Case Report - Clinical Practice (2023) Volume 20, Issue 3
Diagnostic Dilemma: A Case Report of Isolated Pterygomandibular Raphe Rigidity and Review
- Corresponding Author:
- Megarasu Deepanjali
Department of Oral and Maxillofacial Surgery, Meenakshi Ammal Dental College & Hospital, Meenakshi Academy of Higher Education and Research, Chennai 600095, Tamil Nadu, India
E-mail: drdeepanjali.da@gmail.com
Received: 24 July, 2023, Manuscript No. fmcp-23-107854, Editor assigned: 26 July, 2023, PreQC No. fmcp-23-107854 (PQ), Reviewed: 31 July, 2023, QC No. fmcp23-107854 (Q), Revised: 07 August, 2023, Manuscript No fmcp-23-107854 (R), Published: 16 August, 2023, DOI. 10.37532/fmcp.2023.20(3).
Abstract
Pterygomandibular Raphe (PMR) is a tendinous band of tissue which provides attachment to the superior constrictor of pharynx and buccinator muscles. Often overlooked, various anatomical variations of this raphe have been documented in literature. The purpose of this article is to provide an insight into a finding so rare that it has been reported only once in literature. In this report we present an incidental finding of isolated pterygomandibular raphe rigidity which posed difficulties in diagnosis and management. Because of the atypical presentation and obscure etiology, it was challenging to arrive at a diagnosis. As clinicians we must be aware that such anatomical variations exist. Diagnosis and treatment should be provided keeping the patients requirements in mind
Keywords
pterygomandibular raphe, pterygomandibular raphe fibrosis
Introduction
The Pterygomandibular Raphe (PMR) is a band of fib ous tissue that runs from the hamulus to the posterior part of the mylohyoid line in the mandible. It provides attachment to the superior constrictor of pharynx and the buccinator [1]. Thickening of this raphe seems to be a very rare finding, first reported as symptomatic ossification by Warren L. Griffi in 1978 [2]. Various underlying factors could possibly lead to rigidity of this raphe. Oral Submucous Fibrosis (OSMF) is one of the most common reasons for marked rigidity and associated trismus. However, OSMF presents as generalized fib osis of the oral mucosa. Akimoto K et al, studied the structural changes in the oral mucosa due to aging and suggested that fib osis can occur due to aging and this can also be considered as a causative factor [3]. Multiple factors could lead to generalized fib osis of the oral mucosa but the reason for isolated rigidity of the PMR still remains obscure. In this report we present an incidental finding of isolated PMR rigidity which posed difficultie in diagnosis and management.
Case Report
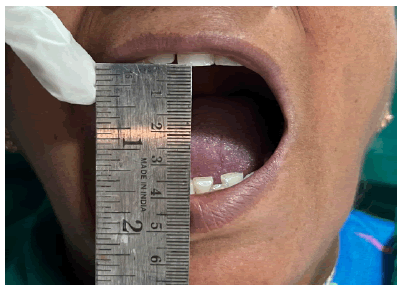
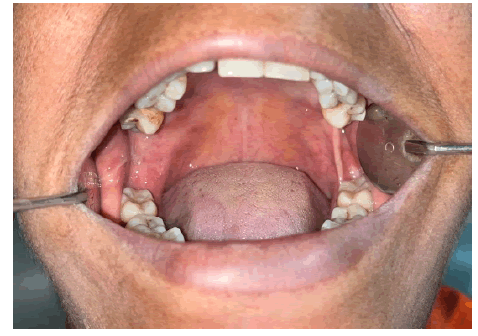
A 50-year-old female patient reported to our institution with a chief complaint of pain in the left lower back tooth region. She gives a history of uneventful extraction of 28 one year back. She is a known case of diabetes mellitus for the past 5 years and is on tab. metformin. On examination, her mouth opening was adequate and recorded as 35 mm (FIGURE 1).Tenderness on percussion was elicited in relation to 36 because of the presence of distal caries. 28 & 26 were missing and a root stump was present in relation to 16. Isolated thickening of the PMR was noticed on the left side (FIGURE 2), however there was no diffe ence in the length of the PMR on both sides and no mucosal changes was observed over the region (FIGURE 3). On palpation patient had mild tenderness over thickened raphe region alone.
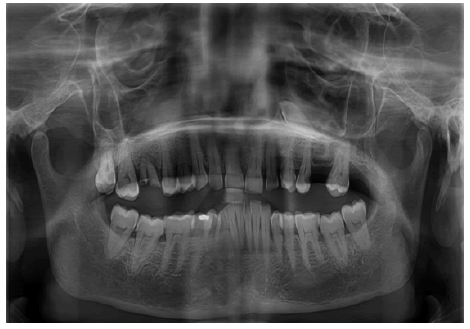
OPG was taken to check the sclerotic changes. OPG revealed no significant abnormalities and the pterygoid hamulus appeared normal with no elongation or bony projection (FIGURE 4). Since it was an incidental finding and the patient did not present with any complaints regarding the same, the mainstay of the treatment was focused on the primary complaint of the patient and dental caries in 36 was restored.
Discussion
The PMR is a tendinous band of fib ous tissue which extends from the pterygoid hamulus to the mylohyoid line in the mandible. It is formed by insertion of two muscles namely superior constrictor of pharynx and buccinator [1]. Kazuyuki Shimada and Raymond F Gasser studied the anatomical variations of the PMR by dissection and reported diffe ent types such as [4]:
Type A- Raphe was broad and triangular in shape and only the upper portion was identifiable.
Type B-PMR was a broad fascial region separating the buccinator and superior pharyngeal constrictor.
Type C- PMR was absent in almost 38% with complete continuity of the muscles.
Despite the varied anatomical presentations of the PMR, only one case of isolated thickening of the PMR has been reported in literature till date [5].
Any inflammation or pathology involving the PMR may lead to pain and trismus. Various factors such as TMJ disorders, trauma, inflammation, presence of tumor, Oral Submucous Fibrosis (OSMF) have been known to cause trismus [6]. OSMF is one of the major causes of generalized fib osis of the oral mucosa leading to trismus. OSMF presents as a generalized fib osis, burning sensation, vesiculation, and ulceration of the oral mucosa [7]. But the reported patient does not give any habit history and the clinical presentation also did not point towards the diagnosis of OSMF. Patient had adequate mouth opening which was recorded as 35 mm.
It has also been suggested that oral mucosa tends to undergo fib osis as age increases. Hence a fib osis due to aging can also be a consideration in this case [3]. This age-related fib osis presents as a generalized appearance rather than isolated thickening of the raphe. This presentation again poses a difficulty in attaining a diagnosi
Griffi in 1978 reported a case of symptomatic ossification of the PMR where the patient presented with severe tenderness over the left pterygoid hamulus region. Surgical exploration revealed a small bony projection extending inferiorly from the pterygoid hamulus region which was excised. Griffi also suggested that an initially an impression of bursitis or tendonitis was made [2]. However, in our present case, there seemed to be no tenderness elicited on palpation over the hamulus region, and OPG revealed no bony projection and sclerotic changes.
In the case reported by Ouchi et al, the patient presented with limited mouth opening because of the rigidity of the right PMR. Hence the PMR was incised and mouth opening was improved by 5 mm [5]. However, in the present case the patient had adequate mouth opening and did not present with any other complaints. So, surgical excision of the thickened raphe was not performed. The close approximity to the pharyngeal wall also has to be kept in mind while performing any surgical intervention near the PMR region.
Generally, for fib osis of the oral mucosa intralesional injection of corticosteroid is considered to be a dependable and safe treatment option. Ekanayaka et al in 2015 evaluated the effecti eness of intralesional corticosteroid therapy in 230 patients suggested that it is one of the most reliable intervention in oral and submucous fib osis [8]. Leena James et al in 2015 suggested that the use of intralesional dexamethasone and hyaluronidase improved the interincisal mouth opening by 6 mm in 92% of the OSMF patients. Hyaluronidase catalyses the breakdown of hyaluronic acid while corticosteroid decreases the fib oblastic proliferation and deposition of collagen thus reducing fib osis [9].
Conclusion and Practical Implications
Because of the atypical presentation and obscure etiology, diagnosis of the underlying pathology was one of the major difficultie encountered. A histological evaluation of fib osed raphe would have given us more insight into the actual diagnosis behind the raphe.
Isolated rigidity of the PMR is a rare finding, but progressive fib osis may cause difficultie such as restricted mouth opening, mastication and speech. Hence treatment has to be provided following proper evaluation and keeping the patient’s chief complaints in mind.
Ethical Approval
Not applicable
Not applicable
Nil
Conflict of interest statement
The authors declare that they have no conflict of interest.
Acknowledgement
Nil
Consent to publish
Written consent to publish was obtained for publication of the patient’s identifiable information.
References
- Susan S., Gray’s anatomy: the anatomical basis of clinical practice.
[Google Scholar] [Cross ref]
- Griffin W. L, Symptomatic Ossification of the Pterygomandibular Raphe. Arch. Otolaryngol. 104(5),298-9(1978).
- Akimoto K, Observations on the structural changes according to aging of oral mucous membrane in the elderly--structure of buccal mucous membrane in the vicinity of angulus oris. Kokubyo Gakkai zasshi. J. Stomatol. Soc., Japan., 71(2),80-94(2004).
- Shimada K, Gasser R. F, Morphology of the pterygomandibular raphe in human fetuses and adults. Anat. Rec. 224(1),117-22(1989).
[Google Scholar] [Cross ref]\
- Ouchi K, Ueno Y, Suzuki H, Jinnouchi A, Trismus caused by pterygomandibular raphe rigidity: A case report and systematic review.
[Google Scholar] [Cross ref]
- Luyk N. H, Steinberg B, Aetiology and diagnosis of clinically evident jaw trismus. Aust. dent. j. 35(6),523-9(1990).
- Sharma SR, Chavan S, Karjodkar FR, et al. Correlation of clinical features in oral submucous fibrosis: A 9-year retrospective study. Ethiop. J. Health Sci. 1,32(1)( 2022).
[Google Scholar] [Cross ref]
- Tilakaratne W. M, Ekanayaka R. P, Herath M, et al. H. Intralesional corticosteroids as a treatment for restricted mouth opening in oral submucous fibrosis. Oral surgery, oral medicine, oral pathol. oral radiol. 122(2),224-31(2016).
- James L, Shetty A, Rishi D, Abraham M, Management of oral submucous fibrosis with injection of hyaluronidase and dexamethasone in grade III oral submucous fibrosis: A retrospective study. J. int. oral health: JIOH. 7(8),82(2015).
[Google Scholar] [Cross ref]