Case Report - Interventional Cardiology (2024) Volume 16, Issue 4
Changing the geometry: Successful PCI of Chronic Total Occlusion (CTO) of Left Anterior Descending (LAD) artery: A case report
- Corresponding Author:
- Abdelaziz Ahmed Abdelaziz
Department of Cardiology, Teachers Hospital, Cairo, Egypt,
E-mail: abdelaziz_1975@yahoo.com
Received date: 25-Jul-2024, Manuscript No. FMIC-24-143225; Editor assigned: 29-Jul-2024, PreQC No. FMIC-24-143225 (PQ); Reviewed date: 16-Aug-2024, QC No. FMIC-24-143225; Revised date: 23-Aug-2024, Manuscript No. FMIC-24-143225 (R); Published date: 30-Aug-2024, ![]()
Abstract
Background: The treatment of Chronic Total Occlusions (CTOs) remains controversial, with various approaches ranging from medical therapy to revascularization strategies. In particular, the Left Anterior Descending (LAD) artery’s involvement necessitates careful consideration due to its significant role in myocardial perfusion. In this report, we highlight a successful intervention utilizing the Subintimal Tracking and Re-Entry (STAR) technique, which is particularly useful in cases where the proximal cap is ambiguous traditional wire escalation strategies are unsuccessful and balloon was used predilate the LAD-diagonal lesion to change the geometry of the lesion and to assist in further clarification of LAD stump.
Patient concerns: A male patient 47 years old, suffered from Hypertension (HTN), and dyslipidemia and had typical chest pain for the last couple of days on minimal exertion. The Electrocardiogram (ECG) and Echo revealed ischemic changes and regional wall motion abnormality.
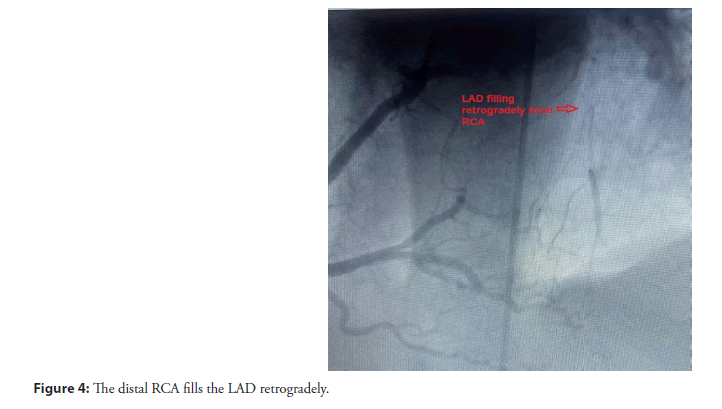
Diagnosis: The coronary angiography results revealed an occluded LAD artery that is filling retrogradely from the Right Coronary Artery (RCA).
Interventions: Percutaneous angioplasty to LAD was done using dual injection and implantation of 2 Drug-Eluting Stents (DES) in LAD using the Subintimal Tracking and Re-Entry (STAR) technique.
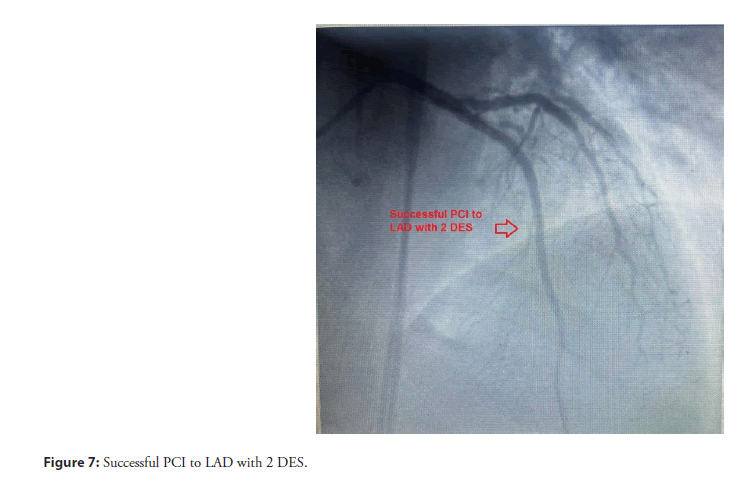
Outcomes: Successful PCI to CTO LAD using 2 DES.
Conclusion: The successful utilization of the STAR technique, augmented by lesion geometry modification through balloon predilation, exemplifies the advancements in PCI strategies for CTO management.
Keywords
Chronic total occlusions • Drug-eluting stents • The subintimal tracking and re-entry
Abbreviations
DES: Drug-Eluting Stent; ECG: Electrocardiogram; HTN: Hypertension; LAD: Left Anterior Descending Artery; LCX: Left Circumflex Artery; LM: Left Main Artery; OM: Obtuse Marginal Branches; PCI: Percutaneous Coronary Intervention; RCA: Right Coronary Artery; CTO: Chronic Total Occlusions; STAR: Subintimal Tracking and Re-Entry; TIMI III: Thrombolysis in Myocardial Infarction- Grade III; RWMA: Regional Wall Motion Abnormalities; IVUS: Intravascular Ultrasound; OCT: Optical Coherence Tomography
Introduction
The management of CTOs in coronary arteries remains one of the most challenging aspects of interventional cardiology. CTOs, defined as complete occlusions of coronary arteries persisting for more than three months, are present in approximately 15%-30% of patients undergoing coronary angiography [1]. These lesions are associated with adverse clinical outcomes, including increased risk of myocardial infarction and mortality [2]. CTOs pose significant technical challenges due to their complex morphology, which often includes calcification, tortuosity, and ambiguous proximal and distal caps [3].
Traditional PCI techniques, such as wire escalation and antegrade dissection re-entry, often face limitations when dealing with ambiguous proximal caps and tortuous lesion anatomy [4]. In such situations, the STAR technique has emerged as a viable alternative, providing a novel strategy for the successful recanalization of CTOs.
The STAR technique, first introduced by Colombo et al., involves intentional subintimal entry and re-entry into the true lumen of the distal vessel, bypassing the occluded segment. This method is particularly advantageous in cases where the proximal cap is ambiguous, and traditional wire escalation strategies have proven unsuccessful [5]. By facilitating the creation of a subintimal space, the STAR technique enables the operator to navigate through challenging occlusions and achieve re-entry into the distal true lumen, thus restoring coronary perfusion [6].
In the presented case, the LAD-diagonal lesion exhibited these challenging features, necessitating an alternative approach. To optimize the intervention, a balloon was utilized for predilation, a strategy that has been shown to enhance lesion crossing and improve procedural success rates.
Balloon predilation serves multiple purposes in this context. Firstly, it modifies the lesion geometry, potentially creating microdissections that facilitate wire passage. Secondly, it augments the visualization of the lesion and adjacent anatomical structures, aiding in the identification of the true lumen and the LAD stump [7]. This dual benefit of balloon predilation enhances the efficacy of the STAR technique, increasing the likelihood of successful reentry and restoring coronary perfusion.
Case Presentation
A 47-year-old Egyptian male was admitted to the cardiology department of Teachers Hospital complaining of unstable angina. The patient had other co-morbidities, including HTN and dyslipidemia, and a history of primary PCI one year ago, during which it was noted that the patient had a totally occluded LAD filling retrograde from the RCA. The patient had typical chest pain on minimal exertion for the last couple of weeks. The diagnosis of the case was confirmed by the ECG that revealed inverted T Wave Lead I and aVL. Furthermore, the Echo showed regional wall motion abnormality in the form of hypokinetic antero-lateral wall and EF 45%.
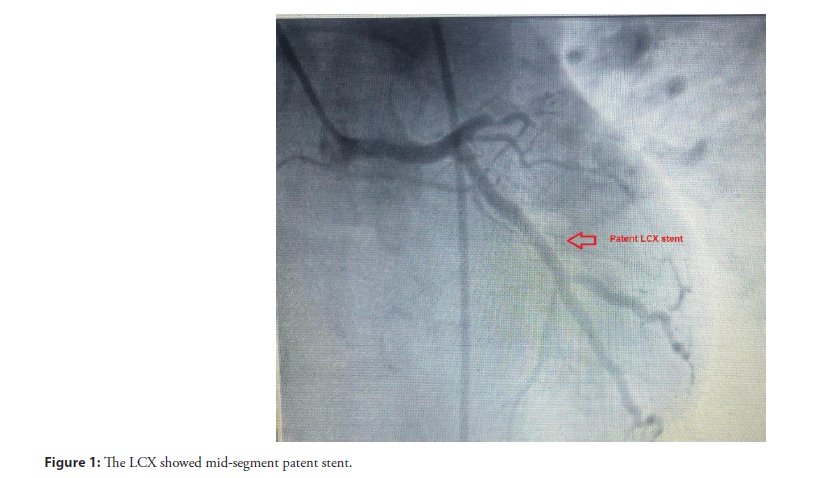
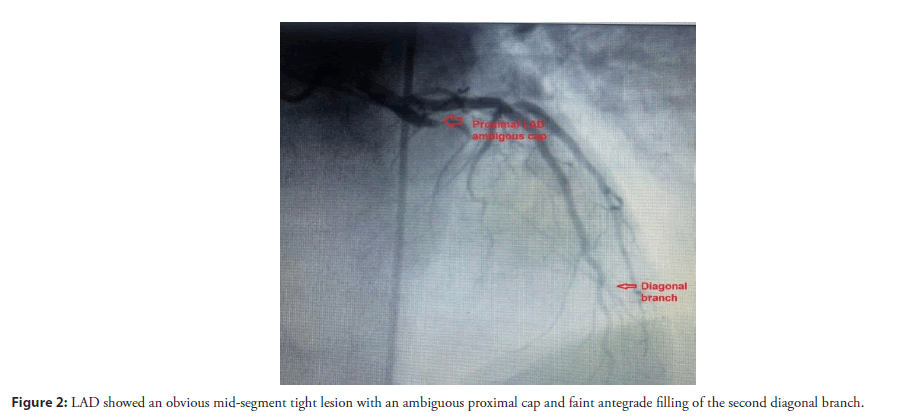
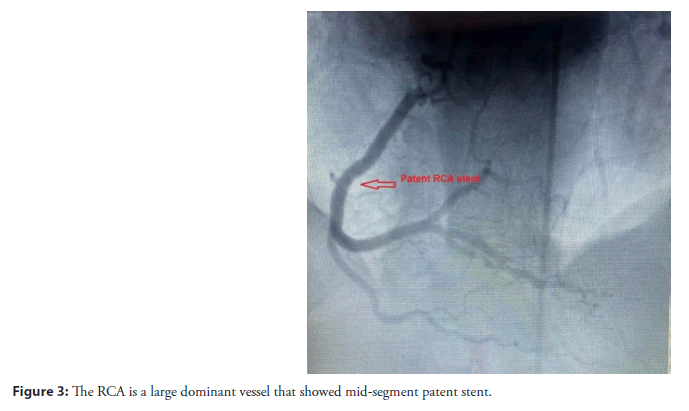
The coronary angiography was done using trans-femoral approach and revealed that LM had an average size and bifurcated into the LAD and Left Circumflex (LCX) arteries without any significant lesions. The LCX showed a mid-segment patent stent (Figure 1). LAD showed an obvious mid-segment tight lesion with an ambiguous proximal cap and faint antegrade filling of the second diagonal branch (Figure 2). The RCA is a large dominant vessel that showed a mid-segment patent stent (Figure 3). The distal RCA fills the LAD retrogradely (Figure 4).
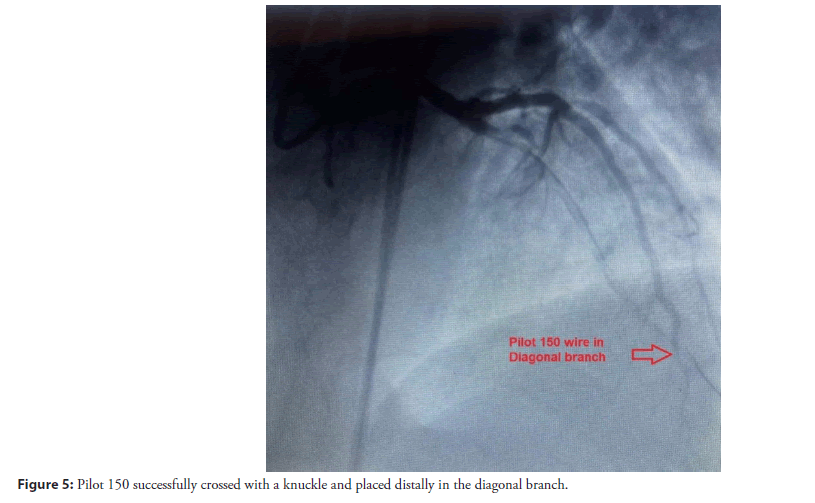
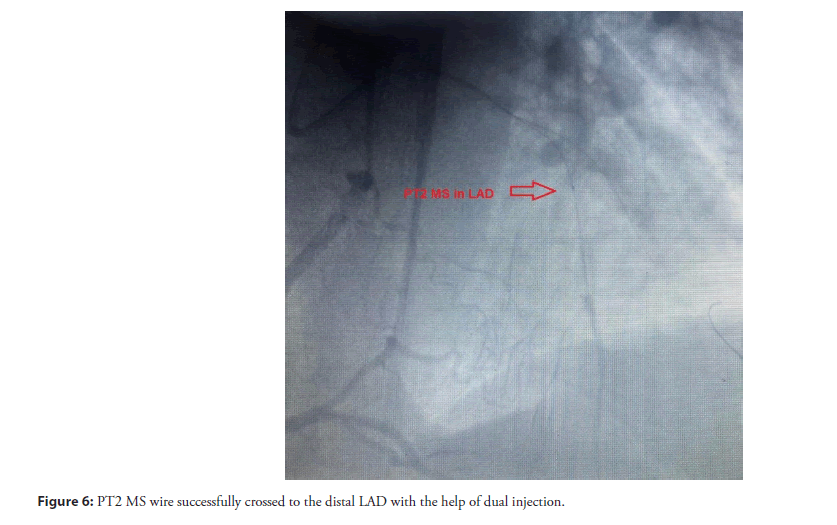
The LM artery was engaged using XB 3.5 guiding catheter and the RCA was engaged with JR4 catheter for retrograde injection. The LAD was tackled with several wires to cross the ambiguous LAD proximal cap including Fielder XT, Pilot 150, and Sion Black wire until finally the Pilot 150 successfully crossed into the second diagonal branch subintimally with a knuckle and was placed distally (Figure 5). A Maverick 1.5 × 15 mm balloon was used to predilate the LAD-diagonal lesion to “change the geometry of the lesion” and to assist in further clarification of the LAD stump.
Successfully the PT2 MS wire crossed to distal LAD with the assistance of dual injection (Figure 6) and 2 DES (Xience V 2.5 × 48 and Xience V 3 × 33 mm) were implanted and post-dilated with a Valista NC 3.5 × 15 mm balloon. Finally, the patient left the Cath lab with TIMI-III flow (Figure 7) and no complications. The patient was followed up in the clinic with improvement of his symptoms and the Echo showed improvement of his EF to 56% and no RWMA.
Results and Discussion
The treatment of CTOs in coronary arteries continues to be a formidable challenge in interventional cardiology. The STAR technique, complemented by balloon predilation, offers a promising strategy for managing complex lesions where traditional wire escalation fails, particularly in the presence of an ambiguous proximal cap. The current case report exemplifies the practical application of the STAR technique and its advantages in overcoming the anatomical hurdles associated with CTOs, specifically in LAD artery-diagonal branch lesions.
The STAR technique, pioneered by Colombo et al., has significantly evolved and is now a cornerstone in the armamentarium for CTO interventions [5]. The technique’s primary advantage lies in its ability to navigate through challenging occlusions by intentionally creating a subintimal space and re-entering the true lumen distal to the occlusion. This method is particularly valuable in cases where the proximal cap is ambiguous, making traditional wire escalation strategies ineffective.
The intentional subintimal entry offers a controlled approach to bypass the occlusion, reducing the risk of vessel perforation and facilitating the advancement of guidewires and other interventional tools. However, the technique is not without its challenges. Successful execution of the STAR technique requires a high level of operator skill and experience, along with precise angiographic visualization to ensure accurate re-entry into the true lumen. Missteps can lead to extensive subintimal dissection, which may complicate the procedure and affect long-term outcomes [8].
Balloon predilation serves as a critical adjunct to the STAR technique, particularly in complex lesion subsets. In the presented case, predilation was employed to modify the geometry of the LAD-diagonal lesion, creating micro-dissections that facilitated subsequent wire passage and enhanced visualization of the LAD stump. This strategic use of balloon predilation has multiple benefits, including the potential to reduce the resistance encountered during wire manipulation and improve the operator’s ability to identify anatomical landmarks [9].
Moreover, balloon predilation can aid in the expansion of the subintimal space, making it easier to navigate through the occlusion and achieve re-entry into the true lumen. This approach aligns with findings from Galassi et al., who demonstrated that balloon predilation could significantly improve procedural success rates and clinical outcomes in patients undergoing PCI for CTOs [7]. By altering the lesion’s structure, predilation reduces the complexity of subsequent steps, thereby enhancing the overall efficacy of the STAR technique.
Clinical implications and outcomes
The successful intervention highlighted in this report underscores the clinical utility of combining the STAR technique with balloon predilation in managing complex CTOs. The patient’s favorable outcome, marked by the restoration of coronary flow and an uneventful recovery, exemplifies the potential benefits of this approach. Importantly, the intervention addressed the anatomical challenges posed by the ambiguous proximal cap and resistant lesion morphology, factors that often preclude successful treatment with conventional techniques [10]. The case also emphasizes the importance of personalized treatment strategies tailored to the specific anatomical and clinical context of each patient. The decision to employ the STAR technique, augmented by balloon predilation, was guided by the lesion’s unique characteristics and the limitations of traditional wire escalation. This individualized approach aligns with contemporary principles of interventional cardiology, which advocate for the use of advanced techniques and technologies to optimize patient outcomes.
Conclusion
The successful utilization of the STAR technique, augmented by lesion geometry modification through balloon predilation, exemplifies the advancements in PCI strategies for CTO management. The strategic combination of these techniques facilitated lesion crossing, enhanced visualization of the LAD stump, and ultimately restored coronary perfusion. This approach underscores the importance of personalized treatment strategies and the potential of advanced interventional techniques in overcoming the challenges associated with CTOs.
As interventional cardiology continues to advance, the ongoing refinement of techniques like STAR and the integration of emerging technologies will play a crucial role in improving patient outcomes. Further research and clinical experience will be essential in optimizing these interventions and expanding their applicability to a broader range of complex coronary lesions.
Future Directions and Research
While the STAR technique and balloon predilation have demonstrated significant promise in the management of complex CTOs, further research is needed to refine these strategies and expand their applicability. Prospective studies and randomized controlled trials could provide valuable insights into the longterm outcomes and potential complications associated with these interventions. Additionally, advancements in imaging technologies, such as Intravascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT), may enhance the precision and safety of the STAR technique by providing real-time, high-resolution visualization of the lesion and surrounding structures.
References
- Guo L, Lv HC, Huang RC, et al. Percutaneous coronary intervention in elderly patients with coronary chronic total occlusions: Current evidence and future perspectives. Clin Interv Aging. 15:771-781 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Fefer P, Knudtson ML, Cheema AN, et al. Current perspectives on coronary chronic total occlusions: The Canadian multicenter chronic total occlusions registry. J Am Coll Cardiol. 59(11):991-997 (2012).
[CrossRef] [Google Scholar] [PubMed]
- Creaney C, Walsh SJ. Antegrade chronic total occlusion strategies: A technical focus for 2020. Interv Cardiol. 15:e08 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Rangan BV, Kotsia A, Christopoulos G, et al. The hybrid approach to intervention of chronic total occlusions. Curr Cardiol Rev. 11(4):299-304 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Colombo A, Mikhail GW, Michev I, et al. Treating chronic total occlusions using subintimal tracking and reentry: The STAR technique. Catheter Cardiovasc Interv. 64(4):407-411 (2005).
[CrossRef] [Google Scholar] [PubMed]
- Brilakis ES, Mashayekhi K, Tsuchikane E, et al. Guiding principles for chronic total occlusion percutaneous coronary intervention. Circulation. 140:420-433 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Galassi AR, Tomasello SD, Reifart N, et al. In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: Insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. EuroIntervention. 7(4):472-479 (2011).
[CrossRef] [Google Scholar] [PubMed]
- Cilia L, Megaly M, Davies R, et al. A non-interventional cardiologist’s guide to coronary chronic total oc clusions. Front Cardiovasc Med. 11:1350549 (2024).
[CrossRef] [Google Scholar] [PubMed]
- Brodie BR, Cooper C, Jones M, et al. Is adjunctive balloon postdilatation necessary after coronary stent de ployment? Final results from the POSTIT trial. Catheter Cardiovasc Interv. 59(2):184-192 (2003).
[CrossRef] [Google Scholar] [PubMed]
- Lim MC. Antegrade techniques for chronic total occlusions. Curr Cardiol Rev. 11(4):285-290 (2015).
[CrossRef] [Google Scholar] [PubMed]