Image Article - Clinical Practice (2022) Volume 19, Issue 1
Ogilvie's syndrome with colonic perforation: A rare complication
- Corresponding Author:
- Wael Ferjaoui
Department of General Surgery, Mongi Slim University Hospital, Faculty of medicine of Tunis,Tunisia
E-mail: farjaouiwael4@gmail.com
Received: 18 January, 2022, Manuscript No. M-51794 Editor assigned: 21 January, 2022, PreQC No. P-51794 Reviewed: 23 January, 2022, 2022, QC No. Q-51794 Revised: 25 January, 2022, Manuscript No. R-51794 Published: 30 January, 2022, DOI. 10.37532/fmcp.2022.19(1).1849- 1850
Abstract
Description
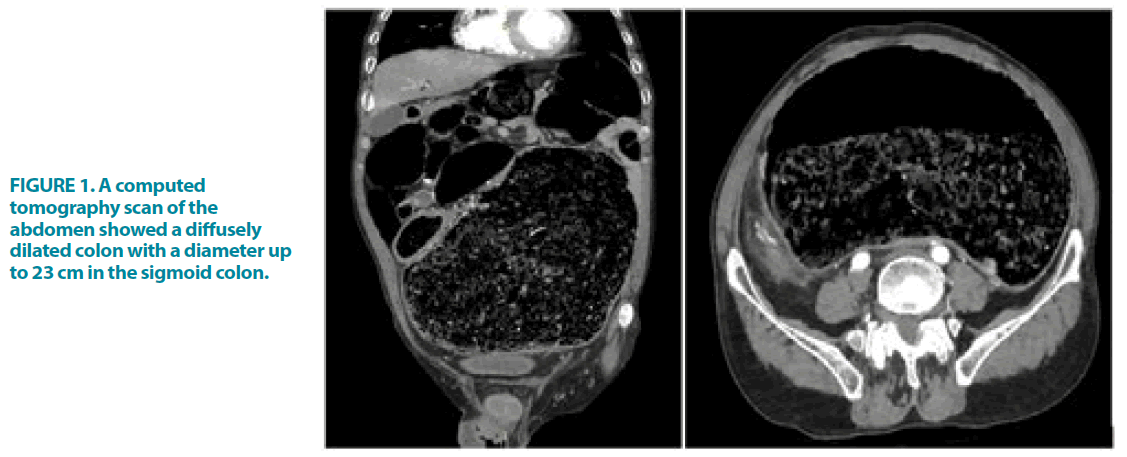
We present the case of a 55-year-old male with a past medical history of diabetes mellitus and hypertension, who presented to the emergency room with chronic constipation and abdominal distension for a few months. He reported that his abdominal girth increased significantly the past few days, causing breathing and walking problems. At the physical examination, he was tachypneic and the abdomen was markedly distended. A computed tomography scan of the abdomen showed a diffusely dilated colon with a diameter up to 23 cm in the sigmoid colon, which occupied almost the entire abdominal cavity (FIGURE 1). Ogilvie’s syndrome was the most likely diagnosis. Few minutes later, he developed hemodynamic instability, and the physical examination showed abdominal contracture. Emergent laparotomy was performed. Surgical exploration found a stercoral perforation of the sigmoid colon. Peritoneal lavage and Hartmann’s procedure were done. The patient died a few hours after surgery.
Acute colonic pseudo-obstruction, also known as Ogilvie’s syndrome, refers to pathologic dilation of the colon without evidence of underlying mechanical or anatomic cause. It is primarily occurring in older adults with multiple underlying comorbidities [1]. The exact pathophysiology remains unclear, and no effective prevention strategy is known. There is probably an imbalance between the parasympathetic nerves that often innervate the colon and the sympathetic nerves [2]. Diagnosis is based on clinical and radiologic findings. Perforation is a rare complication, occurring in less than 2.5% of patients. The current management for Ogilvie’s syndrome without peritoneal signs includes acetylcholinesterase inhibitors (such as neostigmine) associated with decompressive procedures including colonoscopy. When colonoscopic decompression fails or is in perforated forms, as in our case, surgery must be performed [1,3].
References
- Haj M, Haj M, Rockey DC. Ogilvie’s syndrome: management and outcomes. Medicine. 97 (2018).
- Fakirullahoglu M, Peksoz R. Og, Ogilvie Syndrome, and Current Treatment Methods. (2021).
- Jain A, Vargas HD. Advances and challenges in the management of acute colonic pseudo-obstruction (Ogilvie syndrome). Clin Colon Rectal Surg. 25, 37-45 (2012).