Research Paper - Clinical Investigation (2017) Volume 7, Issue 3
Biomechanical assessment of the reconstruction of the anterolateral ligament during anterior cruciate ligament surgery
- Corresponding Author:
- Martin Komzák
Department of Orthopaedic and Traumatologic Surgery
Hospital Znojmo, MU Dr. Jana Jánského 11, Znojmo
669 02, Czech Republic
E-mail: m.komzak@seznam.cz, martin.komzak@nemzn.cz
Submitted: 04 August 2017; Accepted: 17 August 2017; Published online: 23 August 2017
Abstract
Background: Rotational instability after the anterior cruciate ligament (ACL) injury and subsequent reconstruction may be caused by the rupture of the anterolateral structures of the knee, specifically the anterolateral ligament (ALL). There are more techniques to improve the rotational stability of the knee. The objective of this randomised cohort study was: (1) To evaluate the knee rotational stability after the single-bundle ACL reconstruction (SB) with addition of the ALL reconstruction and to compare it with the double-bundle ACL reconstruction technique (DB). (2) To analyse when the ALL is necessary to reconstruct.
Methods and findings: 60 patients underwent the ACL reconstruction with the average age of 29.5 years. In thirty patient’s knees the ACL was replaced with quadriceps muscle graft using the SB technique in combination with the ALL reconstruction by the gracilis graft (ALL group). With another thirty patients the ACL was reconstructed performing DB technique with the use of hamstring tendons (DB group). The rotational stability was studied before and after the reconstruction of the ACL in time “zero” using the computer navigation system. In the ALL group, the rotational stability was also analysed after the ALL reconstruction. Before the surgery, the mean internal rotational instability (IR) was 18.7° in DB group and 19.1° in ALL groups. After the DB reconstruction, IR stability improved to 10.4°. After the ACL reconstruction in the ALL group, the IR stability was 13.3°. When the ALL was added, the IR stability improved up to 9.8°. In cases where IR stability achieved 12° after the ACL reconstruction, the addition of the ALL reconstruction would not further significantly improve the IR stability.
Conclusions: The SB reconstruction of the ACL using the quadriceps muscle graft in combination with the ALL reconstruction restores the IR stability of the knee to same extent as DB reconstruction does. If the IR stability after the SB reconstruction achieves 12°, the ALL reconstruction is no longer necessary
Keywords
Anterolateral ligament, Anterior cruciate ligament, Rotational stability of the knee
Introduction
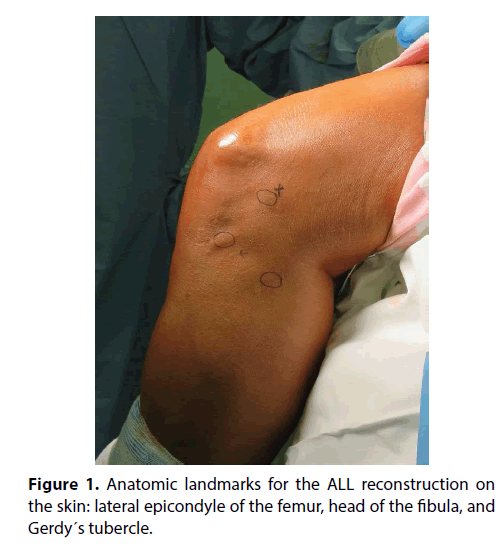
The main goal of the reconstruction of the anterior cruciate ligament (ACL) is the restoration of the anterior-posterior and rotational stability of the tibia in relation to the femur. The position of the femoral attachment of the ACL is more important for the kinematics after the ACL reconstruction [1,2]. The position of the femoral foot-print is well known [3-5]. The biomechanic studies describe the kinematics of the knee joint after various types of the ACL reconstructions [6-8]. Some investigations describe that the double-bundle (DB) reconstruction of the ACL restores the rotational stability more effectively than the single-bundle (SB) technique [9-11]. On the other hand when it comes to the DB technique there are more complications during and after the surgery and it is also more costly [12]. After suffering an ACL injury, rotational instability and subsequent reconstruction may be caused by rupture of the anterolateral structures of the knee, specifically the anterolateral ligament (ALL) [13]. The anatomy of this structure has already been described [14-18]. Its tibial insertion is located between the Gerdy´s tubercle and the head of the fibula. The ALL is inserted on the femoral site approximately 4 mm dorsally and 8 mm proximally to the most prominent point of the lateral epicondyle of the femur (Figure 1) [14].
Figure 1: Anatomic landmarks for the ALL reconstruction on the skin: lateral epicondyle of the femur, head of the fibula, and Gerdy´s tubercle.
The biomechanical function of the ALL is still in the process of being analysed. There are cadaveric studies describing the role of this structure for the anterior-posterior and rotational stability of the knee [13,19,20]. The main role of the ALL is to prevent the internal rotational (IR) instability in between 30° and 90° of flexion of the knee [19].
Reconstruction of the ALL could possibly be a way to improve the IR stability of the knee joint. But there is a lack of studies discussing the IR stability of the knee joint after the ALL reconstruction in vivo. Another way to achieve restoration of the IR stability after the ACL reconstruction would be performing the DB reconstruction. The goals of this study were: (1) To evaluate the knee IR stability after the single-bundle ACL reconstruction accompanied by the ALL reconstruction and to compare it with the double-bundle ACL technique. (2) To analyse when the ALL is necessary to reconstruct.
Materials and Methods
Sixty patients in the average age of 29.5 years (17-40 years; 34 men/26 women; 35 right/25 left knees) were operated due to ACL tears found in one of each patient’s knee between July 2014 and July 2016. The ACL injury was confirmed by magnetic resonance imaging (MRI). All patients signed an informed agreement on being included in this prospective research. The inclusion criteria were very strict: a) The isolated ACL lesion; b) The absence of the previous surgery on the knee joint; c) The age between 17-40 years; d) The body mass index (BMI) less than 30. All other patients with the associated injuries of the tissue around the knee joint such as meniscal lesions, fractures, collateral ligament ruptures as well as cases with systematic diseases were excluded. The cases with only partially torn ACL by arthroscopy were excluded as well.
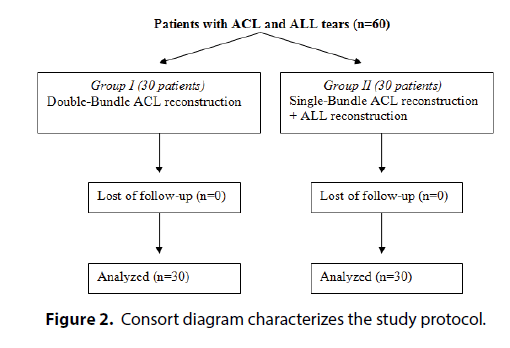
The study has been edited by ClinicalTrials.gov with the number NCT02993679. In the first group, 30 patients underwent a single-bundle reconstruction of the ACL with the bone-tendon graft from quadriceps femoris muscle and the ALL reconstruction using the gracilis tendon graft (ALL group). In the second group, 30 patients had DB reconstruction of the ACL with hamstring tendons (DB group) (Figure 2). The selection of patients for each individual technique of the ACL reconstruction was done randomly using the permuted block randomization by Random Number Generator Software 7.0. The sample size, that is the number of patients included in the study, was determined by power analysis. Due to a minimal change in absolute values during the movement of the tibia against the femur (in mm or in degrees), the minimal sufficient sample size to detect the hypothesized effects was determined to N=60 with the effect size of 90%, the power of 0.90 (β=0.10) and α-level 0.05.
After putting the patient under anesthesia, the femur was fixed using a standard metal holder. Subsequently, diagnostic arthroscopy was performed to confirm the total rupture of the ACL suspected on MRI and also to rule out possible injuries of other intraarticular structures. After such confirmation, the grafts were harvested.
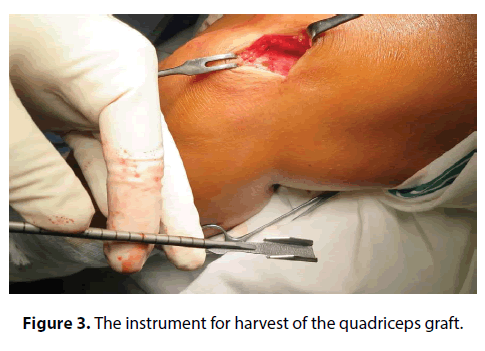
For the DB technique, the skin incision of 5 cm in length was performed on the anteromedial part of the proximal tibia above the anterior board of the pes anserinus. The tendons of gracilis and semitendinosus muscles were identified, separated and harvested with the tendon striper. For the single-bundle reconstruction, the graft was harvested from the quadriceps tendon and the upper part of the patella through the transverse 4 cm skin incision. The special instrumentation was used to separate the tendinous part of the graft from the muscle tendon (Figure 3). The bone-tendon graft was 9 cm long and 9 mm wide. For the ALL reconstruction, the gracilis muscle tendon was harvested. This graft was then folded to be 10 cm long and 6 mm wide. Graft taken from the semitendinosus muscle was used for the anteromedial (AM) bundle reconstruction and the gracilis tendon was used for the posterolateral (PL) bundle. The grafts were adjusted to match the size of 9 cm × 8 mm for the AM bundle and 8 cm × 6 mm for the PL one. Both grafts were folded three times.
During the single-bundle reconstruction, the femoral tunnel was drilled in the anatomic position of the femoral attachement of the ACL [4]. The tibial tunnel was drilled to the centre of the original footprint of the ACL [4]. For the DB replacement, the femoral tunnel for the AM bundle was located behind the lateral bifurcate ridge on the medial side of lateral femoral condyle. The tibial bone tunnel for the AM bundle was located at a distance of 14 mm in front of the posterior cruciate ligament (PCL) attachment slightly medially. The femoral attachment of the PL bundle was positioned between the lateral bifurcate ridge and the lateral intercondyle ridge. The tibial tunnel for the PL bundle was located at a distance of 7 mm in front of PCL attachment slightly lateraly.
During the ALL reconstruction, the 6 mm femoral dock was placed into the point which was situated 8 mm proximally and 4 mm posteriorly to the most prominent point of the lateral epicondyle of the femur. The dock for the tibial attachment of the ALL was drilled posteriorly to Gerdy´s tubercle and anteriorly to the head of the fibula (Figure 1). The fixation of the ALL graft was done with the interference screws, tensioned with a dynamometer set to 85 N in 30° flexion of the knee joint. All grafts for ACL replacements were fixed with interference screws, too.
Subsequently, one bicortical screw for a passive marker fixation was drilled percutaneously into the femur 10 cm above the patella. The second screw was fixed into the ventral side of the tibia, 15 cm distally from the patella. Both screws were equipped with navigation system passive markers. The optical computer navigation system was used for the measurements of the rotational knee stability. Its function is based on reception of infrared rays reflected by the markers using a stereooptic infrared camera. The computer system calculates a relative position of the markers. The resolution specification of the motion measurements of this navigation system is under 1 degree. The navigation system allows evaluation of rotation values of the tibia in relation to the femur (in degrees).
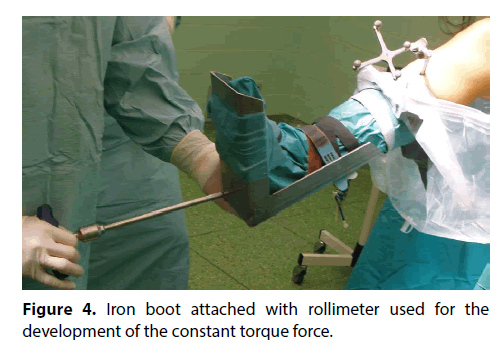
In order to measure the rotational tibial movements, the patient´s foot was fixated to a customized “iron boot” by plastic bands in 10° ankle dorsal flexion to eliminate rotations in the ankle joint. A rollimeter was attached to the boot in the prolongation of the tibial axis. The rotational movement of the tibia with a constant force of 2.5 Nm was produced (Figure 4).
The internal rotation (IR) of the tibia was performed using the rollimeter. The same procedure was repeated for the external rotation (ER). The value of the range of rotation in degrees shown by the navigation device was recorded. Each measurement was repeated three times by the same senior orthopaedic surgeon. Then followed ACL replacement and its fixation with interference screws. In the DB reconstruction the tonisation of the AM bundle was carried out using the dynamometer set to 85 N in 45° flexed knee joint. The PL bundle was tensioned in 10° of flexion with the same force applied. In the single-bundle replacement, the graft was tensioned also by 85 N, but in 30° flexion. After fixation of the graft, the same data as in ACL-deficient condition were collected three times from the navigation device, again with the forces of 2.5 Nm applied in 30° flexion. The same was done after the tensioning and fixation of the ALL in the graft.
After collecting all the data, the stability values after the DB technique were compared with those of the ACL-deficient preoperative knee joint, with the stability of the knee joint after the single-bundle ACL reconstruction and after the ALL reconstruction. In the ALL group, the impact of the ACL and ALL reconstruction on stability was examined separately and compared with the ACL-deficient condition preoperatively.
Statistical analysis
All data were statistically treated by STATISTICA 9.0 software. The description of the deviation of the movement in degrees included mean, standart deviation and range for continuous variables. For statistical evaluation of mean values between the DB and ALL groups and for comparing the internal rotational stability of the knee joint for the single-bundle ACL and the ALL reconstruction, the two-sample t- test was used. For analyzing the optimal value that would signify when the ALL is necessary to restore, IR instability was divided into groups according to the values of IR after single-bundle ACL reconstruction. Then, in each group, the stability was evaluated with comparison with the ALL group using the paired t- test. A P value<0.05 was considered statistically significant.
Results
Internal rotation
Before the surgery, the IR instability did not show any statistically significant difference between the DB and the ALL group (P=0.281). The positive impact on IR stability of the double-bundle ACL reconstruction was more significant than the impact of single-bundle reconstruction alone (P=0.001). After the SB reconstruction, the IR stability improved up to 34%, on the other hand the DB reconstruction resulted in 44% IR stability improvement (when 100% IR stability of the knee joint is 0° theoretically). When the ALL replacement was added, the IR stability increased to average value 9.8° which equals 49% of the stability. This value shows statistically significant difference (P=0.001) between the single-bundle reconstruction alone and with ALL reconstruction in addition. There was no statistically significant difference between the DB and the ALL group after the surgery (P=0.117). All the mean of the IR are specified in Table 1.
| IR (degrees) | DB reconstruction | SB reconstruction | SB+ALL reconstruction |
|---|---|---|---|
| Before the surgery | 18.7 ± 2.9 (14-24) | 19.1 ± 2.5 (14-23) | |
| After the reconstruction | 10.4 ± 2.1 (7-15) | 13.3 ± 2.4 (9-17) | 9.8 ± 1.5 (7-12) |
| P value | P1=0.001 | P2=0.117 | P3=0.001 |
Table 1: Mean internal rotation at 30° flexion of the knee joint in the ACL-deficient knee (before reconstruction) and after the DB, single-bundle and ALL reconstruction. P1 value shows the statistical difference between SB and DB group, P2 shows the statistical difference between DB and ALL group. P3 shows the statistical difference between SB and ALL reconstruction.
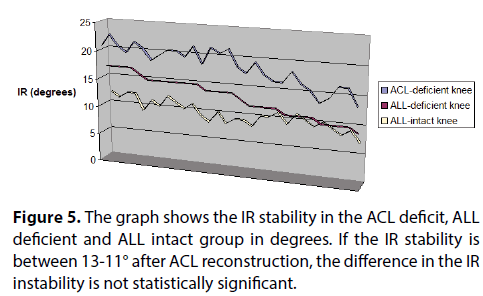
A statistical analysis of absolute values of the IR instability of the knee joints in the ALL group has shown that after ACL replacement using the SB technique, IR stability improved from 23° in average to 9-17° (min-max). After the distribution of these absolute values into the groups based on IR stability after the SB replacement (Tables 2 and 3) and after the comparison with the data after the ALL reconstruction, the improvement of the IR stability of the knee joint is significant when the IR stability is at 11-13° after ACL replacement. If the IR is at less than 11-13°, then the addition of the ALL graft does not further influence the rotational stability significantly enough (P>0.05). This dependence is well seen in Figure 5.
| IR˚ | ||
|---|---|---|
| ACL-deficient knee | ALL-deficient knee | ALL-intact knee |
| 21 | 17 | 12 |
| 23 | 17 | 11 |
| 21 | 17 | 12 |
| 20 | 17 | 12 |
| P value | ˂0.001 | |
| 22 | 16 | 9 |
| 21 | 15 | 11 |
| 19 | 15 | 10 |
| 20 | 15 | 12 |
| 21 | 15 | 11 |
| 21 | 15 | 10 |
| 20 | 15 | 11 |
| 22 | 15 | 9 |
| P value | ˂0.001 | |
| 19 | 14 | 8 |
| 22 | 14 | 10 |
| 21 | 14 | 8 |
| 22 | 14 | 9 |
| P value | 0.002 | |
| 19 | 13 | 9 |
Table 2: Internal rotation at 30° flexion of the knee joint in the ACL-deficient knee (before reconstruction) and after single-bundle ACL and ALL reconstruction divided into the group 17-13° of the IR instability after SB ACL replacement. P values show the statistical difference between SB and ALL IR stability.
| IR˚ | ||
|---|---|---|
| ACL-deficient knee | ALL-deficient knee | ALL-intact knee |
| 18 | 12 | 8 |
| 20 | 12 | 10 |
| 18 | 12 | 10 |
| 17 | 12 | 11 |
| P value | 0,037 | |
| 17 | 11 | 9 |
| 19 | 11 | 11 |
| 17 | 11 | 10 |
| 16 | 11 | 9 |
| P value | 0,080 | |
| 14 | 10 | 10 |
| 15 | 10 | 9 |
| 17 | 10 | 8 |
| 17 | 10 | 9 |
| P value | 0,092 | |
| 14 | 9 | 7 |
Table 3: Internal rotation at 30° flexion of the knee joint in the ACL-deficient knee (before reconstruction) and after single-bundle ACL and ALL reconstruction divided into the group 12-9° of the IR instability after SB ACL replacement. P values show the statistical difference between SB and ALL IR stability.
External rotation
Statistical evaluation has not revealed any significant difference in influence of the single-bundle and DB techniques on the ER stability (P=0.062). In the absolute values, the ER stability improves more after the DB reconstruction of the ACL. After the reconstruction of the ALL, there was no statisticaly significant difference in the ER stability between both groups (P=0.486). The data are shown in Table 4.
| ER (degrees) | DB reconstruction | SB reconstruction | SB+ALL reconstruction |
|---|---|---|---|
| Before the surgery | 17.9 ± 3.4 (12-24) | 17.3 ± 2.9 (13-23) | |
| After the reconstruction | 11.6 ± 2.5 (8-19) | 12.5 ± 2.1 (8-17) | 11.5 ± 2.4 (7-15) |
| P value | P1=0.062 | P2=0.486 |
Table 4: Mean external rotation at 30° flexion of the knee joint in the ACL-deficient knee (before reconstruction) and after the DB, single-bundle and anterolateral ligament reconstruction. P1 value shows the statistical difference between SB and DB group, P2 shows the statistical difference between DB and ALL group.
Discussion
The fundamental findings of this research are: (1) The ALL reconstruction together with single-bundle reconstruction of the ACL provides similar IR stability improvement as the DB technique; (2) The ALL significantly influences the IR stability in the 30° of flexion of the knee joint; (3) The reconstruction of the ALL improves the IR stability from 12° to 7° on average.
These data confirm the hypothesis of Thein et al. [20]. They described the ALL as the “secondary stabilizer” to the ACL. These authors analysed the knee joint stability (anterior-posterior translation and internal rotational movement) in ACL-intact knee, ACL-deficient and ACL/ALL deficient knee joints in twelve cadaver speciments using a robotic manipulator. In the 30° of flexion, the cut of the ACL increased the anterior displacement and the internal tibial rotation with statistical significancy. The cut of ALL resulted in statistically significant increase of the anterior displacement and the internal tibial rotation as well. But the load in the ALL did not increase significantlly in comparison with the ACL-intact knee. The conclusion of the Thein´s study was that the ALL is loaded when the anterior tibial subluxation is greater than 15 mm. In our research, the value of 12° of the IR instability after the single-bundle ACL reconstruction was determined.
In the other in-vitro studies, the ALL was found as an insufficient stabilizer of the internal tibial rotation in the ACL-intact knees at less than 30° flexion of the joint [19]. In our research, 30˚ flexion of the knee was chosen as the flexion angle at which both fiber bundles of the ACL are tightened [21-23].
An in-vivo study that would be objectively analysing the rotational stability of the knee joint after the ALL recontruction in comparison to the different ACL reconstruction techniques still does not exist. Sonnery- Cottet and his colleagues analysed the objective and subjective function of the knee joint in 92 patients who underwent a combined ACL/ALL reconstruction 2 years after surgery [24]. Lysholm score, KOOS, IKDC and Tegner activity score were studied. Pivot shift test and anterior tibial displacement test using a rollimeter were done. These authors demonstrated that the combination of the ACL and ALL reconstruction is effective procedure to improve the function of the knee joint, in fact the improvement of the grade of the pivot shift phenomenon.
In our objective research a very precise measurement device (i.e. computer navigation) was used, the grafts were tensioned always by the same force using the dynamometer, the rollimeter was used to develop the same torsion force in all cases, the number of patients was sufficient in both groups enough for us to compare the SB and DB techniques and patients were selected at random.
The insufficiency of this study is the number of patients in the ALL group for analysing the optimal values to determine when the ALL is necessary to restore. In the group with 13° IR instability after SB reconstruction, only one patient was recorded.
Therefore statistical analysis is not possible. But, the value of 12° IR instability after SB reconstruction shows the borderline where the stability improves (P=0.019). Another part in which this study is lacking is the fact, that in the DB group, the semitendinosus and gracilis tendons were harvested whereas in the ALL group only the gracilis tendon was harvested. The active rotational stability could be slightly influenced by this fact. But first of all the main goal of this study was to evaluate the passive rotational stability of the knee joint in moment “zero”. The DB reconstruction of the ACL is the more difficult technique with more possible complications involved in the perioperative and postoperative period [25,26]. The combination of the single-bundle reconstruction of the ACL with the ALL replacement can be another way to restore the rotational stability of the knee joint without higher risk of complications. Furthemore, semitendinosus muscle remains in situ, its proprioception is preserved. The graft from quadriceps muscle tendon shows some advantages in comparison to the other autografts: two times greater cross-section then the distal patellar bone-tendon-bone graft [27], higher density of collagen fibrils compared to patellar tendon [28], better healing of the bone part of the graft in the bone tunnel compared to hamstring tendons and lesser donor-site morbidity and anterior knee pain in comparison with patellar bone-tendon graft [29,30].
Collected data lead us to conclusion that the DB reconstruction of the ACL stabilizes the knee joint in terms of IR better than the single-bundle reconstruction [8]. The addition of the ALL reconstruction to the single-bundle reconstruction of the ACL restores the rotational stability of the knee joint similarly as the DB technique. The ALL reconstruction together with the single-bundle reconstruction of the ACL can be safely used to restore the IR stability of the knee joint. ALL reconstruction is only necessary if the ACL replacement is not sufficient for the IR stability, i.e. if the remaining IR instability of the knee joint is higher than 12° under 2.5 Nm torque force.
Acknowledgements
Not applicable
Competing Interests
The authors declare that they have no competing interests.
Funding
No funding had role in the design of the study.
References
- Monaco E, Ferretti A, Labianca L, Maestri B, Speranza A, Kelly MJ. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol. Arthrosc. 20: 870-877 (2012).
- Lorbach O, Pape D, Zerbe T, Busch L, Kohn D. Influence of the anteromedial and posterolateral bundles of the anterior cruciate ligament on external and internal tibiofemoral rotation.Am J Sports Med. 38: 721-727 (2010).
- Steckel H, Fu FH, Baums MH, Klinger HM. Arthroscopic evaluation of the ACL double bundle structure. Knee Surg Sports Traumatol Arthrosc. 17: 782-785 (2009).
- Forsythe B, Kopf S, Wong AK, Martins CAQ, Anderst W, Tashman S. The Location of Femoral and Tibial Tunnels in Anatomic Double-Bundle Anterior Cruciate Ligament reconstruction Analyzed by Three-Dimensional Computed Tomography Models. J Bone Joint Surg Am. 92: 1418-1426 (2010).
- Martins CAQ, Kropf EJ, Shen W, van Eck CF, Fu FH. The Concept of Anatomic Anterior Cruciate Ligament Reconstruction. Oper Tech Sports Med. 16: 104-115 (2008).
- Ho JY, Gardiner A, Shah V. Equal Kinematics Between Central Anatomic Single-Bundle and Double Bundle Anterior Cruciate Ligament Reconstructions. Arthroscopy. 25: 464-472 (2009).
- Bedi A, Musahl V, O´Loughlin P, et al. A Comparison of the Effect of Central Anatomical Single-Bundle Anterior Cruciate Ligament Reconstruction and Double-Bundle Anterior Cruciate Ligament Reconstruction on Pivot-Shift Kinematics. Am J Sports Med. 38: 1788-1794 (2010).
- Hofbauer M, Valentin P, Polsky R, et al. Rotational and translational laxity after computer-navigated single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 18: 1201-1207 (2010).
- Colombet P, Robinson J, Kristel O, Franceschi JP, Djian P. Using navigation to measure rotation kinematics during ACL reconstruction. Curr Orthop Pract. 454: 59-65 (2007).
- Song EK, Oh LS, Gill TJ, Li G, Gadikota HR, Seon JK. Prospective comparative study of anterior ligament reconstruction using the double-bundle and single bundle technique. Am J Sports Med. 37: 1705-1711 (2009).
- Hofbauer M, Valentin P, Polsky R, et al. Rotational and translational laxity after computer-navigated single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 18: 1201-1207 (2010).
- Yabroudi MA, Björnsson H, Lynch AD, et al. Predictors of Revision Surgery After Primary Anterior Cruciate Ligament Reconstruction. Orthop J Sports Med. 4: (2016).
- Wroble RR, rood ES, Cummings JS, Henderson JM, Noyes FR. The role of the lateral extraarticular restraints in the anterior cruciate ligament-deficient knee. Am J Sports Med. 21: 257-262 (1993).
- Dodds AL, Halewood C, Gupte CM, Williams A, Amis AA. The anterolateral ligament: anatomy, length changes and association with the Segond fracture. Bone Joint J. 96: 325-331 (2014).
- Claes S, Vereecke E, Maes M, Victor, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 223: 321-328 (2013).
- Claes S, Bartholomeeusen S, Bellemans J. High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg. 80: 45-49 (2014).
- Helito CP, Demange MK, Bonadio MB, et al. Anatomy and Histology of the Knee Anterolateral Ligament. Ortho J Sports Med. 1: (2013).
- Rezansoff AJ, Caterine S, Spencer L, Tran MN, Litchfield RB, Getgood AM. Radiographic landmarks for surgical reconstruction of the anterolateral ligament of the knee. Knee Surg Sports Traumatol Arthrosc. 23: 3196-3201 (2015).
- Parsons EM, Gee AO, Spiekerman C, Cavanagh PR. The biomechanice function of the anterolateral ligament of the knee. Am J Sports Med. 43: 669-674 (2015).
- Thein R, Boorman-Padgett J, Stone K, Wickiewicz TL, Imhauser CW, Pearle AD. Biomechanice assessment of the anterolateral ligament of the knee. J Bone Joint Surg Am. 98: 937-943 (2016).
- Dargel J, Gotter M, Mader K, Pennig D, Koebke J, Schmidt-Wiethoff R. Biomechanics of the anterior cruciate ligament and implications for surgical reconstruction. Strategies Trauma Limb Reconstr. 2: 1-12 (2007).
- Zantop T, Petersen W, Sekiya JK, et al. Anterior cruciate ligament anatomy and function relating to anatomical reconstruction. Knee Surg Sports Traumatol Arthroscop. 14: 982-992 (2006).
- Jordan SS, DeFrate LE, Nha KW, Papannagari R, Gill TJ, Li G. The in vivo kinematics of the anteromedial and posterolateral bundles of the anterior cruciate ligament during weightbearing knee flexion. Am J Sports Med. 35: 547-554 (2007).
- Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BH, Murphy CG, Claes S. Outcome of a Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Technique With a Minimum 2-Year Follow-up. Am J Sports Med. 43: 1598-1605 (2015).
- Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M. Double-bundle ACL Reconstruction Can Improve Rotational Stability. Clin Ortho Rel Res. 454: 100-107 (2007).
- Siebold R. Observations on bone tunnel enlargement after double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 23: 291-298 (2007).
- Harris NJ, Smith DA, Lamoreaux L, Purnell M. Central quadriceps tendon for anterior cruciate ligament reconstruction. Part I: morphometric and biomechanical evaluation. Am J Sports Med. 27: 27-34 (1999).
- Hamer DL, Brown CH, Steiner ME. Hamstring tendon grafts for reconstruction of anterior cruciate ligament: Biomechanice evaluation of the use of multiple strands and tensioningg techniques. J Bone Joint Surf Am. 81: 549-557 (1999).
- Joseph M, Fulkerson J, Nissen C, Sheehan TJ. Short-term recovery after anterior cruciate ligament reconstruction: a prospective comparison of the autografts. Orthopedics. 29: 243-248 (2006).
- Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 17: 971-980 (2001).