Case Report - Clinical Practice (2022) Volume 19, Issue 3
Intrabiliary growth of colic cancer metastasis: A case report and literature review
- Corresponding Author:
- Wael Ferjaoui
Department of General surgery
Mongi Slim University Hospital, Tunisia
E-mail: farjaouiwael4@gmail.com
Received: 20 Janurary, 2022, Manuscript No. fmcp-22-51930 Editor assigned: 22 Janurary, 2022, PreQC No. fmcp-22-51930 Reviewed: 15 February, 2022, QC No. fmcp-22-51930 Revised: 28 February, 2022, Manuscript No. fmcp-22-51930 Published: 07 March, 2022, DOI. 10.37532/fmcp.2022.19(3).1920-1924
Abstract
Introduction: Biliary metastasis of colorectal cancer is a rare association with metastatic liver carcinoma. Differential diagnosis with cholangiocarcinoma can be difficult but must be established in order to offer the best therapeutic strategy. Case presentation: We report the case of a 39 years old woman who has undergone subtotal colectomy with ileocolic anastomosis for occluded sigmoid cancer. Histological examination revealed well-differentiated adenocarcinoma pT3N0M0 with perineural and vascular invasion. Adjuvant chemotherapy was undergone. Three years later, a resection of the segment I for liver metastasis was performed. The microscopic examination concluded to adenocarcinoma from a primary colic cancer. Two years later, wedge resection of two liver nodules of segment IV and VIII and a cholecystectomy was performed. Each time surgical margins were negative. In December 2019, follow-up biology revealed elevated carcinoembryonic antigen. A liver metastasis in segment VIII and a suspicious hepatic hilum ganglion were revealed in imaging. Chemotherapy was conducted. Control imaging showed total regression of segment VIII metastasis and a slight increase in the size of the hilum mass. The patient was operated on preoperative examination showed a mass hanging from the right edge of the hepatic pedicle. Its resection resulted in the loss of substance from the left hepatic duct. Macroscopic examination revealed intrabiliary growth. Histological examination revealed carcinomatous metastasis compatible with the first colic cancer. Resection margins were negative. Conclusion: Intrabiliary growth can have a deceptive presentation. The mechanism and prognosis are not clear. Surgical resection appears to be an acceptable treatment.
Keywords
colic cancer, metastasis, intrabiliary.
Introduction
The liver is a common location of colorectal metastasis [1]. Surgical resection has been accepted as a reasonable treatment for patients with hepatic metastases [2,3]. Intrabiliary growth of liver metastasis originating from colorectal carcinoma is a rare manifestation of metastatic liver carcinoma. This unusual location is thought to be associated with liver metastases in 3% to 10% [3-5]. We report a rare case of intrabiliary carcinoma mimicking a lymph node metastasis.
Case presentation
A 31 years old woman presented with bowel obstruction related to sigmoid cancer. A subtotal colectomy with ileocolic anastomosis. Microscopic examination revealed a welldifferentiated adenocarcinoma, pT3 N0 M0, stage IIA according to the Union for International Cancer Control (UICC) 7th edition. The patient received adjuvant chemotherapy based on FOLFOX for 6 months.
Two years later, the follow-up Computed Tomography (CT) revealed liver metastasis in segment I. patient underwent surgical resection of segment I. The histological examination concluded a liver metastasis of colonic adenocarcinoma. The resection margins were negative. The patient received a second course of chemotherapy based on FOLFOX for six weeks.
In 2018, the patient presented with elevated carcinoembryonic antigen. No disturbance in liver function tests was found. CT showed two liver metastasis in segments IV and VIII. She underwent surgical hepatectomy resecting both metastasis and a cholecystectomy. Surgical margins were also negative and microscopic examination concluded the same ascertainment.
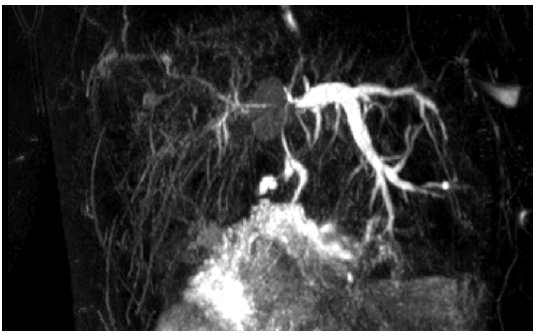
In December 2019, biological follow-up showed an increase in the serum carcinoembryonic antigen level from normal at 5 mg/mL to 11 mg/ mL. Liver MRI showed an infracentimetric liver nodule and dilation of the left intrahepatic bile duct without a detectable obstacle (FIGURE 1).
A PET imaging was then performed showing abnormal uptake in segment VIII of the liver and the hepatic hilum related to a metastatic lymph node (FIGURE 2). Chemotherapy based on 11 courses of Bevacizumab and 13 courses of FOLFIRI was undergone.
In January 2021, reevaluation imaging showed total regression of the liver nodule, an increase in the size of the metastatic Hilary lymph node from 10 mm to 15 mm, and a discrete increase in the dilation of the left intrahepatic bilbiliaryact (8 mm to 11 mm) (FIGURE 3).
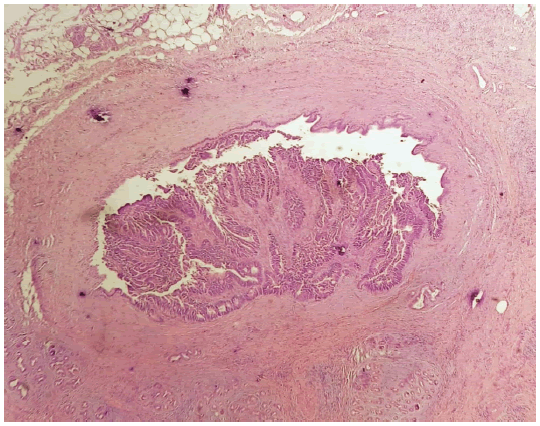
The second course of bevacizumab and FOLFIRI was undergone but curtailed due to hematologic intolerance. IMarchsh 2021, an imagery assessment, consisting of a liver MRI, a PET scan, and a thoracic-abdominal-pelvic CT found similar observations compared to those of January the same year. Serum level of carcinoembrionic antigen was 2829 mg/ml. The decision was to operate on the patient. Through a right subcostal incision. Dissection was laborious. Perioperative examinations found a mass hanging from the right edge of the common hepatic duct and invading the left hepatic bile duct. Its resection resulted in the loss of substance from the left hepatic duct. Reparation of the biliary air duct was done using a patch of the falciform ligament. Macroscopic examination revealed budding epithelial proliferation in a biliary lumen (FIGURE 4).
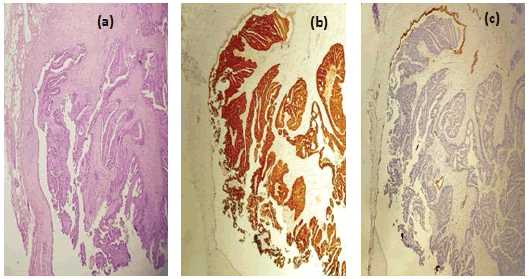
Histological examination showed Tubulopapillary carcinomatous proliferation budding in intra- lumen bordered by a biliary epithelium. This fibrous wall contains also many biliarytype glands. Resection margins were negative. Immunohistochemistry showed strong positivity for CDX2. CK20 positive profile and CK negative, prooving the colorectal origin of the metastasis. The postoperative course was complicated by an under hepatic abscess which responded to percutaneous drainage and antibiotics. The patient was released on day 11.
Discussion
The liver is the first site of metastasis from colorectal cancer [6]. Intrabiliary growth of liver metastasis is a rare association. Sasaki and all reported an incidence rate of intrabilary growth raging between 3.6% and 10.6%[1]. This incidence is still disputed. Japanese studies suggested that the occurrence of intrabiliary microscopic invasion reaches 46% and macroscopic growth reaches 10.6% [5]. However, in 2013, Estrella and all [7] found lower bile duct involvement at a rate of 5.3% prospectively and 3.6% retrospectively. The reason for this discrepancy is unclear and may be related to the different management strategies for colorectal metastases (TABLE 1).
TABLE 1. Intrabiliary growth of liver metastasis in colorectal cancer, literature review.
| Study | Type of study | Year | Number of cases | Bile duct involvement |
|---|---|---|---|---|
| Okano et al. [3] | Retrospective | 1999 | 149 | Macroscopic: 18 (12%) |
| Microscopic: 44 (30%) | ||||
| Kubo et al. [5] | Retrospective | 2002 | 217 | Macroscopic: 23 (10.6%) |
| Microscopic: 89 (40.6%) | ||||
| Estrella et al. [7] | Retrospective/prospective | 2013 | Retrospective: 1114 | Major: 22 (1.9%) |
| Minor: 19 (1.7%) | ||||
| Prospective: 170 | Major: 9 (5.3%) | |||
| Minor: 9 (5.3) | ||||
| Kawakatsu et al. [8] | Case report | 2015 | - | - |
| Yamao et al. [9] | Case report | 2015 | - | - |
| Watanabe et al. [6] | Case report | 2018 | - | - |
| Sasaki et al. [1] | Case report | 2019 | - | - |
| Nakagawa et al. [4] | Case report | 2020 | - | - |
This localization may pose the problem of differential diagnosis with intrahepatic cholangiocarcinoma [8]. Some authors recommend the use of immunohistochemistry to establish the diagnosis of colorectal metastasis by determining the expression of CK7 and CK20 [7]. CK7 negative and CK20 positive expression pattern has a 93% predictive value for the diagnosis of colorectal metastases [4]. In our case, the metastasis mimicked a hilum lymph node that was responsible for dilatation of the left intrahepatic bile ducts. This was an exceptional presentation of colorectal liver metastasis. An aggressive therapeutic strategy based on iterative surgery and chemotherapy was conducted to give the patient the best curative chances.
Okano et al. found that macroscopic bile duct invasion of colorectal metastases was paradoxically associated with a better prognosis than liver metastases with no bile duck extension [3]. In 2002 Kubo proceeded with this work and found similar results [5]. The authors found that this group of patients had well-differentiated phenotypes, no venous invasion, and longer intervals between colectomy and hepatectomy [5]. These findings were confirmed by other papers [2,7,10]. However, a more recent study associated intrabiliary metastasis with a poorer prognosis [6]. Furthermore, Estrella et al. did not find a significant difference between patients presenting bile duct invasion with those who have no invasion [7].
Colon cancer is known to disseminate through three patterns, lymphatic, hematogenous, and peritoneal. However, the mechanism of intrabiliary extension remains unclear [5].
Sano et al. suggested that the mechanism of metastasis was through cancer cell implantation [11]. This may be due to spontaneous shedding of cancer cells or may arise from a complication of percutaneous transhepatic biliary drainage. This theory is not applicable in our case because there was no need for transhepatic biliary drainage. Kawakatsu et al. suggested that the mechanism involves cancer cell implantation rather than hematogenous dissemination. This may be explained by the fragile nature of well-differentiated adenocarcinoma [8]. In this mechanism, Nakagawa et al. supposed that implantation occurred in injured bile ducts or at the site of the resection stump [4]. In our case, there was no injury to the left bile duct reported preoperatively and resection margins were negative. The mechanism remains unclear such as in the case reported by Yamao et al. [9].
Furthermore, intrabiliary invasion of liver metastases can be seen in noncolorectal cancer. But this eventuality remains extremely rare and it appears that this localization is more specifically associated with colorectal cancer [7].
Conclusion
Intrabiliary growth of liver metastases from colorectal cancer remains a rare localization. Still, Japanese authors state that this entity may be largely overlooked. Some authors associated this localization with a better prognosis than patients with liver metastases did. Diagnosis may be challenging. In our case, intrabiliary localization mimicked a hilum lymph node. Surgical resection seems to be the most appropriate treatment. Nevertheless, a clear strategy should be established.
References
- Sasaki S, Nomura Y, Fukutomi S, et al. Intrabiliary growth type of metastasis from colon cancer, 12 years after curative colectomy: A case report. BMC Surg. 19, 8 (2019).
Google Scholar Crossref - Sugiura T, Nagino M, Oda K, et al. Hepatectomy for colorectal liver metastases with macroscopic intrabiliary tumor growth. World J Surg. 30, 1902-1908 (2006).
Google Scholar Crossref - Okano K, Yamamoto J, Moriya Y, et al. Macroscopic intrabiliary growth of liver metastases from colorectal cancer. Surgery. 126, 829-834 (1999).
Google Scholar Crossref - Nakagawa Y, Maeda A, Seita K, et al. Lower bile duct metastasis from rectal cancer after surgery for liver metastasis and intrahepatic bile duct metastasis: A case report. BMC Surg. 20, 137 (2020).
Google Scholar Crossref - Kubo M, Sakamoto M, Fukushima N, et al. Less aggressive features of colorectal cancer with liver metastases showing macroscopic intrabiliary extension. Pathol Int. 52, 514-518 (2002).
Google Scholar Crossref - Watanabe Y, Tamagawa H, Mizushima T, et al. Colon liver metastasis complicated with tumor thrombus in the bile duct: A case report. Int J Surg Case Rep. 49, 238-238 (2018).
Google Scholar Crossref - Estrella JS, Othman ML, Taggart MW, et al. Intrabiliary growth of liver metastases: clinicopathologic features, prevalence, and outcome. Am J Surg Pathol. 37, 1571-1579 (2013).
Google Scholar Crossref - Kawakatsu S, Kaneoka Y, Maeda A, et al. Intrapancreatic bile duct metastasis from colon cancer after resection of liver metastasis with intrabiliary growth: A case report. World J Surg Oncol. 13, 254 (2015).
Google Scholar Crossref - Yamao T, Hayashi H, Higashi T, et al. Colon cancer metastasis mimicking intraductal papillary neoplasm of the extra-hepatic bile duct. Int J Surg Case Rep. 10, 91-93 (2015).
Google Scholar Crossref - Seo SI, Lim S-B, Yoon YS, et al. Comparison of recurrence patterns between ≤5 years and >5 years after curative operations in colorectal cancer patients: Recurrent colorectal cancer. J Surg Oncol. 108, 9-13 (2013).
Google Scholar Crossref - Sano T, Kamiya J, Nagino M, et al. Pancreatoduodenectomy after hepato-biliary resection for recurrent metastatic rectal carcinoma. J Hepatobiliary Pancreat Surg. 30, 516-519 (2000).
Google Scholar Crossref