Review Article - Interventional Cardiology (2012) Volume 4, Issue 6
Possibility of contact force monitoring during catheter ablation of ventricular tachycardia
- Corresponding Author:
- Paolo Della Bella
Arrhythmia Department & Clinical Electrophysiology Laboratories
Ospedale San Raffaele, IRCCS, Milan, Italy
E-mail: dellabella.paolo@hsr.it
Abstract
Keywords
arrhythmic substrate,catheter ablation,contact force,electroanatomical mapping,late potential,ventricular tachycardia
Introduction
Catheter ablation is considered to be a firstline therapy for various tachyarrhythmias, including ventricular tachycardia (VT). Nowadays, its indication has been widely extended to more complicated arrhythmias by the use of electroanatomical mapping systems, which reconstruct integrated anatomical and electrophysiological information as threedimensional images. The precise characterization of the arrhythmia substrate leads to the identification of a suitable ablation target even for unstable VTs.
The contact between the tip electrode of the ablation catheter and the myocardial tissue is one of the most important factors that affect both the accuracy of maps and the efficacy of energy delivery.
In an electroanatomical map, the geometry is created by tracing of the catheter along the wall of the chamber. During the mapping procedure, on one hand, an insufficient contact force (CF) between the catheter tip and the myocardial tissue leads to internal points acquisition, but on the other hand, an excessive CF can lead to distortion of the chamber, creating, in both cases, a discrepancy between acquired data and actual anatomy. One can also easily imagine that the radiofrequency (RF) delivery with insufficient contact results in an incomplete ablation lesion.
Thus, the importance of the concept of applying appropriate CF in the mapping and ablation procedure has been widely recognized. Nevertheless, the authors had previously had only surrogate contact indicators, such as the movement of the tip of catheter in fluoroscopy, ST segment elevation in unipolar electrogram, and the change of impedance during RF application. Recently several new technologies, providing direct information of contact status including direction, value of CF and its chronological change have been developed to reduce the recurrence rate by improving the CF between the catheter tip and the myocardial tissue. In this review, principles, utilities, limitations and future directions of CF monitoring during mapping and ablation procedures of VT are discussed.
Contact force mapping technologies
According to the specific technologies provided by different companies, contact between the tip and the tissue is evaluated in different ways. Currently, three technologies for CF monitoring are available, based on deformation of spring, the change of optical parameters, or change of impedance.
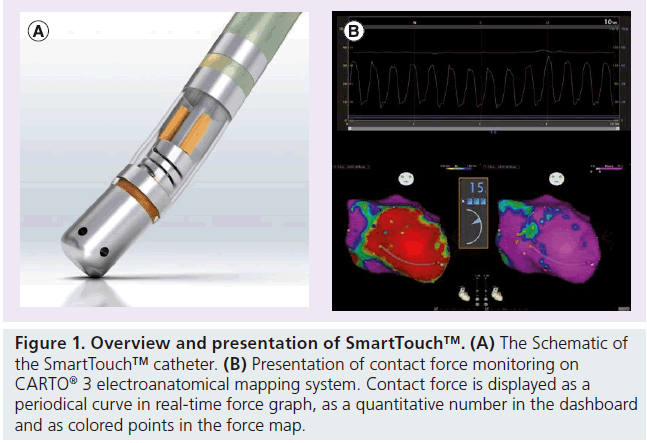
▪ SmartTouch™
SmartTouch™ (Biosense Webster, CA, USA) (Figure 1), is a CF monitoring technology integrated into the Thermocool® SmartTouch™ irrigated tip catheter and CARTO® 3 electroanatomical mapping system. A tiny spring is mounted in the distal tip of this catheter, to connect the distal tip dome to the proximal second ring electrode. The degree of spring compression and/or stretching is detected every 50 ms by the three receiving sensors located at the base of the spring. CF values are visualized in different ways on the CARTO 3 system, as a real time value, direction and real time force graph. The quantitative CF is visualized on the CARTO 3 screen as an average or maximum value within a given time window; the direction of the force is displayed as a color-coded arrow vector on the tip of the catheter image; a real-time force graph is displayed in an independent window to visualize the chronological changes during the cardiac cycle. The distribution of CF can also be constructed on a CF map.
Figure 1: Overview and presentation of SmartTouch™. (A) The Schematic of the SmartTouch™ catheter. (B) Presentation of contact force monitoring on CARTO® 3 electroanatomical mapping system. Contact force is displayed as a periodical curve in real-time force graph, as a quantitative number in the dashboard and as colored points in the force map.
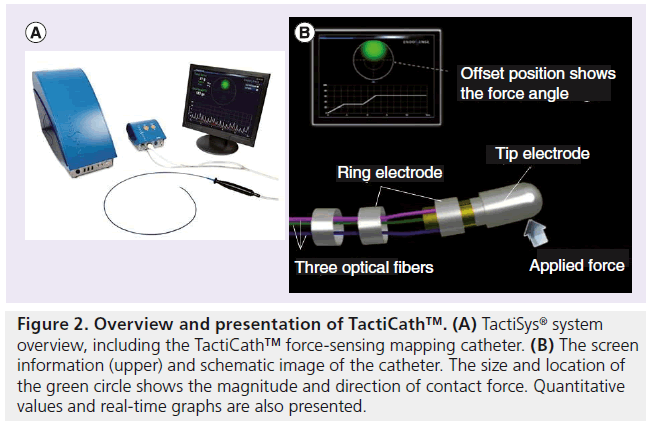
▪ TactiCath™
TactiCath™ (Endosense SA® , Geneva, Switzerland) (Figure 2) is a technology to evaluate the CF by detecting the change in the specific wavelength of light reflected in the fiber Bragg grating (FBG) [1–3]. An optical sensor with three optical fibers is mounted near the distal part of the RF catheter, between the second and third electrodes.
Figure 2: Overview and presentation of TactiCath™. (A) TactiSys® system overview, including the TactiCath™ force-sensing mapping catheter. (B) The screen information (upper) and schematic image of the catheter. The size and location of the green circle shows the magnitude and direction of contact force. Quantitative values and real-time graphs are also presented.
FBG is one type of in-fiber grating sensor which is made of the optical fiber inscribed with periodic perturbations. As broadband light is introduced into the fiber, a specific wavelength (i.e., Bragg wavelength), corresponding to the period of the gratings, is reflected back towards the source. In this system, instead of broadband light, infrared laser light (with a wavelength of 1520–1570 nm) is emitted through the proximal end of the optical fiber in the RF catheter, and only the light with the specific wavelength is reflected by the FBG on the deformable body at the distal end of each fiber.
When CF is applied to the tip, it deforms the sensor body, and compression or stretch of the three fibers changes the periodical cycle of the R refractive index pattern. This change of cycle shifts the wavelength of the reflected light proportionally to the applied force. This system can present direction and magnitude of the force at every 100 ms, with a sensitivity of 1 g. The total value and magnitude of axial and lateral component vectors of CF are visualized, as well as the direction or chronological trend.
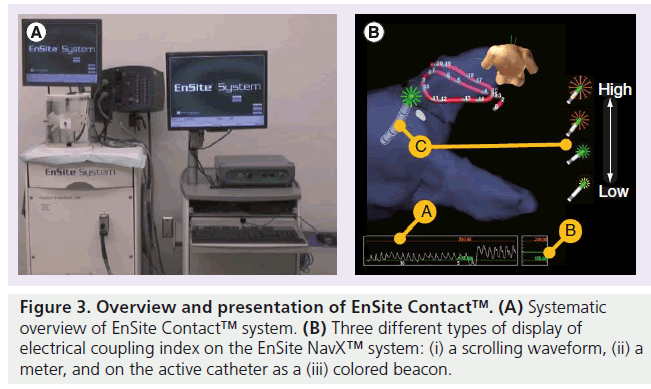
▪ EnSite Contact™
EnSite Contact™ (St Jude Medical Inc., MN, USA) (Figure 3) presents the contact and other information derived from impedance between the tip of the catheter and the myocardial tissue. RF energy applied to the human body forms an alternative current circuit. In this model, besides the resistance in a direct current circuit, the reactance yielded by the capacitor-like behavior of the cell (a charge gradient created by a lipid bilayer) also acts to impede current flow. Impedance is represented as a complex number derived from resistance and reactance.
To measure the impedance, this system applies subthreshold (100 μA at 20 kHz) alternative current between the tip of the catheter and two independent patches on the body surface. The equivalent circuit for this configuration is modeled as three networks, each of which contains a resistance and a capacitor (RCcommon, RCA, RCB). If the two patches are placed physically close to each other, the RCcommon network represents not only the local impedance at the catheter tip-to-tissue interface, but also includes thoracic impedances between the heart and the body surface. On the other hand, as the patches are moved further apart from each other, RCcommon increasingly represents only the catheter tip-to-tissue impedance. Local resistance and reactance derived from the value of the local impedance at RCcommon are again integrated mathematically (after appropriate weighing, derived from the bench and animal experimental studies) into a single measure termed the electrical coupling index. The electrical coupling index is displayed on the EnSite NavX™ system in three ways: as a scrolling waveform; as a meter; and on the active catheter as a colored beacon.
Importance of contact between the tip of catheter & myocardial tissue
Previous studies using a nonirrigated ablation catheter [4,5] have shown that CF is a predictor of successful lesion creation and complications such as cardiac tamponade or steam pop during radiofrequency application. Since tip temperature feedback is practically meaningless to control lesion formation by using irrigation catheters [6], the process of CF monitoring might be increasingly highlighted.
Thus, the importance of the concept of appropriate CF in mapping and ablation procedures had been widely recognized from the early stage of catheter ablation. Nevertheless, the authors had only had surrogate indicators. In the absence of a direct quantitative indicator of the CF, many attempts to identify surrogate parameters of ‘good contact’ have been made, including direct visualization of the tip of the catheter by fluoroscopy or echocardiography, or indirect quantitative parameters such as ST segment elevation in unipolar electrogram, change of temperature and impedance during ablation [5,7]. Fluoroscopy has been used as one of the most common techniques to monitor and visualize the contact between the catheter tip and the myocardial tissue. It provides a visualization of real-time catheter positions and movements from many angles around the patient; however, little quantitative information is available about the level of catheter–endocardial contact, and it increases the risk of radiation exposure for both patient and physician [8,9].
Intracardiac and transesophageal echocardiography is one solution to reduce the limitations of fluoroscopy [8,10–13]. Kalman et al. reported that good perpendicular contact between catheter tip and tissue, validated by intracardiac echocardiography, is associated with the efficacy of tissue heating and lesion size, which is often overestimated by fluoroscopic visualization [12,14].
As an indirect surrogate parameter of contact, electrical impedance between the tip of the catheter and the dispersive electrode was investigated by Cao et al. Since resistivity differs between blood and endocardium, the impedance increases as the catheter tip lodges into the tissue. They reported good accuracy for prediction of the depth by spline curve interpolation using the preobtained calibration curve [15]. Zheng et al. and Stickberger et al. also suggest that greater CF is related to higher preablation impedance [16,17].
Thermal coagulation of myocardium leads to significant changes in its optical properties in the near infrared spectral region. To test the hypothesis that the changes in the optical properties of the RF-ablated cardiac tissue can be used to provide in vivo monitoring of lesion-formation parameters, Demos and Sharareh meanwhile assessed various parameters of the RF ablation operation via optical spectroscopy [18]. The near-infrared light was transmitted through a fiber at the tip of the catheter, and another fiber received the reflected light. The difference between the spectral characteristics of the transmitted and received light provided information such as contact level, lesion quality and char formation.
However, as the relationship between these surrogate indicators and actual CF had not been fully elucidated, there were no data on the adequate CF to be used in clinical settings until the improvement in the real-time force-sensing technology.
At first, the utility of the direct force sensing was evaluated by animal experimental studies. Yokoyama et al. [3] and Thiagalingam et al. [19] evaluated the effect of CF on ablated lesion size using canine thigh muscle and swine excised heart with the ex vivo preparation, respectively. They both showed that the depth, diameter and volume of the ablated lesion becomes greater according to increased applied CF in each subgroup of different power control strategy.
Okumura et al. performed in vivo analyses investigating the relationship between CF and contact status validated by intracardiac echocardiography, image distortion during mapping procedures, and individual lesion formation during irrigated-tipped ablation of canine atria [20]. Minimal contact, consistent contact and tissue tenting by intracardiac echocardiography was correlated with forces of 4.7 ± 5.8 g, 9.9 ± 8.6 g, and 25.0 ± 14.0 g, respectively. A robotics-aided electroanatomical map obtained with CF more than 10 g was 1.5- times greater than that with minimum contact. In ablation procedure, full-thickness, larger volume ablative lesions were optimized by application of 10–20 g of CF. The researchers suggested that the results of mapping and ablation procedures are dependent on the force applied to the tissue. While mapping requires lower-force application to avoid image distortions, ablative lesion size is optimized by the application of higher CF.
Clinical studies for assessing safety & efficacy of contact force
The procedure-related and device-related safety and possible implications on patient safety of this CF-sensing system were evaluated for the first time in the TOCCATA study [21]. In this multicenter observational study, 77 patients (43 with right-sided supra-VT [SVT group] and 34 with atrial fibrillation [AF; LA group]) received percutaneous catheter ablation with the use of the TactiCath CF catheter. The safety profile of the CF was comparable to that of conventional irrigated RF catheters. The incidence of deviceor procedure-related serious adverse events was 2% among study patients with rightsided SVT and 12% with AF patients, which were both below the prespecified safety rate of 11.4 and 16.8%, respectively. This study also showed there were significant differences in forces applied during CF mapping among the investigators. High transient CF events occurred in 27 (79%) patients, and one cardiac tamponade during manipulation occurred in one patient of the LA group, which highlights the importance of continuous monitoring of CF during not only ablation, but also mapping procedures. Furthermore, they presented the results of post hoc retrospective study, which showed a statistically significant relationship between the CF applied at ablation sites and the 12‑month success of the procedure (median CF applied: 20 g in the nonrecurrent group vs 11 g in the recurrent patient group, p < 0.05).
New ongoing clinical studies aim to evaluate the utility of CF monitoring.
EFFICAS is a series of single-arm, multicenter, prospective studies launched in May 2010 to assess the clinical effectiveness of catheter ablation with and without TactiCath CF monitoring. In the EFFICAS I pilot study, 17 patients with AF underwent pulmonary vein isolation by operators blinded to CF which was recorded for later study. The relationship between CF and gap recurrence was evaluated at second interventional procedure 3 month after index procedure. At a 3-month assessment, 17 gaps recurred in seven patients. Particularly in posterior walls, CF and force-time integral was lower in segments with gaps (CF 17.9 ± 8.1 g and force time integral 2103 ± 1479 gram seconds [gs]) compared with segments with no gap (CF 24.4 ± 14 g and force time integral 2989 ± 2328 gs). According to outcome data from pilot studies including EFFICAS I, larger EFFICAS studies will be designed with appropriate clinical end points.
TOCCASTAR is a prospective, randomized, multicenter, investigational device exemption clinical trial to assess the safety and effectiveness of a TactiCath CF sensing catheter used for ablation in patients with symptomatic paroxysmal AF [101]. This study has been conducted at up to 30 centers in the USA and Europe. The total number of patients is estimated to be 400. Enrollment started in January 2011 and was completed in July 2012. Subjects were randomized on a one-to-one basis for treatment with either the TactiCath force-sensing catheter or another irrigated-tip ablation catheter with no CF-sensing capability. The primary effectiveness end point measures were acute procedural success (successful electrical isolation of all pulmonary veins) and chronic freedom of symptomatic AF, atrial tachycardia and atrial flutter at 12 months. The safety end points will report incidence of device-related early-onset primary serious adverse events, as well as serious adverse events occurring within 7 days of the index procedure or hospital discharge, whichever is later, and diagnosed at any time during the follow-up period. Additional measures including quality of life or the contribution of real-time CF information to procedural effectiveness during ablation compared with conventional RF irrigated catheters will also be studied.
Another clinical study, SMART-AF, was designed to demonstrate the safety and effectiveness of the Thermocool SmartTouch catheter during standard electrophysiology mapping and RF procedures of symptomatic, drug-refractory, paroxysmal AF [102]. The primary effectiveness outcome for this study was freedom from documented symptomatic AF, atrial tachycardia, or atrial flutter episodes through 12‑month follow-up (includes a 3-month blanking period), and the primary safety end point was defined as the incidence of early onset (within 7 days of the AF ablation procedure) primary adverse events. After the launch in June 2011, it enrolled 173 patients at leading centers across the USA and in January 2012, Biosense Webster Inc. announced the completion of enrollment in this clinical trial.
Likewise, St Jude Medical Inc. also launched a prospective, multicenter and nonrandomized clinical study called CONTACT-AFL in October 2011 [103]. It enrolls 150 patients with cavo-tricuspid isthmus-dependent typical atrial flutter and measures the incidence of composite, serious adverse events within 7 days postprocedure as a primary safety end point, and achievement of bidirectional block in the cavotricuspid isthmus and noninducibility of typical atrial flutter at least 30 min following the last RF ablation with the investigational system as primary efficacy or acute success end point. This study also assesses chronic success defined as freedom from recurrence of typical atrial flutter at 3 months after ablation.
Contact force monitoring in ventricular tachycardia mapping & ablation
As described above, current interest in assessment of safety and effectiveness of CF monitoring is mainly focused on SVT including atrial flutter or fibrillation. We can easily imagine that the importance of CF sensing should also be emphasized in mapping and ablation procedures of VT, however, little data is available on the effects of CF on electrophysiological parameters, such as signal amplitude or local impedance during mapping and ablation of ventricular chamber.
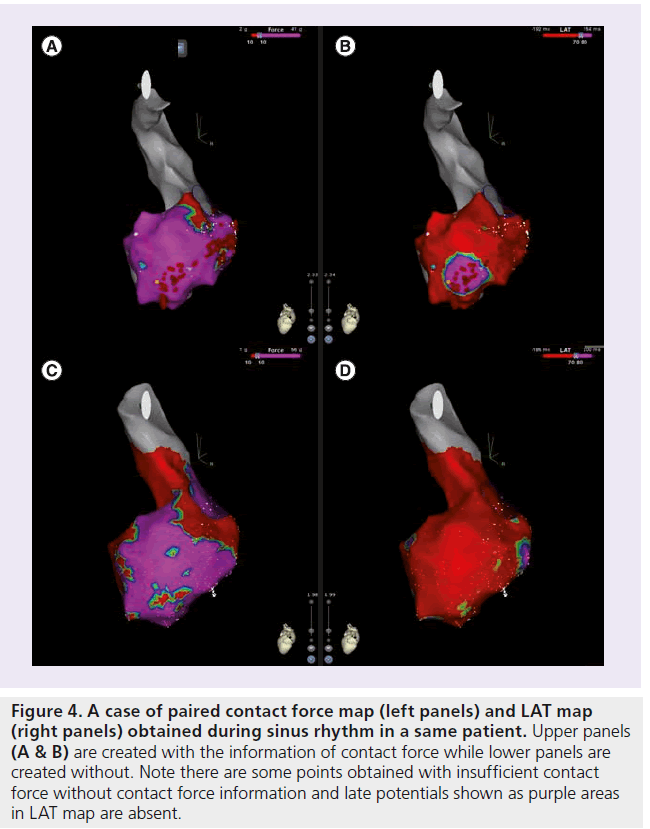
To assess the relationship between CF and electrophysiolosical parameters and to evaluate the importance of CF monitoring during mapping procedures of VT, CF was measured using SmartTouch in 27 chambers (six endocardial maps of right ventricle, 13 endocardial maps of left ventricle and eight epicardial maps) of 17 patients. All 8892 points sampled were thoroughly reviewed, and 5926 points with stable recording across at least 2 s were taken into further analysis. These points were divided into two groups according to presence or absence of consistent positive CF during thorough cardiac cycle: good contact and poor contact group. The frequency of points in the poor contact group reached up to 26%, despite of all of the efforts made by the operators to obtain constant contact based on classical parameters. There was no linear correlation between CF and electrophysiological parameters, such as bipolar and unipolar signal amplitude or local impedance. However, points with late potential were seen more frequently in the good contact group, which was consistent across the characteristics of the myocardial tissue (normal, low voltage area and scar). For the adverse characteristics of the VT like poor hemodynamic tolerance, the variable response to ventricular stimulation or to the entrainment maneuvers that can induce change in VT morphologies, the substrate mapping and ablation has become an important and sometimes unavoidable strategy to reach a good result. In this setting, late potentials registered in sinus rhythm are good markers for the characterization of the critical part of the re-entry circuits. Our data underline the importance of detecting these important signals to avoid the risk of underestimating pathological substrates of VT (Figure 4).
Figure 4: A case of paired contact force map (left panels) and LAT map (right panels) obtained during sinus rhythm in a same patient. Upper panels (A & B) are created with the information of contact force while lower panels are created without. Note there are some points obtained with insufficient contact force without contact force information and late potentials shown as purple areas in LAT map are absent.
During the VT ablation procedure, the use of irrigation-tip catheter is indispensable, since it allows delivery of more power to the tissue to create deeper lesions in thick ventricular myocardium. However, during irrigation, temperature monitoring is meaningless to evaluate the extent of contact between the tip of the catheter and the myocardial tissue. Previous studies have shown that the CF is related not only to lesion size, but also to incidence of complication, such as steam pop and coagulation. Recently, Nakagawa et al. clarified the relationship between CF and lesion size or steam pop in canine models. The SmartTouch irrigation-tip catheter was positioned in right ventricle and left ventricle under fluoroscopic and CARTO guidance. RF energy was delivered with different CF (low CF with median 7 g, moderate with 22 g and high with 48 g) to each three different sites in the right and left ventricle. According to increasing CF, lesion size increased significantly. Steam pop occurred with high CF in the right ventricle and moderate or high CF in the left ventricle [22]. Another study by Perna et al. shows that the level of CF to cause perforation during RF application is lower than that during mapping procedure [23], which highlights the increased importance of CF sensing in ablation procedures.
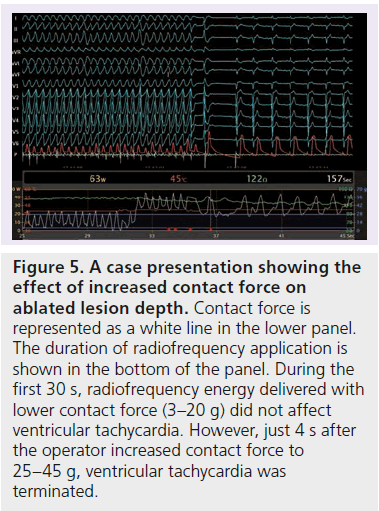
A case is presented in Figure 5 showing the efficacy of CF during RF application on lesion depth. The patient was a 22-year-old male with myocarditis-related VT. We could not obtain epicardial access because of severe adhesion; thus, the authors delivered RF energy only at the endocardial point with diastolic activity during VT. During the first 30 s of energy delivery with a mean CF of 15 g, the RF application did not affect VT. However, as soon as the operator increased the mean CF to 40 g, VT was interrupted and remained no longer inducible.
Figure 5: A case presentation showing the effect of increased contact force on ablated lesion depth. Contact force is represented as a white line in the lower panel. The duration of radiofrequency application is shown in the bottom of the panel. During the first 30 s, radiofrequency energy delivered with lower contact force (3–20 g) did not affect ventricular tachycardia. However, just 4 s after the operator increased contact force to 25–45 g, ventricular tachycardia was terminated.
Limitations of the contact force sensing
Although CF provides important information that supports efforts to achieve successful mapping and ablation procedures, there are at present no proven data showing its utility in increasing the precision of mapping or reducing complication. Some clinical trials are ongoing to measure noninferiority with existing, non-CF ablation. Furthermore, we have to note the limitations of CF monitoring. First, CF itself changes periodically during the cardiac and respiratory cycles, and the value is affected by contact status [24]. Second, the value of CF is presented in different ways, like mean or peak values of certain preceding times, or force– time integral. Furthermore, as Okumura has suggested previously, the optimal CF value may vary between mapping and ablation procedure [20]. Thus, there are many parameters presenting contact; however, it is not fully elucidated which one actually reflects the contact status best and how much the value should be. Previous study has shown that the ablation lesion size was correlated linearly to force–time integral, not to peak CF value [25]. In an observational study, we found that the mean CF value (during 500 ms preceding point annotation) is well correlated to contact status obtained from real-time graphs during thorough cardiac cycle, and a mean value more than 7 g predicts positive CF during the diastolic phase with good sensitivity and specificity (86 and 88%, respectively). However, these cutoff values may be affected by many factors, including chambers, tissue characteristics and setting of presentation.
As for safety issue, things are more complicated. Several studies refer to the relationship between CF and complications such as steam pop and perforation [2,3,19,20,23]. Although we can easily imagine that an excessively high CF plays an important part, actually many factors, including tissue characteristics, angle between the tip of the catheter and tissue, and amount of blood flow are involved in such complications. Furthermore, cardiac cycle CF sometimes increases too steeply to predict perforation. Thus, at present, it is important to remember that there is no threshold for CF, which assures complete safety. Further studies are required to establish the ‘optimal’ value of CF in each different situation.
Future perspective
Today, safety of catheter ablation is already established, with a quite low incidence of complications, except for one, remaining substantial risk: radiation exposure. This is especially true in mapping and ablation procedure of complex arrhythmia, which require f luoroscopy-guided catheter manipulation for long time periods, in which the amount of exposure has been becoming too large for patients and for medical professionals to ignore. The American College of Cardiology attaches importance to reducing radiation exposure and to promoting the as low as reasonably achievable principle (keep fluoroscopic exposure to a level as low as reasonably achievable). On the other hand, recent medical imaging technologies, including electroanatomical mapping and intracardiac ultrasound, have been improved towards lesser use of x-ray. Recently, Kerst et al. reported their results of ‘zero-fluoroscopy ablation’, attempted in 30 patients (20 cases of right atrium ablation, two of right ventricle and eight of left atrium) [26]. Mapping and ablation was performed by EnSite Contact CF sensing system with combined use of the NavX electroanatomical mapping system and transesophageal echocardiography for leftsided arrhythmias. Procedural time was generally comparable with conventional mapping and ablation, and procedural success rate was 97% (29 out of 30 patients: one unsuccessful case due to an epicardial accessory pathway within a coronary sinus aneurysm). In this study, CF monitoring made a great contribution to assure physical contact and to determine the safety range (mean CF was kept below 50 g during mapping and below 40 g during ablation).
To achieve an ultimate goal of nonfluoroscopic catheter intervention, the disadvantages of abolishing x-ray should be compensated for by other modalities. CF sensing provides us with precise information regarding contact status and will play a great role in the progression toward nonradiation ablation.
Conclusion
CF monitoring is a recently-emerging technology. Although its usefulness has not been proven in clinical studies, especially in cases with VT, it actually provides additional information that operators had never previously had. With understanding of the principles, advantages and limits, it could be a promising tool to improve the results of the mapping and ablation procedure of VT.
Financial & competing interests disclosure
P Della Bella is consultant for St Jude Medical and has received honoraria for lectures form Biosence Webster, St Jude Medical and Biotronik. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Executive summary
Contact force mapping technologies
▪▪ At present, three specific technologies are provided by different companies.
▪▪ Contact force (CF) is evaluated by deformation of the spring (SmartTouch™), shift in the wavelength of the reflected light (TactiCath™),
and change of impedance (EnSite Contact™).
Importance of contact between the tip of catheter & myocardial tissue
▪▪ CF is a predictor of successful lesion creation and complication.
▪▪ Operators have been forced to confirm good contact by surrogate parameters before a direct indicator of contact force is available.
▪▪ Animal experimental models have shown the relationship between quantitative CF and image distortion or size of ablation lesion.
Clinical studies for assessing safety & efficacy of contact force
▪▪ Some clinical studies are complete (TOCCATA, EFFICAS 1) or ongoing (TOCCASTAR, SMART-AF, CONTACT-AFL) to evaluate the safety
and efficacy of the CF monitoring technology, mainly in patients with supravantricular tachycardia or atrial fibrillation.
Contact force monitoring in VT mapping & ablation
▪▪ Our data showed 26% of the ventricular points sampled during sinus rhythm were taken with insufficient contact force, which was
associated with low detection of late potential.
Limitations of the contact force sensing
▪▪ At present there are no proven data showing improved efficacy and safety of contact force monitoring, compared with conventional
mapping and ablation.
▪▪ It is still unclear which parameters of CF provide the best efficacy and safety, or how much the value should be.
References
Papers of special note have been highlighted as:
▪ of interest
▪▪ of considerable interest
- Ho SC, Razavi M, Nazeri A, Song G. FBG sensor for contact level monitoring and prediction of perforation in cardiac ablation. Sensors (Basel) 12(1), 1002–1013 (2012).
- Shah D, Lambert H, Langenkamp A et al. Catheter tip force required for mechanical perforation of porcine cardiac chambers.Europace 13(2), 277–283 (2011).
- Yokoyama K, Nakagawa H, Shah DC et al. Novel contact force sensor incorporated in irrigated radiofrequency ablation catheter predicts lesion size and incidence of steam pop and thrombus. Circ. Arrhythm. Electrophysiol. 1(5), 354–362 (2008).
- Wittkampf FH, Nakagawa H. RF catheter ablation: lessons on lesions. Pacing Clin. Electrophysiol. 29(11), 1285–1297 (2006).
- Avitall B, Mughal K, Hare J, Helms R, Krum D. The effects of electrode-tissue contact on radiofrequency lesion generation. Pacing Clin. Electrophysiol. 20(12 Pt 1), 2899–2910(1997).
- Thiagalingam A, D’avila A, Mcpherson C, Malchano Z, Ruskin J, Reddy VY. Impedance and temperature monitoring improve the safety of closed-loop irrigated-tip radiofrequency ablation. J. Cardiovasc. Electrophysiol. 18(3), 318–325 (2007).
- Everett THT, Byrd I, Wilson E, Skoglund J, Olgin J. Phase angle shift is a better determinant for catheter electrode contact with tissue compared with a catheter sensed electrogram. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2008, 1733–1736 (2008).
- Stellbrink C, Siebels J, Hebe J et al. Potential of intracardiac ultrasonography as an adjunct for mapping and ablation. Am. Heart J. 127(4 Pt 2), 1095–1101 (1994).
- Calkins H, Niklason L, Sousa J, El-Atassi R, Langberg J, Morady F. Radiation exposure during radiofrequency catheter ablation of accessory atrioventricular connections. Circulation 84(6), 2376–2382 (1991).
- Saxon LA, Stevenson WG, Fonarow GC et al. Transesophageal echocardiography during radiofrequency catheter ablation of ventricular tachycardia. Am. J. Cardiol. 72(9), 658–661 (1993).
- Chu E, Fitzpatrick AP, Chin MC, Sudhir K, Yock PG, Lesh MD. Radiofrequency catheter ablation guided by intracardiac echocardiography. Circulation 89(3), 1301–1305 (1994).
- Kalman JM, Fitzpatrick AP, Olgin JE et al. Biophysical characteristics of radiofrequency lesion formation in vivo: dynamics of catheter tip-tissue contact evaluated by intracardiac echocardiography. Am. Heart J. 133(1), 8–18 (1997).
- Kalman JM, Olgin JE, Karch MR, Lesh MD. Use of intracardiac echocardiography in interventional electrophysiology. Pacing Clin. Electrophysiol. 20(9 Pt 1), 2248–2262 (1997).
- Stec S, Zaborska B, Sikora-Frac M, Krynski T, Kulakowski P. First experience with microprobe transoesophageal echocardiography in non-sedated adults undergoing atrial fibrillation ablation: feasibility study and comparison with intracardiac echocardiography. Europace 13(1), 51–56 (2011).
- Cao H, Tungjitkusolmun S, Choy YB, Tsai JZ, Vorperian VR, Webster JG. Using electrical impedance to predict catheter-endocardial contact during RF cardiac ablation. IEEE Trans. Biomed. Eng. 49(3), 247–253 (2002).
- Zheng X, Walcott GP, Hall JA et al. Electrode impedance: an indicator of electrode-tissue contact and lesion dimensions during linear ablation. J. Interv. Card. Electrophysiol. 4(4), 645–654 (2000).
- Strickberger SA, Vorperian VR, Man KC et al. Relation between impedance and endocardial contact during radiofrequency catheter ablation. Am. Heart J. 128(2), 226–229 (1994).
- Demos SG, Sharareh S. Real time assessment of RF cardiac tissue ablation with optical spectroscopy. Opt. Express 16(19), 15286–15296 (2008).
- Thiagalingam A, D’avila A, Foley L et al. Importance of catheter contact force during irrigated radiofrequency ablation: evaluation in a porcine ex vivo model using a force-sensing catheter. J. Cardiovasc. Electrophysiol.21(7), 806–811 (2010).
- Okumura Y, Johnson SB, Bunch TJ, Henz BB, O’Brien CJ, Packer DL. A systematical analysis of in vivo contact forces on virtual catheter tip/tissue surface contact during cardiac mapping and intervention.J. Cardiovasc. Electrophysiol. 19(6), 632–640 (2008).
- Kuck KH, Reddy VY, Schmidt B et al. A novel radiofrequency ablation catheter using contact force sensing: Toccata study. Heart Rhythm. 9(1), 18–23 (2012).
- Nakagawa H, Ikeda A, Govari A et al. Contact force sensor in a sarine irrigated radiofrequency ablation catheter predicts lesion size and incidence of steam pop in the canine heart. Heart Rhythm. 6(Suppl. 5), S65 (2009).
- Perna F, Heist EK, Danik SB, Barrett CD, Ruskin JN, Mansour M. Assessment of catheter tip contact force resulting in cardiac perforation in swine atria using force sensing technology. Circ. Arrhythm. Electrophysiol.4(2), 218–224 (2011).
- Kumar S, Morton JB, Halloran K et al. Effect of respiration on catheter-tissue contact force during ablation of atrial arrhythmias. Heart Rhythm. 9(7), 1041–1047 (2012).
- Shah DC, Lambert H, Nakagawa H, Langenkamp A, Aeby N, Leo G. Area under the real-time contact force curve (force-time integral) predicts radiofrequency lesion size in an in vitro contractile model. J. Cardiovasc. Electrophysiol. 21(9), 1038–1043 (2010).
- Kerst G, Weig HJ, Weretka S et al. Contact force-controlled zero-fluoroscopy catheter ablation of right-sided and left atrial arrhythmia substrates. Heart Rhythm. 9(5), 709–714 (2012).
- TOCCASTAR – TactiCath Contact Force Ablation Catheter Study for Atrial Fibrillation.http://clinicaltrials.gov/ct2/show/NCT01278953
- THERMOCOOL® SMARTTOUCH™ Catheter for the Treatment of Symptomatic Paroxysmal Atrial Fibrillation. http://clinicaltrials.Gov /ct2/show/NCT01385202
- Clinical Evaluation of Contact™ Therapy™ Cool Path™ Cardiac Ablation System in Conjunction With EnSite Velocity Contact™ Technology for the Treatment of Typical Atrial Flutter (CONTACT AFL).http://clinicaltrials.gov/ct2/show/NCT01401361
▪ Websites