
| Group 1 (Device closure) | Group 2 (Surgical closure) | |||||
|---|---|---|---|---|---|---|
| Before | After | P-value | Before | After | P-value | |
| QTD (ms) | 70.33 ± 24.04 | 60.26 ± 28.56 | 0.003 | 80.73 ± 30.38 | 60.27 ± 28.57 | 0.001 |
QTD: QT Dispersion. Data expressed as frequency (percentage), mean (SD). P-value was significant if <0.05.
Table 2: ECG parameters before and after ASD closure in device and surgical group.
| Group 1 (Device closure) (n=15) | Group 2 (Surgical closure) (n=15) | P-value | |
|---|---|---|---|
| Heart rate (bpm) | |||
| Baseline | 92 ± 10.14 | 93 ± 9.59 | 0.78 |
| Post-closure | 78 ± 6.76 | 78.67 ± 11.87 | 0.85 |
| Percentage of change | (-) 14.68 ± 8.07 | (-) 15.40 ± 8.89 | 0.81 |
| QT dispersion (ms) | |||
| Baseline | 70.33 ± 24.04 | 80.73 ± 30.38 | 0.3 |
| Post-closure | 60.26 ± 28.56 | 60.27 ± 28.57 | 0.66 |
| Percentage of change | (-) 19.33 ± 11.28 | (-) 24.98 ± 10.16 | 0.42 |
QTD: QT Dispersion. Data expressed as frequency (percentage), mean (SD). P-value was significant if <0.05.
Table 3: ECG parameters comparing both groups.
Shunt fraction (QP/QS) by CMR
Shunt fraction assessed by CMR showed insignificant statistical difference between both groups, (Table 4).
| Device closure (n=15) | Surgical closure (n=15) | P-value | |
|---|---|---|---|
| QP/QS ratio | |||
| Before closure | 2.03 ± 0.25 | 2.23 ± 0.40 | 0.11 |
| After closure | 0.95 ± 0.13 | 1.04 ± 0.09 | 0.04 |
Data expressed as frequency (percentage), mean (SD). P-value was significant if <0.05. PAP: Pulmonary Artery Pressure, QP\QS: Shunt fraction.
Table 4: PAP and shunt fraction (QP/QS) in both groups.
Assessment of the mechanical remodelling by CMR
RV measurements: RVEDV and RVESV showed significant changes from the baseline measurements in both groups after ASD closure. Comparing between both groups showed significant difference between them with more reduction in the transcatheter arm with P-value <0.05, (Table 5). In device closure; RV-function after closure was significantly higher in comparison to surgical closure (P<0.001).
| Group 1 (Device closure) (n=15) | Group 2 (surgical closure) (n=15) | P-value | |
|---|---|---|---|
| RV-EDV (ml/mm2) | |||
| Before closure | 133.33 ± 25.26 | 152.33 ± 52.36 | 0.21 |
| After closure | 87.10 ± 14.08 | 106.60 ± 31.21 | 0.03 |
| Percentage of change | (-) 32.60 ± 13.55 | (-) 27.20 ± 15.07 | 0.31 |
| RV-ESV (ml) | |||
| Before closure | 51.63 ± 11.31 | 69.20 ± 33.81 | 0.06 |
| After closure | 35.52 ± 8.24 | 50.67 ± 23.90 | 0.02 |
| Percentage of change | (-) 29.33 ± 15.37 | (-) 21.86 ± 23.99 | 0.31 |
| RV function (%) | |||
| Before closure | 56.93 ± 4.38 | 56.33 ± 8.72 | 0.81 |
| After closure | 60.67 ± 5.12 | 52.73 ± 8.62 | <0.001 |
| Percentage of change | 6.64 ± 5.85 | (-) 6.22 ± 3.19 | <0.001 |
| RV mass (mm) | |||
| Before closure | 37.53 ± 5.02 | 39.35 ± 8.71 | 0.48 |
| After closure | 29.78 ± 5.46 | 32.29 ± 7.82 | 0.31 |
| Percentage of change | (-) 20.38 ± 10.80 | (-) 16.63 ± 14.91 | 0.43 |
Data expressed mean (SD). P-value was significant if <0.05. RV: Right Ventricle; EDV: End-Diastolic Volume; ESV: End-Systolic Volume.
Table 5: Parameters of RV in comparison among two groups.
The RV mass decreased significantly in each group as absolute value from the baseline (P-value 0.001) but it was statistically insignificant different between the two groups (P-value 0.31). Univariate and multivariate logistic regression analyses were performed to identify the potential clinical, ECG and CMR predictors of remodeling. Using univariate logistics regression, TR regurgitant fraction, RA SV, LA SV, LA maximal area and QP/ QS are the predictors of remodeling. While multivariate logistic regression showed that previous predictors were insignificant.
Discussion
We included a total number of 30 adult patients, age, sex and BSA matched patients in a prospective study to compare short term outcome of the RV electrical and mechanical remodelling parameters after transcatheter and surgical ASD closure.
The main purpose of ASD closure is the abortion of shunt with excess right heart volume. With our cohort, ASD surgical closure leading to both electrical remodeling of the same as percutaneous closure with better results for RV mechanical remodeling in device group.
CMR has been shown to be both reliable and reproducible in terms of quantitative RV assessment [15].
In our study there was significant shortening in the QTD after ASD closure as compared to the baseline measurements in both groups. However, there was no significant difference between the two groups.
This agree with Rücklová et al. [16] found significant reduction in the QT dispersion one month after the intervention either transcatheter or surgical closure.
We did not find superiorly of any method of closure on the ventricular electrical remodelling.
Transcatheter ASD closure had led to more reverse remodelling in the indexed RVEDV and RVESV measurements when compared to the surgical arm.
This agreed with Pascotto et al. [17] who reported failure of the surgical ASD closure to completely revert the right ventricular chamber overload, they explained this by either functional changes secondary to the effects of the cardio-pulmonary bypass technique or cardiac geometric alteration resulting from opening of the pericardial sac.
Our results disagree with the study performed by Foo et al. [5] who found no difference between the surgical and device closure groups. This can be explained by the difference of modalities used for analysis of the RV volumes. In our study we used the CMR which is considered as the gold standard for RV volumetric assessment, while Foo et al. used (2D) echocardiography which rely heavily on geometrical assumption [5].
Regarding RV function our study revealed statistically significant improvement in function in device group only, this in disagree with Berger et al. [18] who showed normalization of RVEF early after ASD closure, irrespective of whether this was achieved surgically or by transcatheter closure, which is the only study reported this, the reason for divergent results regarding RV performance after ASD closure is the limited accuracy of two dimensional echocardiography in quantifying RV parameters [19].
RV mass showed statistically significant reduction from baseline parameters. Karen et al. [20] reported reduction of RV mass 6 months post device closure. Schoen et al. [2] showed that regression of RV mass was evident within 12 months but not significantly compared with baseline MRI measurements at 6 months follow up, this due to in their study The moderator band and evident trabeculations were included in the mass and excluded from the RV volume but in our study we included trabeculations and papillary muscles as part of the RV volume will achieve higher reproducibility [21]. No study reported effect of surgery in RV mass post-surgical closure.
Using univariate and multivariate logistic regression analyses, Univariate analysis was in agree with Pascotto et al. [22] who reported a striking correlation between preprocedural cardiac overload and its reduction after shunt disappearance, regardless of the volume overload extent, and partially disagree with Thilén et al. [23] who documented that Sex, age, size of the defect, QP/ QS, RV area prior to closure did not significantly influence the potential to normalize RV area 1 year post-closure.
Conclusion
ASD closure can reverse electrical and mechanical changes in the ventricular myocardium and cause a subsequent reduction in the QT dispersion. As evidenced by CMR, both transcatheter and surgical ASD closure resulted in equivalent degrees of ventricular electrical remodeling and better ventricular mechanical remodeling. ASD percutaneous closure is beneficial not only because it is less costly and invasive than open-heart surgery, but it also improves RV function.
Limitations and Recommendations
A small sample size in our study was used due to financial constraints; patients in our developing countries were unable to pay the cost of CMR, which was performed twice (pre and post closure), and it was not covered by health insurance while I was conducting the study. We require multicenter experience rather than single-center experience.
Rather than studying a single age group, we intend to study several age groups in order to assess the effect of time course on remodeling.
References
- Silvestry FE, Cohen MS, Armsby LB, et al. Guidelines for the echocardiographic assessment of atrial septal defect and patent foramen ovale: From the American Society of Echocardiography and Society for Cardiac Angiography and Interventions. J Am Soc Echocardiogr. 28(8): 910-958 (2015).
- Schoen SP, Kittner T, Bohl S, et al. Transcatheter closure of atrial septal defects improves right ventricular volume, mass, function, pulmonary pressure, and functional class: A magnetic resonance imaging study. Heart. 92(6): 821-826 (2006).
- Graham T. Ventricular performance in congenital heart disease. Circulation. 84(6): 2259-2274 (1991).
- Butera G, Biondi-Zoccai G, Sangiorgi G, et al. Percutaneous versus surgical closure of secundum atrial septal defects: A systematic review and meta-analysis of currently available clinical evidence. EuroIntervention. 7(3): 377-85 (2011).
- Foo JS, Lazu M, Pang SY, et al. Comparative analysis of right heart chamber remodeling after surgical and device secundum atrial septal defect closure in adults. J Interv Cardiol. 31(5): 672-678 (2018).
- Berger F, Ewert P, Boöjrnstad PG, et al. Transcatheter closure as standard treatment for most interatrial defects: Experience in 200 patients treated with the Amplatzer™ Septal Occluder. Cardiol Young. 9(5): 468-473 (1999).
- Wang ZJ, Reddy GP, Gotway MB, et al. Cardiovascular shunts: MR imaging evaluation. Radiographics 23(S1): S181-S194 (2003).
- Petersen SE, Aung N, Sanghvi MM, et al. Reference ranges for cardiac structure and function using cardiovascular magnetic resonance (CMR) in Caucasians from the UK Biobank population cohort. J Cardiovasc Magn Reson. 19(1): 18 (2017).
- Guray U, Guray Y, Mecit B, et al. Maximum p wave duration and p wave dispersion in adult patients with secundum atrial septal defect: The impact of surgical repair. Ann Noninvasive Electrocardiol. 9(2): 136-141 (2004).
- Parasuraman S, Walker S, Loudon BL, et al. Assessment of pulmonary artery pressure by echocardiography-a comprehensive review. Int J Cardiol Heart Vasc. 12: 45-51 (2016).
- Rominger MB, Bachmann GF, Pabst W, et al. Right ventricular volumes and ejection fraction with fast cine MR imaging in breath–hold technique: Applicability, normal values from 52 volunteers, and evaluation of 325 adult cardiac patients. J Magn Reson Imaging. 10(6): 908-918 (1999).
- Alfakih K, Plein S, Thiele H, et al. Normal human left and right ventricular dimensions for MRI as assessed by turbo gradient echo and steady–state free precession imaging sequences. J Magn Reson Imaging. 17(3): 323-329 (2003).
- Reiter G, Reiter U, Rienmüller R, et al. On the value of geometry-based models for left ventricular volumetry in magnetic resonance imaging and electron beam tomography: A Bland–Altman analysis. Eur J Radiol. 52(2): 110-118 (2004).
- Hudsmith LE, Petersen SE, Francis JM, et al. Normal human left and right ventricular and left atrial dimensions using steady state free precession magnetic resonance imaging. Journal of cardiovascular magnetic resonance. 7(5): 775-782 (2005).
- Moon JC, Lorenz CH, Francis JM, et al. Breath-hold FLASH and FISP cardiovascular MR imaging: Left ventricular volume differences and reproducibility. Radiology. 223(3): 789-797 (2002).
- Rücklová K, Koubský K, Tomek V, et al. Prolonged repolarization in atrial septal defect: An example of mechanoelectrical feedback due to right ventricular volume overload. Heart Rhythm. 13(6): 1303-1308 (2016).
- Pascotto M, Santoro G, Cerrato F, et al. Time-course of cardiac remodeling following transcatheter closure of atrial septal defect. Int J Cardiol. 112(3): 348-352 (2006).
- Berger F, Jin Z, Ishihashi K, et al. Comparison of acute effects on right ventricular haemodymanics of surgical versus interventional closure of atrial septal defects. Cardiol Young 9(5): 484-487 (1999).
- Papavassiliou DP, Parks WJ, Hopkins KL, et al. Three-dimensional echocardiographic measurement of right ventricular volume in children with congenital heart disease validated by magnetic resonance imaging. J Am Soc Echocardiogr. 11(8): 770-777 (1998).
- Teo KS, Dundon BK, Molaee P, et al. Percutaneous closure of atrial septal defects leads to normalisation of atrial and ventricular volumes. J Cardiovasc Magn Reson. 10(1): 1-8 (2008).
- Schulz-Menger J, Bluemke DA, Bremerich J, et al. Standardized image interpretation and post-processing in cardiovascular magnetic resonance-2020 update. J Cardiovasc Magn Reson. 22(1): 1-22 (2020).
- Wu ET, Akagi T, Taniguchi M, et al. Differences in right and left ventricular remodeling after transcatheter closure of atrial septal defect among adults. Catheter Cardiovasc Interv. 69(6): 866-871 (2007).
- Thilén U, Persson S. Closure of atrial septal defect in the adult. Cardiac remodeling is an early event. Int J Cardiol. 108(3): 370-375 (2006).
Journal Metrics:
| Impact Factor | 1.34 |
| Scimago Journal Rank (SJR) | 123 |
| SJR Total Cites | 15 |
| Source Normalized Impact per Paper (SNIP) | 0.144 |
| h-index (2023) | 12 |
| PubMed NLM ID: | 10148499 |
| Google Scholar h5 index: | 6 |
| Iindex Copernicus Value: | 105.52 |
Google Scholar citation report
Citations : 1400
Interventional Cardiology received 1400 citations as per Google Scholar report