Brief Report - Interventional Cardiology (2023)
Atrial extrasystole and left atrial strain: A brief report
- Corresponding Author:
- Jose M. Soler
Department of Cardiology, Hospital Nostra Senyora de Meritxell, Andorra la Vella, Andorra,
E-mail: josepmiquel.soler@gmail.com
Received date: 10-Jun-2023, Manuscript No. FMIC-23-102043; Editor assigned: 13-Jun-2023, PreQC No. FMIC-23-102043 (PQ); Reviewed date: 28-Jun-2023, QC No. FMIC-23-102043; Revised date: 04-Jul-2023, Manuscript No. FMIC-23-102043 (R); Published date: 12-Jul-2023, DOI: 10.37532/1755- 5310.2023.15(S17).428
Abstract
In this short study I summarize my experience with the use of the Left Atrial Strain (LAS) in patients without organic heart disease with palpitations and presence of isolated or repetitive Short Atrial Extrasystole (PACs) including isolated forms of isolated Atrial Fibrillation (AF). For this, I developed a database with 270 patients collected over two years including clinical variables, electrocardiographic with continuous monitoring of three days and conventional echocardiography with the additional contribution of the functional study of the left atrium with two-dimensional LAS of two basal chambers, including the dynamic study with PACs in cases where possible. My most relevant finding was the detection of a case with possible anatomical-functional block in possibly specific intraatrial electromechanical conduction, as well as the potential usefulness of LAS with the incorporation of extrasystole in relation to atrial cardiomyopathy
Keywords
Left Atrial Strain (LAS) • Short Atrial Extrasystoles (PACS) • Isolated Atrial Fibrillation (AF)
Introduction
Traditionally, atrial extrasystole in the absence of organic heart disease has only acquired some cardiological importance in very symptomatic cases or in situations with high arrhythmic load in ambulatory monitoring systems. Recent reviews give it a greater prognostic value with its possible direct involvement in relation to the appearance of atrial fibrillation, embolic complications and overall mortality [1]. The 2D and 3D echocardiography and, especially the study with LAS, allows us to perform a functional approximation of the atrium before, during and after extrasystole in adequate film sequences. This possibility could provide additional data in the initial view performed from an ambulatory cardiology unit. In a recent article, we tried to make an approximation in the functional study of the left atrium using imaging techniques feasible in any routine echocardiographic study [2]. All the variables used in the article can be reviewed but, in Soler, et al., summary, they emphasize the anatomical and functional study of the left atrium with LAS in its three components (reservoir, conduction and active contraction) as well as the conduction time (tissue Doppler) and the electromechanical dispersion calculated automatically between the septal and lateral basal walls of the atrium using the values of the maximum peak of the atrial reservoir [2]. In the last five years, I personally carry out this study in all my echocardiographic records enjoying an experience of around five thousand patients being, in my opinion, the first prospective clinical work that analyzes the dynamic behavior of the PACs studied with 2D LAS.
Methodology
The definition of cardiomyopathy includes multiple concepts that stimulate in-depth research in different scenarios. Undoubtedly Goette, et al. summary is one of them represents the study of PACs and their involvement in the diagnostic and therapeutic strategy from the perspective of ambulatory cardiology [3]. On the other hand, the analysis of LAS in patients without diagnosed organic heart disease implies a significant independence with respect to left ventricular function. In our study, the control group was formed by patients without repetitive atrial salvos (78 patients) being age, left atrial volume and CHAD2DS2-VASC values obtained multivariable statistical significance in relation to the appearance of atrial fibrillation. Among the clinical variables, the greater anxiety among patients in the control group regarding repetitive forms was significant, which could show more initial disorders in the autonomic nervous system and variations in normal LAS values currently not documented [4]. The results obtained with LAS did not obtain statistical significance in the univariate and multivariate study according to age. Other similar studies, such as MESA [5], seem to indicate the relationship between reduced values of LAS components and their association with PACs.
The existence of left atrial asynchrony has been related to the presence of fibrosis and recurrent atrial fibrillation in multiple studies. However, there is little scientific documentation of the values obtained by segmental LAS among the general population [6]. Regardless of the methodology used, they obtained a cut-off value of 42 ms by 57 ms obtained by us, although without statistical significance correlating age. These findings have been reproduced by more sophisticated imaging techniques such as scanning or cardio resonance as well as electrophysiological mapping, all of which are costly and not applicable in the first line of diagnosis [7].
Results and Discussion
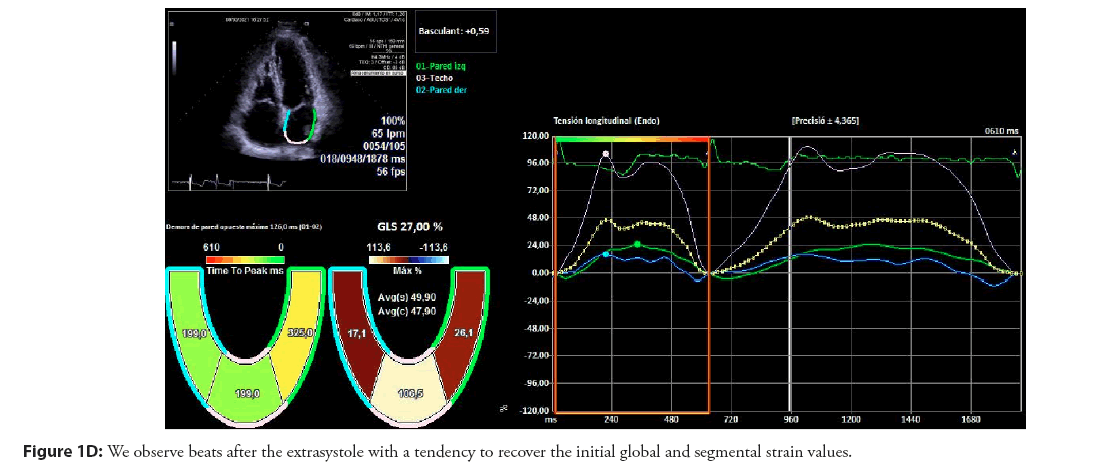
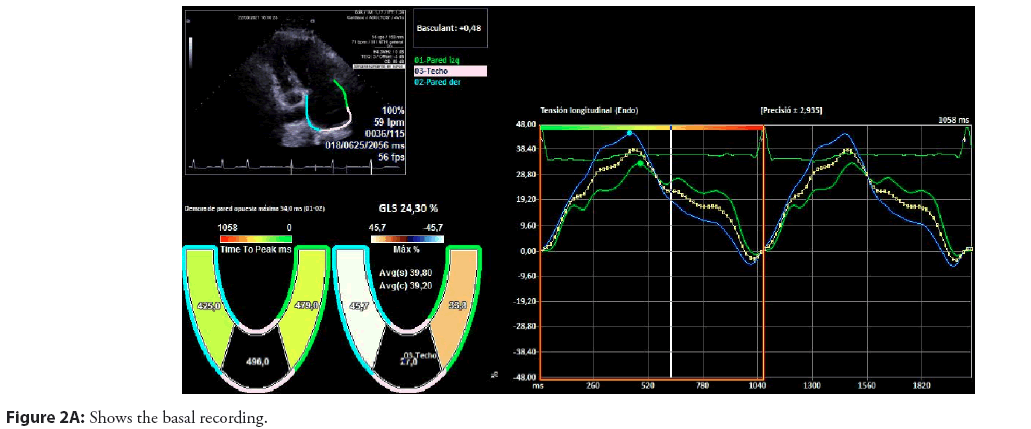
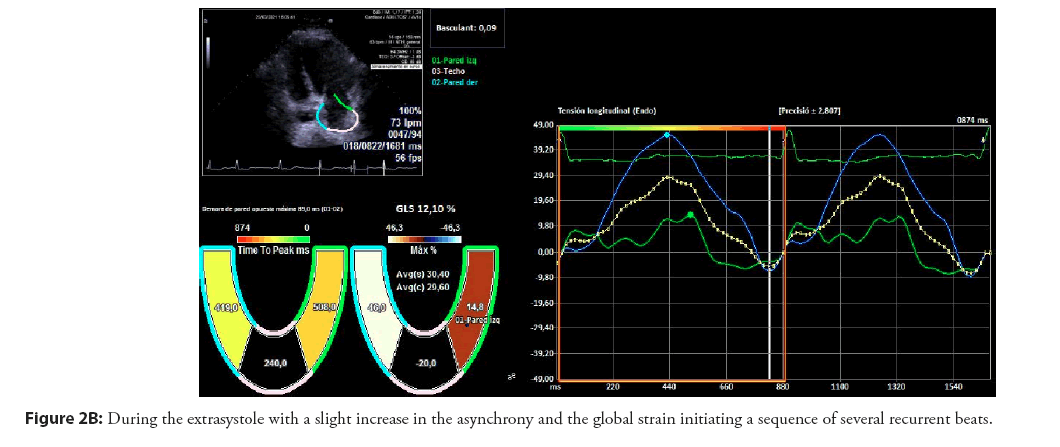
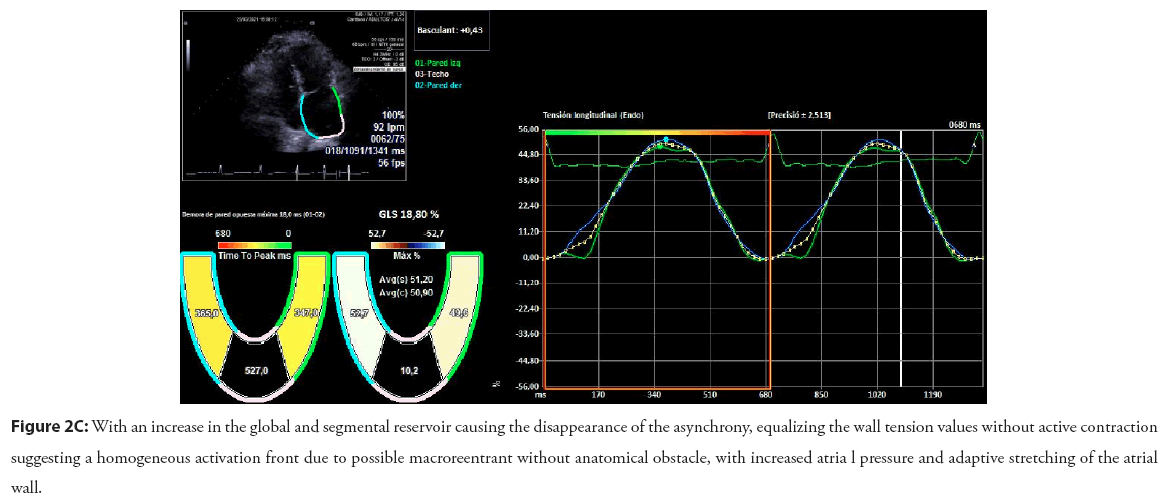
In Figures 1 and 2, we illustrate the graphic study of segmental LAS in two patients that we have chosen as most relevant. The first patient, without documented atrial fibrillation and with 3D echocardiography showing a left auricula with normal morphology and volume, showed a possible intraatrial anatomical block. In addition, the segmental curves of the LAS suggest the birth of extrasystole near the pulmonary veins. Unfortunately it could not be adequately mapped in the electrophysiological study due to the rapid fall in atrial fibrillation. Subsequent follow-up of the patient for two years after ablation has shown persistence of high-density atrial extrasystole with moderately symptomatic short repetitive forms without evidence of atrial fibrillation. This patient has not consented to a new electrophysiological study. Analysis with LAS continues to show the same initial activation pattern. In the second case, we observe the disappearance of the active atrial contribution and the homogeneity of the pressures as well as the progressive tendency to recover the initial values of the LAS prior to the PACs. All this is directly linked to the mechanisms of atrial adaptation after PACs and, therefore, provide new objectives in the study of left atrial cardiomyopathy.
Patient 1
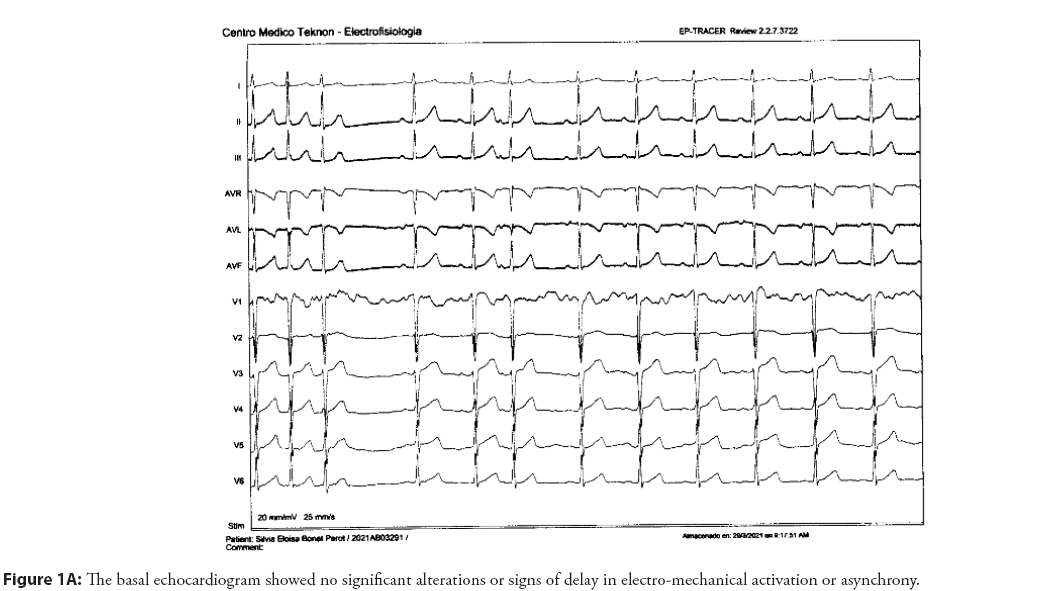
55-Year-old female patient with elevated blood pressure treated with ACEi, family history of ablated atrial fibrillation, and atrial extrasystole of moderate density documented for the last two years with no repetitive forms with clinical limitation to effort without obvious structural heart disease. The basal electrocardiogram showed no alterations to the P wave and the extrasystole was positive on the lower side and V1 with negativity in aVL suggestive of an origin in the posterior left superior pulmonary vein Figure 1A-1D.
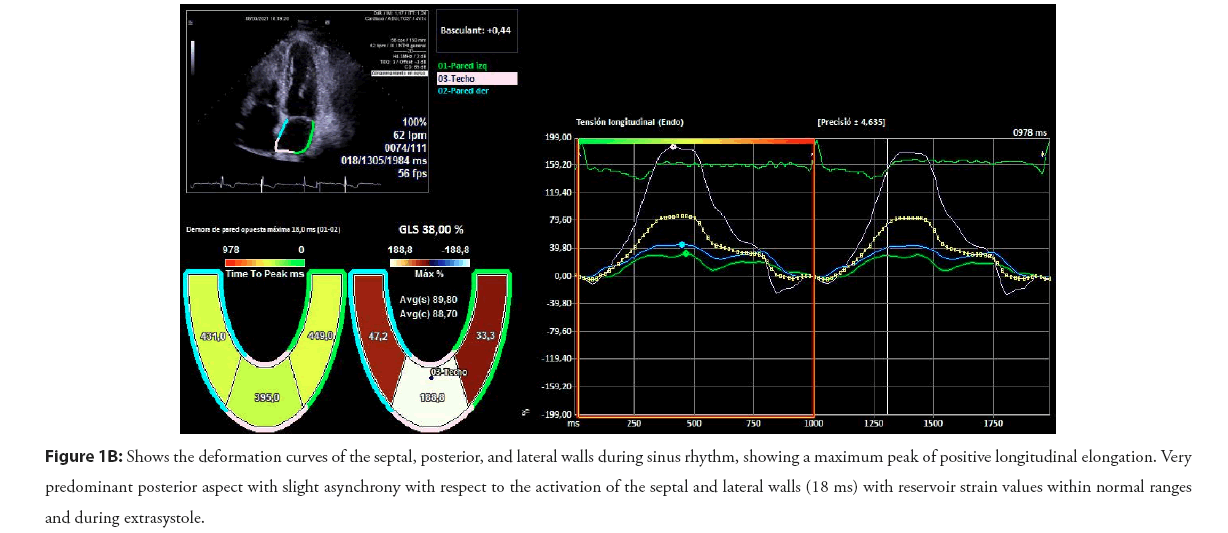
Figure 1B: Shows the deformation curves of the septal, posterior, and lateral walls during sinus rhythm, showing a maximum peak of positive longitudinal elongation. Very predominant posterior aspect with slight asynchrony with respect to the activation of the septal and lateral walls (18 ms) with reservoir strain values within normal ranges and during extrasystole.
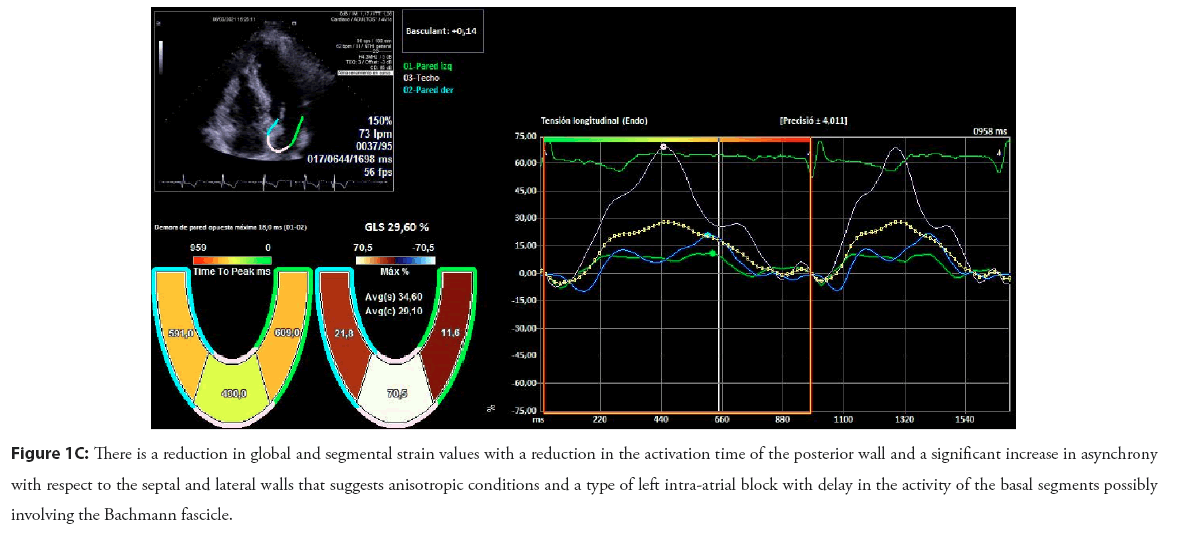
Figure 1C: There is a reduction in global and segmental strain values with a reduction in the activation time of the posterior wall and a significant increase in asynchrony with respect to the septal and lateral walls that suggests anisotropic conditions and a type of left intra-atrial block with delay in the activity of the basal segments possibly involving the Bachmann fascicle.
Patient 2
75-year-old patient, hypertensive with atrial extrasystole bursts with no evidence of atrial fibrillation with an electrocardiograph P wave of 122 ms and an electrocardiogram which showed slight left atrial dilation (35 ml/m2) with no increase in the electromechanical conduction time with asynchrony in the longitudinal tension between the septal and lateral walls (54 ms, 5% relative to the RR) Figure 2A-2C.
Figure 2C: With an increase in the global and segmental reservoir causing the disappearance of the asynchrony, equalizing the wall tension values without active contraction suggesting a homogeneous activation front due to possible macroreentrant without anatomical obstacle, with increased atria l pressure and adaptive stretching of the atrial
In an analysis of my experience with the LAS technique in the study of atrial extrasystole, I would highlight the following aspects:
1. The images obtained from the segmental strain curves aretemporally reproducible in each patient.
2. There are patients with extremely high global and segmentalstrain values (up to five times the normal range) that isprobably related to autonomic dysfunction and initial degrees of atrial cardiomyopathy. Such sharp deviations should notbe overlooked and should be studied further.
3. This study methodology, duly improved with technologicaladvances, should be included in all echocardiography studiesin primary cardiology centers.
Conclusion
The dynamic study of PACs using LAS is a useful measure in the study of left atrial cardiomyopathy. Advances in engineering should contribute to the improvement of the technique and make it applicable in routine studies. The quantification of new parameters in LAS can contribute decisively to a better understanding of left atrial function.
References
- Yang M, Lin Y, Cheng H, et al. Excessive supraventricular ectopic activity and the risk of atrial fibrillation and stroke: A systematic review and meta-analysis. J Cardiovasc Dev Dis. 9(12):461 (2022).
- Soler JM, García-Parés G, Valero O, et al. Assessment of short forms of recurrent atrial extra systoles by echocardiography with left atrial strain in ambulatory patients without organic cardiopathy. Arch Cardiol Mex. 93(2):172-182 (2023).
- Goette A, Kalman JM, Aguinaga L, et al. EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: Definition, characterization, and clinical implication. J Arrhythm. 18(10):1455-1490 (2016).
- Pathan F, D'Elia N, Nolan MT, et al. Normal ranges of left atrial strain by speckle-tracking echocardiography: A systematic review and meta-analysis. J Am Soc Echocardiogr. 30(1):59-70 (2017).
- Huber MP, Pandit JA, Jensen PN, et al. Left atrial strain and the risk of atrial arrhythmias from extended ambulatory cardiac monitoring: MESA. J Am Heart Assoc. 11(21):e026875 (2022).
- Karsum EH, Andersen DM, Modin D, et al. The prognostic value of left atrial dyssynchrony measured by speckle tracking echocardiography in the general population. Int J Cardiovasc Imaging. 37:1679-1688 (2021).
- Marincheva G, Iakobishvili Z, Valdman A, et al. Left atrial strain: Clinical use and future applications-a focused review article. Rev Cardiovasc Med. 23(5):154 (2022).