Research Article - Interventional Cardiology (2019) Volume 11, Issue 1
General anesthesia versus conscious sedation in transcatheter aortic valve replacement: experience from a growing structural cardiology program in the Midwest
- Corresponding Author:
- Bishal Bhandari
Department of Internal Medicine, Southern Illinois University School of Medicine, Springfield, IL
Tel: 2175458000
E-mail: bhandarib88@gmail.com
Received date: January 05, 2019 Accepted date: January 28, 2019 Published date: February 05, 2019
Abstract
Introduction: Transcatheter Aortic Valve Replacement (TAVR) has been established as a viable alternative to surgical aortic valve replacement (SAVR) when treating symptomatic aortic stenosis in intermediate and high risk patients. Historically, general endotracheal anesthesia (GETA) has been the primary form of patient sedation during TAVR. Recently, conscious sedation (CS) has been utilized as a safe option. As there are limited data available comparing these two modalities, it would be helpful to investigate this question further. Methods: To determine the potential benefits of using conscious sedation compared to general anesthesia, 3 outcomes were compared in patients experiencing each method: (1) Total hospital length of stay (LOS), (2) ICU LOS, and (3) occurrence of adverse events (AEs) during hospitalization. Results: Hospital LOS and ICU LOS were found to have a correlation with anesthesia method. CS was correlated with shorter hospital and ICU stays compared to GETA. There were no significant differences between CS and GETA in terms of occurrence of AEs, indicating that the risk of complications was similar for both anesthesia methods. Conclusion: Conscious sedation compared to general anesthesia could potentially be the better alternative for TAVR with no increased adverse events.
Keywords
Transcatheter aortic valve replacement; General anesthesia; Conscious Sedation; Hospital stay
Introduction
Transcatheter Aortic Valve Replacement (TAVR) has become an integral part of the treatment modality of severe aortic stenosis. TAVR has showed similar mortality rates and comparable clinical outcomes to those undergoing surgical aortic valve replacements (SAVR) [1]. It has been shown that TAVR is a reasonable alternative to surgical aortic valve replacement in a patient with intermediate to prohibitive risk patient [2]. A combination of improved patient selection, pre-procedural evaluations and increased operator expertise may be the reasons behind the improvement of outcomes since the procedure’s introduction. Historically, general endotracheal anesthesia (GETA) has been the primary form of patient sedation during TAVR, but conscious sedation (CS) or Monitored Anesthesia Care (MAC) has been found to be feasible in recent times [3]. There is no randomized controlled trial that has evaluated the outcome differences in terms of general anesthesia v/s conscious sedation to this date. Couple retrospective studies have shown encouraging outcomes for conscious sedation cohort [3,4].
TAVR can be safely performed under both conscious sedation and general anesthesia. Under moderate or conscious sedation, the patient's respiratory drive remains intact, they are safely able to maintain their airway, and their brainstem reflexes continue to be functional. Conscious sedation also provides patients who are poor general anesthesia candidates the opportunity to undergo this potentially lifesaving intervention. Our retrospective, cohort study aims to compare conscious sedation to general anesthesia in respect to length of hospitalization, utilization of intensive care units, and occurrence of adverse events.
Methods
Our study was based on TAVR performed at a 500 bed hospital in the Midwest, US. Study was approved by IRB (Institutional Review Board) committee. Patients who underwent TAVR from January 2016 to August 2018 were included on the study (74 total patients). All the procedures were done using GETA until September 2017. Our study included 71 total patients (40 GETA and 31 CS) and excluded 3 patients. Patients who had massive retroperitoneal bleed, displaced valve, or death after complications from prolonged hospital stay were excluded. To determine the potential benefits of using conscious sedation as opposed to general anesthesia during TAVR, we compared 3 outcomes in patients experiencing each anesthesia method: (1) total hospital length of stay (LOS), (2) ICU LOS, and (3) occurrence of adverse events (AEs) during hospitalization. Patients who were not admitted to the ICU had values of zero for ICU length of stay. Adverse events included potential events related to the procedure (i.e., hematoma, left bundle branch block, pacemaker implantation, pericardial effusion, phrenic nerve/hemidiaphragm and blood transfusion).
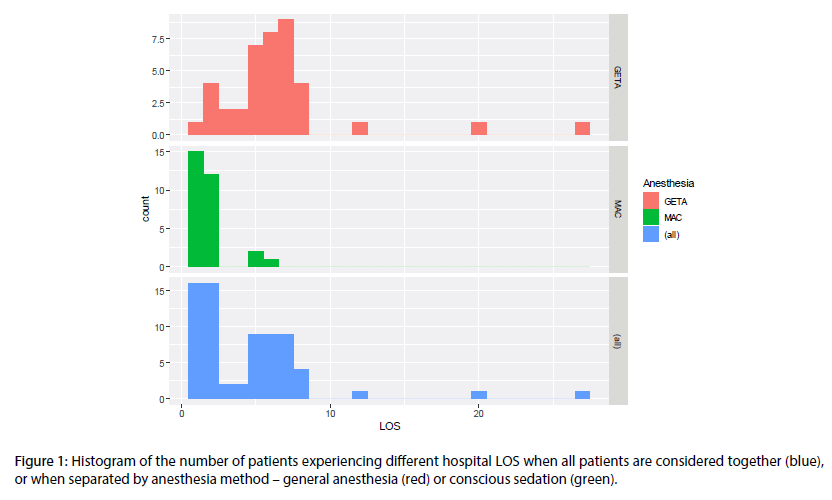
To control for additional factors that may influence our outcomes of interest, we also included age, sex, atrial fibrillation, history of CABG (coronary artery bypass surgery), and PVD (peripheral vascular disease) in a multivariate regression model along with the main effect of anesthesia group. Initial attempts to control for these factors using propensity score weighting yielded higher imbalance between the anesthesia groups. Instead we included all factors in a regression model to adjust for confounding factors while assessing the impact of anesthesia method on our outcomes of interest. Because LOS was measured in days and hospital LOS was over-dispersed in the general anesthesia group (Figure 1), LOS outcomes were analyzed using a negative binomial regression. Because multiple AEs were rare, AEs were treated as a binary (yes/no) variable and analyzed using logistic regression. Exponentiating the model coefficients for a negative binomial and logistic regression yields the expected percentage change in LOS and odds-ratio (OR) of an AE for a one unit change in the predictor, respectively. All analyses were carried out in R statistical software.
Figure 1: Histogram of the number of patients experiencing different hospital LOS when all patients are considered together (blue), or when separated by anesthesia method – general anesthesia (red) or conscious sedation (green).
Results
Our results showed that patients who underwent conscious sedation had significantly shorter hospital and ICU length of stay. CS was associated with 69% shorter hospital stays (mean of 1.8 v/s . 6.5 days for general anesthesia; Tables 1 and 2). Patients receiving conscious sedation had 55% shorter ICU stays (mean of 13 v/s . 39 hours for general anesthesia; Tables 1 and 3). ICU LOS was found to be significantly associated with history of CABG and PVD as well (Table 3). Those with PVD had 114% longer ICU stays (Table 4). Those with a history of CABG had 87% shorter ICU stays. There were no statistical differences found on occurrence of adverse events, indicating that the risk of complications was similar for both anesthesia methods.
| Variable | GETA | MAC/CS | p-value |
|---|---|---|---|
| Aortic valve area, cm2, mean (SD) | 1.81 (6.55) | 0.85 (0.25) | 0.47 |
| Mean aortic valve gradient, mmHg, mean (SD) | 40.4 (15.52) | 34.65 (13.41) | 0.126 |
| LVEF (Left ventricular Ejection Fraction), percent, mean (S D) | 55.77 (11.29) | 57.23 (14.76) | 0.641 |
| Total Costs, $,mean (SD) | 65586.71 (8946.13) | 57921.04 (13781.29) | 0.006 |
| Age, Years, mean (SD) | 81.42 (8.33) | 81.26 (6.58) | 0.927 |
| Hospital LOS, DAYS, mean (SD) | 6.5 (4.56) | 1.83 (1.29) | < 0.001 |
| ICU LOS, HOURS, mean (SD) | 38.88 (29.04) | 13.2 (26.88) | < 0.001 |
| Presence of moderate/severe MR (mitral regurgitation), N (%) | 6 (15.00) | 11 (39.29) | 0.052 |
| Permanent pacemaker, N (%) | 8 (20.00) | 6 (19.35) | 1 |
| Atrial fibrillation, N (%) | 10 (25.00) | 12 (38.71) | 0.299 |
| Previous MI (myocardial Infarction), N (%) | 11 (27.50) | 10 (32.26) | 0.792 |
| History of CABG, N (%) | 2 ( 5.00) | 6 (19.35) | 0.067 |
| PCI (Percutaneous Coronary intervention), N (%) | 13 (32.50) | 6 (19.35) | 0.274 |
| Stroke, N (%) | 7 (17.50) | 3 ( 9.68) | 0.499 |
| PVD, N (%) | 9 (22.50) | 3 ( 9.68) | 0.209 |
| COPD on O2, N (%) | 3 ( 7.50) | 3 ( 9.68) | 1 |
| Serum Creatinine>1.5, N (%) | 8 (20.00) | 8 (25.81) | 0.571 |
| Need for Ventillation post procedure, N (%) | 2 ( 5.13) | 0 (0) | 0.516 |
| Sex, MALE, N (%) | 20 (50.00) | 18 (58.06) | 0.642 |
| ANY Complications, N (%) | 13 (32.50) | 6 (19.35) | 0.289 |
| 1P-value from a t-test without adjusting for confounding factors. | |||
Table 1: Comparison of patient characteristics for individuals undergoing general anesthesia and conscious sedation.
| Variable | Coefficient | Incident Rate Ratio | SE | p-value |
|---|---|---|---|---|
| Intercept | 0.19 | - | 0.83 | 0.82 |
| Age | 0.02 | 1.02 | 0.01 | 0.06 |
| Sex, Male | 0.14 | 1.14 | 0.15 | 0.37 |
| Atrial fibrillation | 0.07 | 1.07 | 0.16 | 0.67 |
| History of cabg | -0.3 | 0.74 | 0.29 | 0.31 |
| PVD | 0.29 | 1.33 | 0.18 | 0.11 |
| Anesthesia, MAC | -1.19 | 0.31 | 0.18 | <0.001 |
Table 2: Multivariate negative-binomial regression model of hospital LOS. Incident rate ratios were calculated by exponentiating model coefficients.
| Variable | Coefficient | Incident Rate Ratio | SE | p-value |
|---|---|---|---|---|
| Intercept | -1.19 | - | 1.23 | 0.33 |
| Age | 0.02 | 1.02 | 0.01 | 0.25 |
| Sex, Male | 0.3 | 1.34 | 0.23 | 0.19 |
| Atrial fibrillation | -0.15 | 0.86 | 0.25 | 0.56 |
| History of cabg | -2.05 | 0.13 | 1.02 | 0.04 |
| PVD | 0.76 | 2.14 | 0.24 | 0.0021 |
| Anesthesia, MAC | -0.79 | 0.45 | 0.28 | 0.01 |
Table 3: Multivariate negative-binomial regression model of ICU LOS; Incident rate ratios were calculated by exponentiating model coefficients.
| Variable | Coefficient | Odds Ratio | SE | p-value |
|---|---|---|---|---|
| Intercept | 0.003 | - | 3.03 | 1 |
| Age | -0.01 | 0.99 | 0.04 | 0.77 |
| Sex, Male | -0.18 | 0.84 | 0.57 | 0.76 |
| Atrial fibrillation | 0.38 | 1.46 | 0.6 | 0.53 |
| History of cabg | -0.55 | 0.57 | 1.18 | 0.64 |
| PVD | 0.52 | 1.69 | 0.7 | 0.46 |
| Anesthesia, MAC | -0.62 | 0.54 | 0.6 | 0.3 |
Table 4: Multivariate logistic regression model of the occurrence of AEs. Odds-ratios were calculated by exponentiating model coefficients.
Discussion
TAVR has evolved as an important strategy in the treatment of severe symptomatic aortic stenosis serving as an alternative to surgical correction in intermediate to prohibitive risk patients. A multi-disciplinary team is tasked with an extensive evaluation of the patient to determine candidacy, appropriate access, and anticipate possible complications. Part of this evaluation includes the choice of anesthesia. Traditionally, GETA has been used for patients undergoing TAVR, with only 5 % of procedures being done using CS in North America according to a study in 2013 [5]. However, with advancement in medical technology and requirement of less cardiovascular and respiratory monitoring, CS is gaining popularity [6-9]. Advantages of the CS includes less catecholamine use, decreased hemodynamic instability, fewer respiratory infections and complications, shorter procedure duration, and better recovery [6,8,9]. Some of these benefits were highlighted by our study as well. There are no randomized controlled trial comparing modes of anesthesia and TAVR. Our study will shed more light into benefits of conscious sedation in terms of length of hospital stay, ICU stay and differences in adverse events between these two modalities.
Our data strongly suggested an association between mode of anesthesia and length of hospital stay. CS group had significant 69% and 55% shorter hospital and ICU stay respectively. Fröhlich et al. performed a meta-analysis which looked at seven studies that compared CS vs GETA in TAVR [6]. They looked at length of hospital stay and procedural time which were both significantly shorter for CS group. Similarly, Toppen et al. studied patients who underwent TAVR (147 GETA and 68 CS) and found that CS had less number of hospital and ICU stay compared to GETA group [8]. Their mean difference in length of hospital stay was about 5.5 days compared to 4.7 days in our study. Shorter LOS with CS is likely multifactorial such as shorter procedure time, no need for intubation, less hemodynamic monitoring, less postoperative infections and management [6,7].
It is also important to assess health care outcomes in these patients for patient safety and adverse outcomes. Our study could not identify any statistically significant difference in the rate of adverse effects between CS and GETA. Common adverse event outcomes were hematoma at the entry site, new left bundle branch block, pacemaker implantation, pericardial effusion, phrenic nerve/hemi diaphragm, and blood transfusion. Meta-analysis by Fröhlich et al. [6] found no statistical difference between occurrence post procedure stroke, AKI or postoperative sepsis in both the groups. Nevertheless, it stated that there was 8% more association pneumonia in GETA v/s CS which was statistically significant. It is also important to note that no other variable like age or history of CABG and PVD was found to have any significant correlation with the adverse effect outcome.
Given health care cost and concerns for affordability, effective and cost efficient health care model is a big emphasis. Study by Toppen et al. showed reduced total cost by about 25% in patients undergoing CS vs GETA in TAVR [8]. Higher length of hospital stays as well as higher cost of GETA likely contributes to higher health care cost for patients undergoing GETA. Given no significant differences in adverse outcomes, the advantages of conscious sedation approach seem logically appealing.
Conclusion
Conscious sedation is associated with shorter hospital and ICU length of stay with comparable adverse outcomes when compared with general anesthesia. Reduced hospital stay and hemodynamic monitoring of CS is tied to more cost effective approach for TAVR.
Conflicting Interests
None
References
- Burrage M, Moore P, Cole C, et al. Transcatheter aortic valve replacement is associated with comparable clinical outcomes to open aortic valve Surgery but with a reduced length of in-patient hospital stay: a systematic review and meta-analysis of randomised trials. Heart. Lung. Circ. 26(3):285-95 (2017).
- Thourani Vh, Neravetla SR. Transcatheter versus surgical aortic-valve replacement in high-risk patients. In: Bernard J. Gersh. Yearbook of Cardiology. Philadelphia, Elsevier Health Sciences, United States of America. pp: 178–179 (2012).
- Motloch LJ, Rottlaender D, Reda S, et al. Local versus general anesthesia for transfemoral aortic valve implantation. Clin. Res. Cardiol. 101:45-53 (2012).
- Mayr NP, Michel J, Bleiziffer S, et al. Sedation or general anesthesia for transcatheter aortic valve implantation (TAVI). J. Thorac. Dis. 7(9):1518–1526 (2015).
- Bufton KA, Augoustides JG, Cobey FC. Anesthesia for transfemoral aortic valve replacement in north america and Europe. J. Cardiothorac. Vasc. Anesth. 27(1):46-9 (2013).
- Fröhlich GM, Lansky AJ, Webb J, et al. Local versus general anesthesia for transcatheter aortic valve implantation (TAVR) – systematic review and meta-analysis. BMC. Med. 10:12-41 (2014).
- Mayr NP, Michel J, Bleiziffer S, et al. Sedation or general anesthesia for transcatheter aortic valve implantation (TAVI). J. Thorac. Dis.7(9):1518-26 (2015).
- Toppen W, Johansen D, Sareh S, et al. Improved costs and outcomes with conscious sedation vs general anesthesia in TAVR patients: Time to wake up? PLoS One.12(4):e0173777 (2017).
- Tchetche D, Biase CD. Local Anesthesia-Conscious Sedation: The Contemporary Gold Standard for Transcatheter Aortic Valve Replacement. JACC. Cardiovasc. Interv. 11(6):579-580 (2018).