Case Report - Interventional Cardiology (2025)
Bailout case of balloon screening technique for lesion behind calcified plaque: A case report
- Corresponding Author:
- Tatsuya Tabata
Department of Cardiology, Urasoe General Hospital, Maeda 1-56-1, Urasoe, Okinawa, Japan
E-mail: peaceatlantic@gmail.com
Received date: 09-Jul-2025, Manuscript No. FMIC-25-167771; Editor assigned: 11-Jul-2025, PreQC No. FMIC-25-167771 (PQ); Reviewed date: 25-Jul-2025, QC No. FMIC-25-167771; Revised date: 01-Aug-2025, Manuscript No. FMIC-25-167771 (R); Published date: 08-Aug -2025, DOI: 10.37532/1755-5310.2025.17(S28).728
Abstract
Background: Eccentric plaques in tortuous arteries can cause dissection during balloon dilation, leading to unintended guidewire placement behind the plaques. We report a case of optical coherence tomography-guided successful stent deployment into the true lumen using a small balloon to screen the dissection cavity.
Case presentation: A 55-year-old man with moderate stenosis of the left anterior descending artery underwent percutaneous coronary intervention. Optical coherence tomography revealed an eccentric calcified lesion and dissection, with the guidewire having advanced behind the plaque. A second guidewire was advanced, and balloon screening ensured precise stent placement. The patient had an uneventful recovery and remains free of ischemic events.
Conclusion: The balloon screening technique successfully enabled true lumen stent placement by occluding the dissection cavity, demonstrating its potential as an effective bailout strategy for guidewire misplacement behind calcified plaques.
Keywords
Case report . Bail-out . OCT . Balloon screening technique
Abbreviations: OCT: Optical Coherence Tomography; PCI: Percutaneous Coronary Intervention
Introduction
Eccentric plaques in tortuous arteries pose the risk of dissection when subjected to balloon dilatation, leading to potential guidewire misplacement behind the plaque. This raises concerns regarding vessel perforation during stent placement and long-term consequences of stent malapposition. Rewiring of the true lumen is crucial, but the guidewire may repeatedly re-enter the dissection cavity once it is formed. The balloonscreening technique, which involves expanding a small balloon within the dissection cavity, may provide a solution to this issue.
Case Presentation
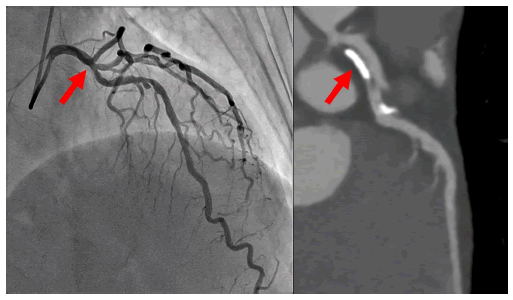
A 55-year-old man with a history of hypertension and smoking was evaluated for intermittent claudication, which revealed moderate stenosis of the proximal left anterior descending artery (Figure 1, red arrow). The lesion showed a significant reduction in fractional flow reserve (0.73, step-up 0.12), and a percutaneous coronary intervention was planned.
Figure 1: Coronary angiography and cardiac computed tomography of the left coronary artery. Moderate stenosis with eccentric calcified plaque can be observed in the proximal left anterior descending artery (red arrow).
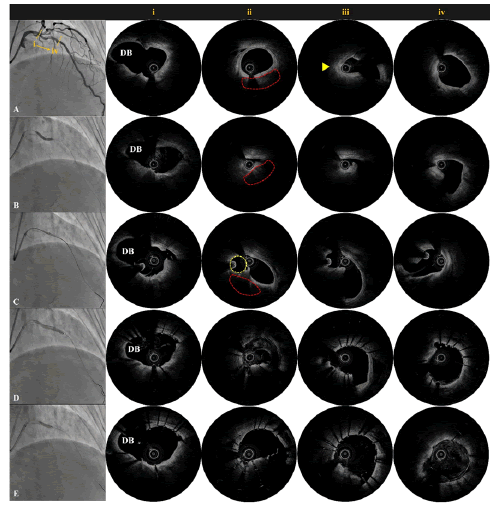
A 7-Fr Launcher EBU 3.5 catheter (Medtronic, MN, USA) was used in the left coronary artery via the radial artery approach. Optical coherence tomography (OCT; Abbott, IL, USA) pullback from the distal segment of the left anterior descending (Figure 2A, Video 1) revealed an eccentric severe calcified lesion around the first diagonal branch (Figure 2A, red arrowhead), with a strong wire bias toward the healthy side just distal to the lesion (Figure 2A, yellow arrowhead). A cutting balloon (WOLVERINE 3.25 Ã 15 mm; Boston Scientific, MN, USA) was used for dilation (Figure 2B) to minimize the risk of injury. Subsequent OCT revealed a dissection originating from the calcification edge, with the guidewire mistakenly entering the dissection cavity (Figure 2B, Video 2). Placing the stent behind the severely calcified plaque was associated with the risks of coronary perforation and stent malposition. Therefore, a second guidewire was inserted into the true lumen. The second guidewire was advanced, and angiography confirmed that it was within the true lumen. The first guidewire was screened using a small balloon (Euphora 1.5 Ã 15 mm; Medtronic, MN, USA) (Figure 2C) to facilitate OCT pullback from the second guidewire to confirm its true lumen position (Figure 2C, Video 3). A drug-eluting stent (COMBO Plus 3.5 Ã 33 mm; OrbusNeich, Hong Kong, China) was deployed while maintaining balloon inflation on the first guidewire (Figure 2D). Post-stent OCT confirmed that true lumen expansion (Figure 2D) and final post-dilation (NC Euphora 3.5 Ã 12 mm; Medtronic, MN, USA) improved stent apposition (Figure 2E). The patient had an uneventful perioperative course and has remained free from ischemic events for 6 months.
Video 1: Optical Coherence Tomography (OCT) at baseline. The target lesion had eccentric calcification. However, strong wire bias toward the healthy intima was observed just distal to the lesion.
Video 2: OCT after ballooning. The guidewire migrated behind the dissected calcified plaque following plain old balloon angioplasty as revealed by OCT.
Video 3: OCT during balloon screening. OCT confirmed dissection cavity sealing, and the second wire was positioned in the true lumen.
Figure 2: Coronary angiography and Optical Coherence Tomography (OCT). DB; First Diagonal branch. (A) The target lesion was identified using OCT, and it had eccentric calcification (ii, area enclosed by red dotted lines). A strong wire bias toward the healthy intima was observed just distal to the lesion (iii, yellow arrowhead). (B) The guidewire migrated behind the dissected calcified plaque following plain old-balloon angioplasty as revealed by OCT (ii, iii). (C) A small balloon was expanded within the dissection cavity (area enclosed by yellow dotted lines). OCT confirmed dissection cavity sealing, and the second wire was positioned in the true lumen (ii, iii). (D) A drug-eluting stent was deployed in the true lumen and verified using OCT (ii, iii). (E) Post-dilation was performed to improve stent apposition (ii, iii).
Discussion
Pathophysiological considerations of dissection in eccentric plaques
Balloon dilation of eccentric calcified plaques creates heterogeneous stress distribution across the vessel wall, with rigid calcified segments and adjacent compliant tissue resulting in concentrated shear stress at the boundary [1,2]. This predisposes to dissection originating from the calcified plaque edge, as demonstrated in our case, despite using a cutting balloon. The OCT finding of strong wire bias toward the healthy intimal side was a crucial predictor of subsequent guidewire misplacement into the dissection cavity following balloon inflation.
Tortuous vessel anatomy further complicates guidewire navigation, as natural curvature creates preferential pathways directing the wire toward areas of least resistance. When combined with eccentric calcification, this significantly increases the likelihood of guidewire entry into dissection planes rather than maintaining true lumen position. Stenting behind a severe calcified plaque poses risks of vessel perforation [3,4] and long-term complications due to stent malapposition [5,6]. Rewiring into the true lumen is preferred; however, guidewires often re-enter the dissection cavity due to their rigidity.
Balloon screening technique: Principles and application
The balloon screening technique represents an innovative solution for reliable true lumen rewiring by physically occluding the dissection cavity with a small balloon. In our case, a 1.5 mm balloon effectively blocked the dissection entrance, enabling secure advancement of a second guidewire into the true lumen under OCT guidance. The technique's success depends on maintaining screening balloon inflation throughout stent deployment to prevent stent migration into the dissection cavity. Real-time OCT monitoring ensures accurate balloon positioning and confirms true lumen guidewire placement. This approach effectively mitigated risks associated with stent placement behind calcified plaques, including vessel perforation and long-term stent malapposition.
Limitations and risks
The balloon screening technique has some limitations despite its effectiveness. Although our case required a 7-Fr guiding catheter for OCT imaging, the technique could potentially be performed with a 6 Fr system if imaging confirmation during balloon screening is omitted. Screening balloon deployment carries risks of dissection propagation and balloon entrapment, with complete balloon removal before post-dilation being mandatory to prevent device entrapment.
Regarding imaging modality selection, OCT requires blood clearance through contrast injection, which may potentially extend dissection planes and compromise patient safety. IVUS may represent a safer alternative as it does not require blood removal and provides adequate visualization for confirming true lumen position, despite its inferior spatial resolution compared to OCT. The technique's applicability remains limited in cases of extensive dissections or when the dissection cavity is too large for effective balloon occlusion.
Conclusion
The balloon screening technique offers an effective bailout strategy for guidewire misplacement behind calcified plaques following coronary dissection. By physically occluding the dissection cavity, this approach enables reliable true lumen rewiring and secure stent deployment, potentially preventing procedural failure in challenging clinical scenarios.
Acknowledgment
We thank the patient for consent to present this case.
Funding
This study did not receive any funding.
Conflicts of Interest
The authors declare no conflicts of interest.
Data Availability Statement
Data supporting the findings of this study are available from the corresponding author upon reasonable request.
Patient Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
References
- Barbato E, Shlofmitz E, Milkas A, et al. State of the art: Evolving concepts in the treatment of heavily calcified and undilatable coronary stenoses-from debulking to plaque modification, a 40-year-long journey. EuroIntervention. 13(6):696-705 (2017).
[Crossref] [Google Scholar] [PubMed]
- Riley RF, Patel MP, Abbott JD, et al. SCAI expert consensus statement on the management of calcified coronary lesions. J Soc Cardiovasc Angiogr Interv. 3(2):101259 (2024).
[Crossref] [Google Scholar] [PubMed]
- Hendry C, Fraser D, Eichhofer J, et al. Coronary perforation in the drug-eluting stent era: Incidence, risk factors, management and outcome: The UK experience. EuroIntervention. 8(1):79-86 (2012).
[Crossref] [Google Scholar] [PubMed]
- Shaukat A, Tajti P, Sandoval Y, et al. Incidence, predictors, management and outcomes of coronary perforations. Catheter Cardiovasc Interv. 93(1):48-56 (2019).
[Crossref] [Google Scholar] [PubMed]
- McDaniel MC, Eshtehardi P, Sawaya FJ, et al. Contemporary clinical applications of coronary intravascular ultrasound. JACC Cardiovasc Interv. 4(11):1155-1167 (2011).
[Crossref] [Google Scholar] [PubMed]
- Shimamura K, Kubo T, Akasaka T, et al. Outcomes of everolimus-eluting stent incomplete stent apposition: A serial optical coherence tomography analysis. Eur Heart J Cardiovasc Imaging. 16(1):23-28 (2015).
[Crossref] [Google Scholar] [PubMed]