Research Article - Clinical Practice (2017) Volume 14, Issue 6
The role of corticosteroids in the management of kidney stones disease: a systematic review
- Corresponding Author:
- Ahmed Nouri
Universiti Sains Malaysia, Penang, Pulau Pinang, Malaysia
E-mail: ahmad090@hotmail.com
Abstract
Background: Therapy for kidney stones disease has undergone many changes in the last decades. Medical expulsive therapy such as alpha-blockers and calcium channel blockers regarded as effective agents for stones expulsion and colic pain alleviation. However, many studies have used corticosteroids to utilize their actions in urolithiasis management as well.
Objectives: To determine the role of corticosteroids in the management of urolithiasis in terms of stone expulsion rate and stones expulsion time.
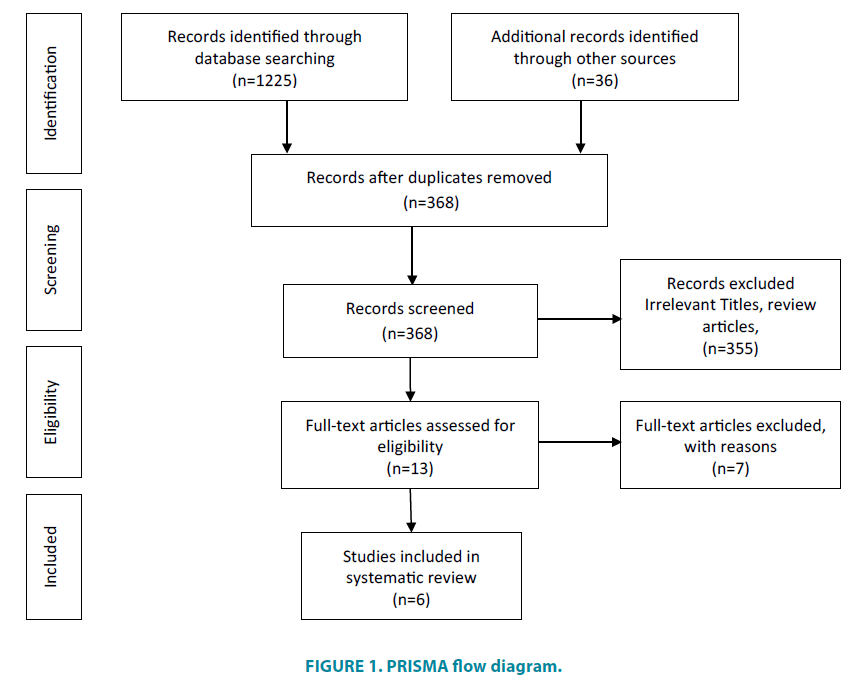
Methods: Following the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement, a literature search using electronic databases including Pub Med, Google Scholar, and Science Direct was undertaken. Full text, prospective, English published studies were included.
Results: Initial search identified 1261 studies. By excluding duplicates, irrelevant titles, and articles that don’t fulfil the inclusion criteria, six articles were included. The included studies were conducted in three countries that was published between 2000 and 2016. All studies examined patients with ureteral stones. The corticosteroids used were (deflazacort, methylprednisolone, and prednisolone); each trial used one of them as monotherapy or in combination with another medical expulsive therapy agent. The retrieved studies achieved their objectives by investigating stone expulsion rates and stone expulsion time mainly.
Conclusions: Corticosteroids can improve the action of medical expulsive drugs when combined with nifedipine or alfa-antagonists for the treatment of ureterolithiasis. In which, reduction of the time for stone passage was statistically significant in most studies while corticosteroids monotherapy was not effective by any means. However, future prospective research studies are required to determine the corticosteroids actual role in the management of urinary tract stones and the worthiness of its combination.
Keywords
urolithiasis; renal colic; corticosteroids; urinary stones; medical expulsive therapy
Introduction
A Kidney stone, or calculi, can be formed by the precipitation of minerals and urinary constituents such as calcium oxalate, calcium phosphate, cystine or uric acid. Urolithiasis is a common problem worldwide with remarkable health and economic burden. It is regarded as a common cause of morbidity and the third most frequent urological disease [1-3].
Renal colic is the acute cramping and intermittent abdominal and flank pain caused by kidney stones. The increased wall tension caused by urinary flow obstruction together with the contraction of ureteral smooth muscle in an attempt to move the stone stimulate the synthesis of prostaglandins. This will cause inflammation, edema formation, and the painful spasms [4-7]. Nonsteroidal anti-inflammatory drugs considered as one of the first line drugs to treat renal colic [8].
Therapy for urolithiasis has undergone many changes. The advent of non-invasive and minimal invasive procedures has revolutionized the surgical approach to kidney stones treatment [9]. However, the mode of treatment is individualized from patient to patient, as it depends on variety of factors such as stone location, stone size, stone physicochemical properties, and patient’s preferences. Using hydration, diuretics, herbals and other non-surgical maneuvers; medical expulsive therapy remains a cornerstones of treatment [10,11].
In patients who have controlled symptoms or newly diagnosed stones, medical expulsive therapy refers to the use of medications to ease the pain of contracting muscles in order to facilitate stone passage during observation period [12,13]. With availability of many agents, alpha-blockers and calcium channel blockers are considered by urologists as effective agents in facilitating stone passage for their actions on decreasing peristaltic activity and colic pain alleviation [4,14-17].
Corticosteroids examined by many studies and often used in combination with drugs used to facilitate stone passage. In which, corticosteroids have been used to treat or prevent the induced mucosal inflammatory reactions that cause edema formation due to stone presence, which will eventually facilitate stones expulsion [18]. Corticosteroids stabilize lysosomes of neutrophils by exerting antiinflammatory and antiedema actions, they also may exhibit their inflammation reduction action by inhibiting prostaglandin release at the site of obstruction [19].
Urolithiasis is one of the most common urological diseases. Almost 20% of stones localized in the ureter, 70% of them are distal ureteral stones that may proceed down for selfpassage [20,21]. Pharmacological therapy of kidney stones disease is still one of the standard management. Many studies showed calcium channel blockers and alpha-blockers efficiency as medical expulsive therapy by reducing expulsion time, increasing rates of expulsion, and reducing colic pain episodes [22,23].
Corticosteroid agents have antiinflammatory and antiedema effects [24] as the presence of stones induces mucosal inflammatory reactions that cause edema, many studies used corticosteroids to treat or prevent these reactions to facilitate stones expulsion. The study aimed to gather and systematically review the evidence of using corticosteroids identify the roles of corticosteroids in urolithiasis management [19].
The aim of this study was to perform a systemic literature review for studies that examined corticosteroids in the management of kidney stones in order to present their role whether in combination with medical expulsive drugs or as monotherapy in terms of stones expulsion rate, renal colic alleviation and the need for an additional analgesia.
The present review’s outcomes of interest are stones expulsion rate, stone expulsion time, renal colic pain status, and the need for an additional analgesic.
Methods and analysis
This systematic review was conducted in accordance with Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA), the results reported following PRISMA as well.
Study Registration
Complying with PRISMA (Preferred Reporting Items for Systematic review and Meta-Analysis) statement, a protocol has been made for this systematic review and registered on PROSPERO, an international database of prospectively registered systematic reviews. The record has been published in the database, under registration number: CRD42017056210.
Search strategy for selecting studies
A literature search within electronic databases including PubMed/Medline, Google Scholar, and Science Direct was conducted. An initial limited search of Medline/PubMed was conducted using medical subject headings such as renal colic, corticosteroids, urolithiasis, medical expulsive therapy and kidney stones. Followed by a thorough search using all keywords stated in the protocol such as kidney stones disease; urinary tract stones, ureteral stones, deflazacort; nephrolithiasis. Eventually, cross checked all bibliography and reference lists of selected paper to select additional studies. Search was limited to English language and unspecified date.
Eligibility criteria
Full text, prospective studies, including randomized controlled trials (RCT) and non- RCTs in which corticosteroids were used as monotherapy or in combination for the management of urinary tract stones, were included. Studies that used corticosteroids without providing analysis related to them were excluded. Retrospective studies, crosssectional, case series, case reports, and reviews were excluded. Moreover, studies that used corticosteroids as adjunctive treatment to procedures were not included.
Participants
The present review included studies investigating the use of corticosteroids in patients with 18 years old or above who complained of renal colic or diagnosed with urinary tract stones by other complaints or as incidental finding, whether as monotherapy or co-administered with medical expulsive therapy. Studies that included pregnant patients or patients using corticosteroids for other indications were not included.
Data extraction
The data which were extracted from included papers using data extraction forms guided by standardized extraction data tool by Cochrane Collaboration; assured to match with the review question and fulfill the review objectives.
Selected studies
An electronic search of all databases identified 1225 studies and 36 studies were found from other sources such as manual search through bibliography and grey literature. By using Zotero V.4.0., duplicates removal lead to 368 studies. By screening of titles, we managed to exclude irrelevant titles, titles that were completely not related to the study objectives, followed by reading abstracts of relevant titles. This resulted in excluding 355 studies, and 13 studies left for full text assessment for eligibility.
Of the 13 eligible studies, seven studies excluded (due to no full article availability, the record was a review article, there was no comparative analysis related to corticosteroids). Final review included six articles as shown in the PRISMA flow diagram (FIGURE 1) [25-27].
Extracted data included: (1) study details: authors, country and year of publication; (2) study objective; (3) sample characteristics: number of participants, (4) methods: design, sampling and duration of study; (5) outcome measures (6) stone type; (7) mean expulsion time; (8) mean expulsion rate (9) medications used, as shown in (TABLE 1).
| Author, Country, Year |
Study Objective | Sample (Duration) |
Outcome | Stone Type | Drug, dose, (no. of patients) |
Mean Expulsion Time | Expulsion Rate |
|---|---|---|---|---|---|---|---|
| Porpiglia
Italy 2000 |
Evaluate the effectiveness of Nifedipine And Deflazacort in the Management of Distal Ureter Stones during Watchful Waiting | 96 patients (28 days) | - Expulsion rate - Expulsion time - Stone size - Analgesic use |
Radiopaque distal ureter stones ≤ 10 mm |
(A) Deflazacort 30 mg (10 d) + Nifidipine 30 mg (28 d) (n=48) |
(A) 7 D (B) 20 D p<0.05 | (A)79% (B) 35% p<0.05 |
| (B) Watchful waiting (n=48) |
|||||||
| Saita
Italy 2004 |
Effect of nifedipine association with prednisolone as expulsive Therapy For ureteral Stones | 50 patients (20 days) | - Expulsion rate - Expulsion time - Analgesic use |
Radiopaque ureteral stones. ≤ 15 mm |
(A) Nifedipine 30 mg (20d) + Prednisolone 25 mg (10 d) (n=25) |
(A) 6 D (B) 10 D | (A) 81% (B) 68% |
| (B) Prednisolone 25 mg (10d) (n=25) |
|||||||
| Dellabella
Italy 2005 |
Assess the clinical efficacy of the addition of a corticosteroid drug to tamsulosin in the medical-expulsive therapy of distal ureterolithiasis | 60 patients (28 days) | - Expulsion rate - Expulsion time - Analgesic use - ER admission - Hospitalization - Quality of life |
distal ureteral stone | (A)Tamsulosin 0.4 mg (n=30) |
(A) 139 ± 113.8 H (B) 103 ± 136.2 H p=0.036 |
(A) 90% (B) 96.7% p=0.612 |
| (B)Deflazacort 30 mg + Tamsulosin 0.4 mg (n=30) |
|||||||
| Porpiglia
Italy 2006 |
Assess the clinical role of corticosteroids in the medical expulsive therapy of symptomatic distal ureteral stones. | 114 patients (10 days) | - Expulsion rate - Analgesic taken - Ureteroscopies - Safety |
Distal ureteral stones ≥ 5 mm |
(A) Tamsulosin 0.4 mg (n=33) |
- | (A) 60% (B) 37.5% (C) 84.5% (D) 33.3% p=0.01 |
| (B) Deflazacort 30 mg QD (n=24) |
|||||||
| (C) Tamsulosin 0.4 mg + Deflazacort 30 mg (n=33)` |
|||||||
| (D) Analgesics (Control) (n=24) |
|||||||
| Hwang Korea 2012 |
Evaluate the efficacy of alfuzosin with methylprednisolone on expulsion and pain control of lower ureteral stones | 113 patients (28 days) | - Expulsion rate - Expulsion time - Stone size - Analgesic used |
Lower ureteral stones ≤ 10 mm |
(A) Alfuzosin 10 mg + Methylprednisolone 8 mg (n=47) |
(A) 7.3 ± 4.87 D (B) 4.4 ± 3.21 D p=0.001 |
(A) 82.9% (B) 62.1% p=0.014 |
| (B) Analgesic only (n=66) |
|||||||
| Shabana
Egypt 2016 |
Compare the safety and efficacy of tamsulosin, alfuzosin, and their combinations with methylprednisolone, in the medical management of lower ureteric stones | 240 Patients (14 days) |
- Expulsion rate - Expulsion time - Side effects |
single lower ureteric stone ≤ 10 mm |
(A) Tamsulosin 0.4 mg (n=53) |
Median (A) 13 D (B) 10 D (C) 12 D (D) 9 D p=0.082 |
(A) 54.7% (B) 71.9% (C) 52.8 (D) 73.6% p=0.042 |
| (B) Tamsulosin 0.4 mg + Methylprednisolone 8mg (n=53) |
|||||||
| (C) Alfuzosin 10 mg (n=53) |
|||||||
| (D) Alfuzosin 10 mg + Methylprednisolone 8mg (n=53) |
Table 1: Antibiotics used for susceptibility testing.
Studies characteristics
The included studies were conducted in 4 countries and were published between 2000 and 2016. None of the selected studies, except the study by Shabana et al., followed the Consolidated Standards of Reporting Trials (CONSORT) statement guideline, which is an evidence based, minimum set of recommendations for reporting randomized trials [28]. None of the selected studies was blinded as well.
Testing techniques used to diagnose kidney stones were stated in all selected studies, where all patients had confirmed diagnosis of ureteral stones. All studies included patients diagnosed with distal ureteral stones, except one of the studies enrolled patients diagnosed with ureteral stones regardless of the exact location. The enrollment period of selected studies ranged from 6 months to 24 months. Demographics of patients were not presented in most of the studies. Kidney-ureter-bladder [KUB] X-ray was done as a weekly follow-up measure. One study had duration of 10 days and only performed KUB before and after treatment [29].
Overall, studies included three types of corticosteroids (Deflazacort, Methylprednisolone, and Prednisolone); each trial used one of them as monotherapy or coadministered with medical expulsive therapy agents. Only three studies compared the intervention groups to a control group and only one study made corticosteroids monotherapy comparison.
All studies allowed the use of analgesic as needed. Non-steroidal anti-inflammatory drugs were the suggested agent except one study allowed for pethidine, in which the control group administered almost double the pethidine administration in intervention group (p=0.021) [8,30].
Expulsion rate and expulsion time were the main endpoints of all studies. Other outcomes, including stone size and number of ureteroscopies, were also investigated [31]. One study used hospitalization and quality of life during treatment as secondary endpoints [32]. Investigating the impact of corticosteroids’ use on analgesic consumption was not an outcome of interest in all selected studies. No correlation was found between stone size and expulsion rate or time in most selected studies [32,33].
All studies considered margin of error as 5%, where p<0.05 was statistically significant, except one study did descriptive analysis only [33]. Student’s t-test, Chi-square test, and other tests were presented. Time to stone expulsion was plotted using a Kaplan–Meier curve and log-rank test in one study. One study only mentioned sample size consideration, in contrast to the rest of studies where no justifications of sample size determination.
After the duration of each study, nonpharmacological approach was used to treat patients if they failed to get rid of stones by selfexpulsion. Ureteroscopy was the most common procedure used to treat most patients.
Porpiglia et al., 2000 performed a prospective randomized controlled trial to evaluate the effectiveness of pharmacological therapy for patients diagnosed with distal ureteral stones left for watchful waiting [34]. The researcher used nifedipine, a calcium channel blockers, based on prior studies, such as Salman et al. and Sahin et al. which concluded that antagonism to calcium inhibits the ureteral contractions and can be used for ureteral colic [35,36]. However, calcium channel blockers as a diverse class of drugs structurally and pharmacologically, it should be noted that only nifedipine has been used in Medical expulsive therapy [37].
Nifedipine was combined with a corticosteroidal agent, deflazacort, for its antiedemic effect. Deflazacort has been shown with minimal side effects and high tolerability [10]. In this study, 96 patients with distal stones were randomly sampled into two groups; one group took oral 30 mg nifedipine slow release per day and oral 30 mg deflazacort per day while the other groups kept for watchful waiting as a control group, only analgesics were provided. Deflazacort was used for 10 days only, while the whole duration of study was 28 days. Expulsion rate in group one was 79% and in group two was 35%, it was statistically significant (p<0.05). Expulsion time ranged from 2 to 10 days in the first group and from 10 to 28 days in the second group (p<0.05). The mean rate of consumption of diclofenac for analgesia per patient in the watchful waiting group was 7 folds the mean rate of consumption of the first group who received combination therapy (p<0.05) [34].
In a study by Porpiglia in 2004, 50 patients diagnosed with radiopaque ureteral stones <15 mm were recruited within 6 months to evaluate the effect of associating nifedipine with corticosteroids. A group received 25 mg oral prednisolone plus 30 mg oral slow release nifedipine per day and the second group received monotherapy of 25 mg oral prednisolone per day. No control group was considered in the study design. Patients were followed for 20 days. Expulsion time of monotherapy group ranged from 5 to 15 days, while that of the combination group ranged from 2 to 10 days. The average size of expulsed stones was almost the same for both groups, 15 mm or below. Monotherapy resulted in 68% expulsion rate, which was less than that of the combination group (81%). Prednisolone monotherapy group required more nonsteroidal anti-inflammatory drugs (NSAIDs) than the other group [33].
A study was conducted by Dellabella et al in 2005 to assess the efficacy of adding corticosteroids in medical expulsion therapy of distal urolithiasis. The recruitment in this study took place in emergency department; recruitment was done to patients diagnosed with distal ureterolithiasis. Included patients were randomized into two groups; each group consisted of 30 patients. One group received 0.4 mg tamsulosin orally, once daily as monotherapy while the other group received 30 mg deflazacort plus 0.4 mg tamsulosin orally, once daily. The expulsion rate between two groups was almost the same (90% vs. 96.7%, p=0.612) and median vials of analgesics used was zero for both groups. No significant differences were found between groups for emergency visits and hospitalizations. The only significance of adding deflazacort was stone expulsion time reduction p=0.036. Median expulsion time for tamsulosin group was 5 days and 3 days for combination group. Moreover, as one of the secondary endpoints, quality of life was assessed by using the EuroQol questionnaire (EQ-5D), a validated questionnaire for quality of life. It was concluded that there was no difference between both groups and corticosteroid addition did not add any extra value to renal colic pain reduction [32].
In a prospective study in 2006, corticosteroid monotherapy was compared with combination alpha blocker and deflazacort. One hundred and fourteen patients were recruited and divided into 4 groups. Group A received tamsulosin 0.4 mg daily only, group B deflazacort 30mg only, group C received both agents, and group D as control group they received only analgesics (intramuscular sodium diclofenac). Patients received medications for 10 days, based on this being the safe period of time to prevent steroids side effects and expulsion of stone was anticipated to occur within this time as demonstrated by literature [14]. The combination of tamsulosin with deflazacort had a high expulsion rate (84.8%), this was statistically significant compared to other groups (p<0.01). By comparing deflazacort monotherapy to tamsulosin monotherapy in terms of expulsion rate, the use of corticosteroids monotherapy had a lower efficacy than alphablocker (37.5% vs. 60%; p>0.05). However, although the use of deflazacort monotherapy had a higher expulsion rate than the control group (37.5% vs. 33%), it was not statistically significant, p>0.05. Regarding consumption of analgesics, deflazacort efficiency in the reduction of analgesic consumption shown when associated with tamsulosin, since the combination group had the lowest average analgesic consumption compared to other groups (p<0.001). The use of deflazacort monotherapy had less effective in reducing analgesic consumption compared to tamsulosin monotherapy [31].
Hwang et al. evaluated the efficacy of combining methylprednisolone and alfuzosin. Between 2005 and 2007, 113 patients with lower ureteral stones <10 mm in size were enrolled in the study, they were divided into two groups; one group received oral 8 mg methylprednisolone plus oral 10 mg alfuzosin daily and a control group received daily analgesics for four weeks only. Expulsion rate and time of stone passage were the endpoints of the study in addition to analgesic use. After 28 days of follow-up, their analysis found that combining alpha-blocker and Methylprednisolone gives better outcomes over the control group. 82.9% of combination group had stone passage compared to 62.1% in control group (p=0.014). Also, mean stone expulsion time was lower in the combination group (4.4 days vs. 7.3 days, p=0.001) [30].
More recently, in 2016, a study by Shabana in Egypt concluded that stone expulsion rate will be higher if combine corticosteroids with alpha-blockers. From 2012 to 2014, 240 patients with distal ureteral stones <10 mm was recruited; patients were randomized into four groups. The groups received oral 0.4 mg Tamsulosin only, oral 0.4 mg Tamsulosin plus 8 mg Methylprednisolone, oral 10 mg Alfuzosin only, and oral 10 mg Alfuzosin plus 8 mg Methylprednisolone. The groups who used Methylprednisolone combined with an alphablocker had a significant higher stone expulsion rate compared to groups used alpha-blocker only (p<0.05). While in terms of stone expulsion time, expulsion time was not significantly different between groups (p=0.082) [38].
Discussion
While six studies are presented, only three compared alpha blockers with corticosteroid to alpha blocker alone. One study by Saita (2004) compared nifedipine/corticosteroid to corticosteroid monotherapy. Hwang et al. (2012) compared alfuzosin/methylprednisolone to analgesics use. Poriglia (2000) compared nifedipine/deflazacort to placebo.
All studies that examined corticosteroids treated distal ureteral stones only, except one study that examined all ureteral stones. Most studies included radiopaque stones only which lead to a gap in knowledge about corticosteroids for non-radiopaque stones like cystine and uric acid stones [39].
All studies intended to investigate the efficacy of expulsion rate as the primary outcome, while none of the studies investigated the role of corticosteroids in reducing episodes of renal colic.
Although the percentage of expulsion rate was high whenever corticosteroids combined with an alpha-blocker or calcium channel blocker, studies failed to conclude a significant difference in comparison of corticosteroids monotherapy over the combination. While all studies showed a significant difference in expulsion time in patients who used combination compared to single alpha-blockers, calcium channel blocker, or control.
Regarding generalizability of the studies, reviewed studies had high exclusion criteria that almost do not resemble the reality of patients. Generally, there was no rationalization for sample sizes included in the studies.
No significant side effects of corticosteroids occurred with patients, this may be attributed to the short duration of receiving corticosteroids [40].
Limitations
The present study, as all studies do, does not lack limitations that systematic reviews could fall into. No attempts were made to contact with authors to collect full papers of eligible abstract that could not be found.
Conclusion
Turk (2014 EAU) in “Guidelines on Urolithiasis” stated “There is no evidence to support the use of corticosteroids as monotherapy in MET”. Additionally, in the 2016 EAU guidelines it stated, “No recommendation for the use of corticosteroids in combination with alpha-blockers in MET can be made” [29].
Hence, to state the actual effect and role of corticosteroids in urolithiasis management; the present review gathered studies which use corticosteroids in the management of urolithiasis and compared between them.
Corticosteroids monotherapy was clinically and statistically non-significant in the management of kidney stones disease by all outcome measures, thus it is not recommended to use corticosteroids as monotherapy. Corticosteroids improve stones expulsion action if they are combined with agents like alpha blockers and calcium channel blockers. The corticosteroids reduction of tone passage time was statistically significant in most studies, which coincides with 2016EAU.
Compliance with ethical standards
Funding
No funds supported the research
Conflicts of interest
No conflict of interest to be declared.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
References
- Fisang C, Anding R, Muller SC, Latz S, Laube N. Urolithiasis-an interdisciplinary diagnostic, therapeutic and secondary preventive challenge. Dtsch. Arztebl. Int. 112(6), 83-91 (2015).
- Turk C, Petrik A, Sarica K, et al. EAU Guidelines on Diagnosis and Conservative Management of Urolithiasis. Eur. Urol. 69(3), 468-474 (2016).
- Bartoletti R, Cai T, Mondaini N, et al. Epidemiology and risk factors in urolithiasis. Urologia Internationalis. 79(Suppl. 1), 3-7 (2007).
- Golzari SE, Soleimanpour H, Rahmani F, et al. Therapeutic approaches for renal colic in the emergency department: a review article. Anesth. Pain Med. 4(1), e16222 (2014).
- Beltrami P, Guttilla A, Ruggera L, Bernich P, Zattoni F. Renal colic, where is it headed? An observational study. Arch. Ital. Urol. Androl. 88(1), 7-12 (2016).
- Masarani M, Dinneen M. Ureteric colic: new trends in diagnosis and treatment. Postgrad. Med. J. 83(981), 469-472 (2007).
- Ahmad M, Chaughtai MN, Khan FA. Role of prostaglandin synthesis inhibitors in the passage of ureteric calculus. J. Pak. Med. Assoc. 41(11), 268-270 (1991).
- Holdgate A, Pollock T. Systematic review of the relative efficacy of non-steroidal anti-inflammatory drugs and opioids in the treatment of acute renal colic. BMJ. 328(7453), 1401 (2004).
- Turk C, Petrik A, Sarica K, et al. EAU guidelines on interventional treatment for urolithiasis. Euro. Urol. 69(3), 475-482 (2016).
- Türk C, Knoll T, Petrik A, et al. EAU guidelines on urolithiasis 2014. 2012.
- Moe OW, Pearle MS, Sakhaee K. Pharmacotherapy of urolithiasis: evidence from clinical trials. Kidney Int. 79(4), 385-392 (2011).
- Giannarini G, Autorino R. Recommending medical expulsive therapy for distal ureteric calculi: a step back? Eur. Urol. 56(3), 413-415 (2009).
- Hollingsworth JM, Rogers MAM, Kaufman SR, et al. Medical therapy to facilitate urinary stone passage: a meta-analysis. Lancet. 368(9542), 1171-1179 (2006).
- Dellabella M, Milanese G, Muzzonigro G. Randomized trial of the efficacy of tamsulosin, nifedipine and phloroglucinol in medical expulsive therapy for distal ureteral calculi. J. Urol. 174(1), 167-172 (2005).
- Ferre RM, Wasielewski JN, Strout TD, Perron AD. Tamsulosin for ureteral stones in the emergency department: a randomized, controlled trial. Ann. Emerg. Med. 54(3), 432-439, 9 e1-2 (2009).
- Xu H, Zisman AL, Coe FL, Worcester EM. Kidney stones: an update on current pharmacological management and future directions. Expert. Opin. Pharmacother. 14(4), 435-447 (2013).
- Al-Ansari A, Al-Naimi A, Alobaidy A, et al. Efficacy of tamsulosin in the management of lower ureteral stones: a randomized double-blind placebo-controlled study of 100 patients. Urology. 75(1), 4-7 (2010).
- Swartz SL, Dluhy RG. Corticosteroids: clinical pharmacology and therapeutic use. Drugs. 16(3), 238-255 (1978).
- Yamaguchi K, Minei S, Yamazaki T, Kaya H, Okada K. Characterization of ureteral lesions associated with impacted stones. Int. J. Urol. 6(6), 281-285 (1999).
- Cole R, Fry C, Shuttleworth K. The action of the prostaglandins on isolated human ureteric smooth muscle. BJU I. 61(1), 19-26 (1988).
- Romero V, Akpinar H, Assimos DG. Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev. Urol. 12(2-3), e86 (2010).
- Xu H, Zisman AL, Coe FL, Worcester EM. Kidney stones: an update on current pharmacological management and future directions. Expert Opin. Pharmacother. 14(4), 435-447 (2013).
- Parsons JK, Hergan LA, Sakamoto K, Lakin C. Efficacy of α-blockers for the treatment of ureteral stones. J. Urol. 177(3), 983-987 (2007).
- Coutinho AE, Chapman KE. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol. Cell. Endocrinol. 335(1), 2-13 (2011).
- Porpiglia F, Ghignone G, Fiori C, Fontana D, Scarpa RM. Nifedipine versus tamsulosin for the management of lower ureteral stones. J. Urol. 172(2), 568-571 (2004).
- Cooper JT, Stack GM, Cooper TP. Intensive medical management of ureteral calculi. Urology. 56(4), 575-578 (2000).
- Dellabella M, Milanese G, Muzzonigro G. Efficacy of tamsulosin in the medical management of juxtavesical ureteral stones. J. Urol. 170(6), 2202-2205 (2003).
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 8(1), 18 (2010).
- Türk C, Petřík A, Sarica K, et al. EAU guidelines on diagnosis and conservative management of urolithiasis. Eur. Urol. 69(3), 468-474 (2016).
- Hwang EC, Hwang IS, Yu HS, et al. Effects of alfuzosin with methylprednisolone for spontaneous expulsion and pain control of lower ureteral stone. Urol. Res. 40(5), 605-609 (2012).
- Porpiglia F, Vaccino D, Billia M, et al. Corticosteroids and tamsulosin in the medical expulsive therapy for symptomatic distal ureter stones: single drug or association? Eur. Urol. 50(2), 339-344 (2006).
- Dellabella M, Milanese G, Muzzonigro G. Medical-expulsive therapy for distal ureterolithiasis: randomized prospective study on role of corticosteroids used in combination with tamsulosin—simplified treatment regimen and health-related quality of life. Urology. 66(4), 712-715 (2005).
- Saita A, Bonaccorsi A, Marchese F, Condorelli S, Motta M. Our experience with nifedipine and prednisolone as expulsive therapy for ureteral stones. Urol. Int. 72(Suppl. 1), 43-45 (2004).
- Porpiglia F, Destefanis P, Fiori C, Fontana D. Effectiveness of nifedipine and deflazacort in the management of distal ureter stones. Urology. 56(4), 579-582 (2000).
- Salman S, Castilla C, Vela NR. Action of calcium antagonists on ureteral dynamics. Actas. Urol. Esp. 13(2), 150-152 (1988).
- Sahin A, Erdemli I, Bakkaloglu M, et al. The effect of nifedipine and verapamil on rhythmic contractions of human isolated ureter. Arch. Int. Physiol. Biochim. Biophys. 101(5), 245-247 (1993).
- Scholz H. Pharmacological aspects of calcium channel blockers. Cardiovas. Drugs Therapy. 10, 869-872 (1997).
- Shabana W, Teleb M, Dawod T, et al. Outcome of α-blockers, with or without methylprednisolone combination, in medical expulsive therapy for lower ureteric stones: A prospective randomised study. Arab. J. Urol. 14(1), 7-11 (2016).
- Portis AJ, Sundaram CP. Diagnosis and initial management of kidney stones. Am. Fam. Physic. 63(7), 1329-1340 (2001).
- Schäcke H, Döcke WD, Asadullah K. Mechanisms involved in the side effects of glucocorticoids. Pharmacol Therapeutics. 96(1), 23-43 (2002).