Perspective - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 3
COVID catalyst: telemedicine in rheumatology protects patient care beyond just the pandemic
- *Corresponding Author:
- Adam Kilian
Division of Rheumatology, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC
E-mail: AKilian@mfa.gwu.edu
Abstract
During January 2021, rheumatologic care in Washington DC was affected by both the peak of the COVID-19 pandemic in the United States as well as a deadly insurrection and attack on the US Capitol. As rheumatologists practicing a few blocks from the White House, the authors discuss the crucial role that telemedicine served in delivering healthcare to patients with rheumatic diseases during and after the attack on the US Capitol as threats of violence, physical barriers, military vehicles, and armed troops challenged traditional means of caring for patients. The authors also discuss the role for telemedicine in safely providing future healthcare delivery.
Keywords
telemedicine • telehealth • rheumatology • insurrection • safety • COVID-19 • vaccine • healthcare delivery
Introduction
While much has been written regarding the impact of the COVID-19 pandemic on the delivery of patient care [1], it is often important to recognize that challenges can also present opportunities to catalyze change.
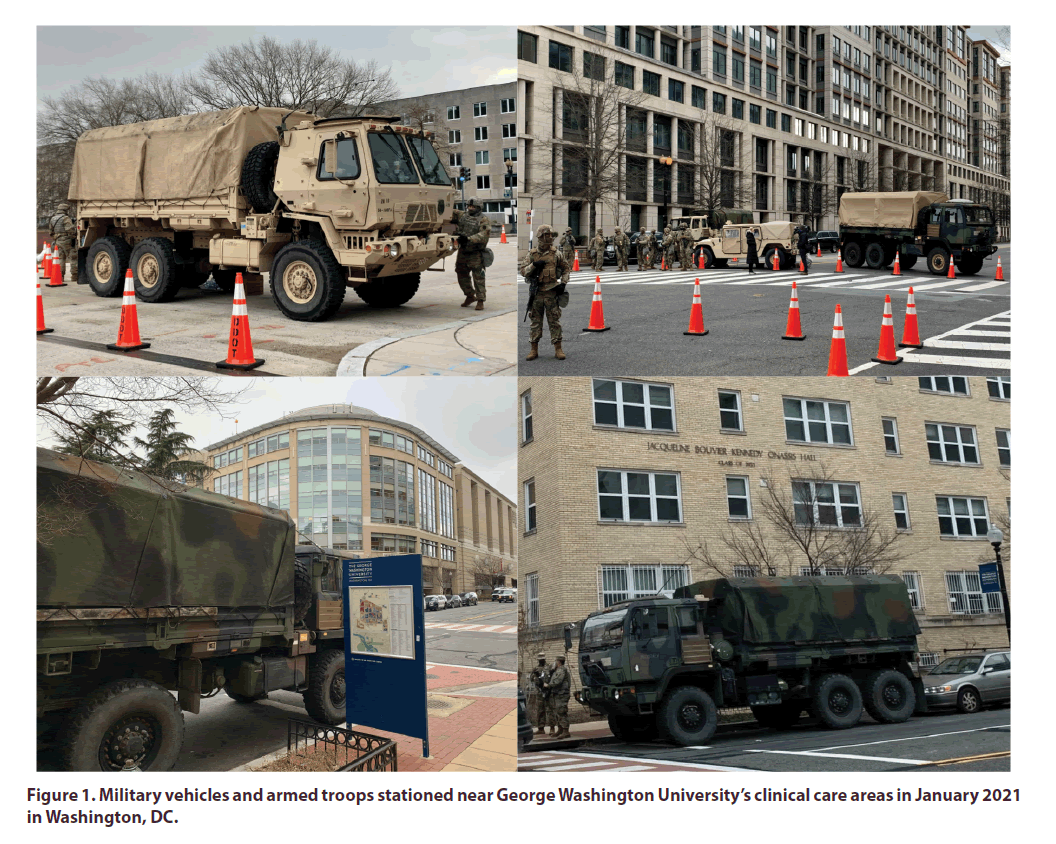
During January 2021 in our nation's Capital, we experienced the impact of not only the ongoing upsurge of COVID-19 cases but also a deadly assault on the Capitol on January 6th, 2021 that aimed to disrupt our constitutional democracy. As clinicians practicing a few blocks from the White House, we witnessed barriers being placed, military vehicles and armed troops stationed throughout our city, including directly adjacent to clinical care areas (Figure 1). These scenes understandably generated a level of anxiety in staff, providers, and patients. Due to safety concerns regarding securing parking lots and patient care areas, our institution was required to shutdown elective clinics - including those in Rheumatology - for several days as military services defended the city and inauguration proceedings. If this had happened in any prior year, our patient care visits and educational meetings would have been cancelled and rescheduled, but in the setting of the pandemic we were able to rapidly transition all patient care and educational activities to online platforms.
Telerheumatology before and during the Pandemic
Telemedicine began in the late 1990s and was subsequently implemented into many aspects of healthcare delivery in the USA and Europe [2, 3]. Telemedicine, however, was not widely used in rheumatology prior to the COVID-19 pandemic. Prior to 2020, few institutions utilized telemedicine to deliver rheumatologic care, and those that did often used it to deliver care to rural areas with success dependent upon technological investments and relationships with rural providers [4].
As the COVID-19 pandemic spread across the globe, widespread cancellations of in-person clinics left our immunocompromised patient population in dire need of safe and effective access to care. All across the USA, the rheumatology community rapidly adopted telemedicine platforms to meet healthcare demands. These efforts were financially feasible on a wide scale due to pressure from the pandemic and resultant fast-track of emergency health policy changes.
Over the course of the pandemic we adopted newer methods of physical examination and were able to confidently treat our patients. Through implanting telemedicine into our rheumatology fellowship curriculum, our fellows learned how to use telemedicine platforms, guide patients through self-examination, and deliver high-quality, secured, and personalized health care through telemedicine to our patients with rheumatic diseases. Our patients have been very appreciative of our continued efforts to provide safe and effective care in these challenging times. A recent survey conducted on 175 patients with various autoimmune rheumatic conditions supported telemedicine as a viable approach even beyond the pandemic [5] and events of the past few weeks have again emphasized the need for continued utilization of this effective tool in medical practice.
Telerheumatology during the Insurrection
The insurrection that took place on January 6, 2021 in the nation’s capital resulted in increased police presence and deployment of thousands of military troops throughout the city as a safety measure ahead of the presidential inauguration. Although the presence of armed forces brought a sense of reassurance, it also created feelings of anxiety, fear, insecurity, and a war-like atmosphere in the city. Seeing armed military troops, tanks, and barricades in our streets is not something many of us rheumatology healthcare professionals have experienced before, and the same is true of many of our patients. As non-military providers, we navigated these unchartered waters in the midst of the COVID-19 pandemic which had already presented considerable challenges to all healthcare workers. We adapted to these unprecedented times to continue to provide quality care while protecting our own safety and the safety of our patients.
As George Washington University Hospital is located in the heart of downtown Washington, DC, commuting to work proved challenging. We needed to carefully plan our daily commute based on road closures and metro station closures limiting access to both motor vehicles and pedestrians. We requested inpatient consultations be called before noon to allow the consultation team ample time to travel to and from the hospital during the daytime to minimize safety concerns. If we were unable to travel to work on a given day, we planned to utilize telemedicine technology to safely provide inpatient consultation services remotely. Finally, one of our primary roles as physicians during this period was to reassure our patients that regardless of what may be going on outside of the walls of the hospital, we would find innovative ways to continue to provide quality healthcare.
Future Public Health Needs for Telemedicine and Health Policy Implications
Many of our patients and fellow providers, remains a new tool that improves access to health care and a powerful alternative to traditional rheumatology care, despite having some limitations. It removes many obstacles for providing care such as geographic borders, difficulty commuting, extreme weather events, or other safety risks as we have recently experienced during the unprecedented attack on our nation’s Capital.
We foresee an ongoing need to offer telemedicine as part of our clinical practice portfolio, since there remain challenges in care delivery as well as limited access to vaccination for many of our high risk immunosuppressed patients who would have to travel on public transport to reach out offices. Many of our patients and fellows providers have expressed preference to conduct clinical care virtually for patients safely sheltered at home until they either receive a vaccine and/ or transmission substantially declines in the region. We advocate that the Centers for Medicare and Medicaid Services and commercial insurers continue long-term coverage of telemedicine services [6] for patients with rheumatic diseases to allow flexibility for maintenance of operations during weather emergencies and other events that threaten the safe delivery of healthcare.
Conclusion
As we continue to balance the complexity of the COVID-19 pandemic, civil unrest, a rheumatology workforce shortage, and ongoing health policy uncertainty, it has become clear that rheumatologists and rheumatology health professionals need to remain innovative and adaptable to the challenges we face [5,7]. The pathway out of the pandemic is likely to be equally as challenging as the events that led us to this point. As rheumatology health professionals and patients continue to advocate for expanding access to rheumatologic care, our experience harnessing telemedicine and tele-education has allowed us to pivot very rapidly in response to both health and safety concerns in our region. Ongoing advocacy is needed to ensure that telemedicine and other innovations become accepted as opportunities to deliver care and improve access for patients in the future.
Disclosures
Conflicts of interest
We declare no conflicts of interest
Funding Support
We declare no financial support.
Authors’ Contributions
Each author has made substantial contributions to both (1) conception and design of the article and (2) drafting the article and revising it critically for important intellectual content. Views expressed are those of the authors and not necessarily those of their affiliations.
References
- Bonfá E, Gossec L, Isenberg DA et al. How COVID-19 is changing rheumatology clinical practice. Nat. Rev. Rheumatol. 17(1), 11–15 (2021).
- Harno K, Paavola T, Carlson C et al. Patient referral by telemedicine: effectiveness and cost analysis of an Intranet system. J. Telemed. Telecare. 6(6), 320–329 (2000).
- Vassallo DJ, Hoque F, Roberts MF et al. An evaluation of the first year's experience with a low-cost telemedicine link in Bangladesh. J. Telemed. Telecare. 7(3), 125–138 (2001).
- Taylor SK, Peoples C. TeleRheumatology Before and During the COVID-19 Pandemic. Pract. Pain. Manag. 21(1), (2021).
- Cavagna L, Zanframundo G, Codullo Vet al. Telemedicine in rheumatology: a reliable approach beyond the pandemic. Rheumatol .60(1), 366–370 (2021).
- Centers for Medicare and Medicaid Services. CY 2021 Physician Fee Schedule final rule (CMS-1734-F). CMS. Gov.(2021).
- Kilian A, Upton LA, Battafarano DF et al. Workforce Trends in Rheumatology. Rheum. Dis. Clin. North. Am. 45(1), 13–26 (2019).