Commentary - Interventional Cardiology (2014) Volume 6, Issue 5
Selective and global strategies for thrombus management in ST-elevated myocardial infarction interventions
- Corresponding Author:
- Sameer Mehta
Lumen Foundation, Miami, FL, USA
Tel: +1 305 860 2843
Fax: +1 305 856 2351
E-mail: sameer.lumenglobal@gmail.com
Abstract
Keywords
mechanical thrombectomy, selective thrombus management, SINCERE database, STEMI
Compulsive management of thrombus in ST-elevated myocardial infarction (STEMI) interventions contributes to improved early and late outcomes by reducing distal embolization and no-reflow and enabling better stent apposition. Although there appears unwavering agreement in the rational for thrombus management, the precise role of thrombectomy devices and techniques remains controversial. Clinical trials have been suggestive but not decisive and the ensuing guidelines remain disconcerted [1,2]. We lean upon our extensive 12-year experience with SINCERE in performing short door-to-balloon (D2B) interventions to clarify the role of thrombectomy and to propose strategies that include situations that lack a complete thrombectomy arsenal.
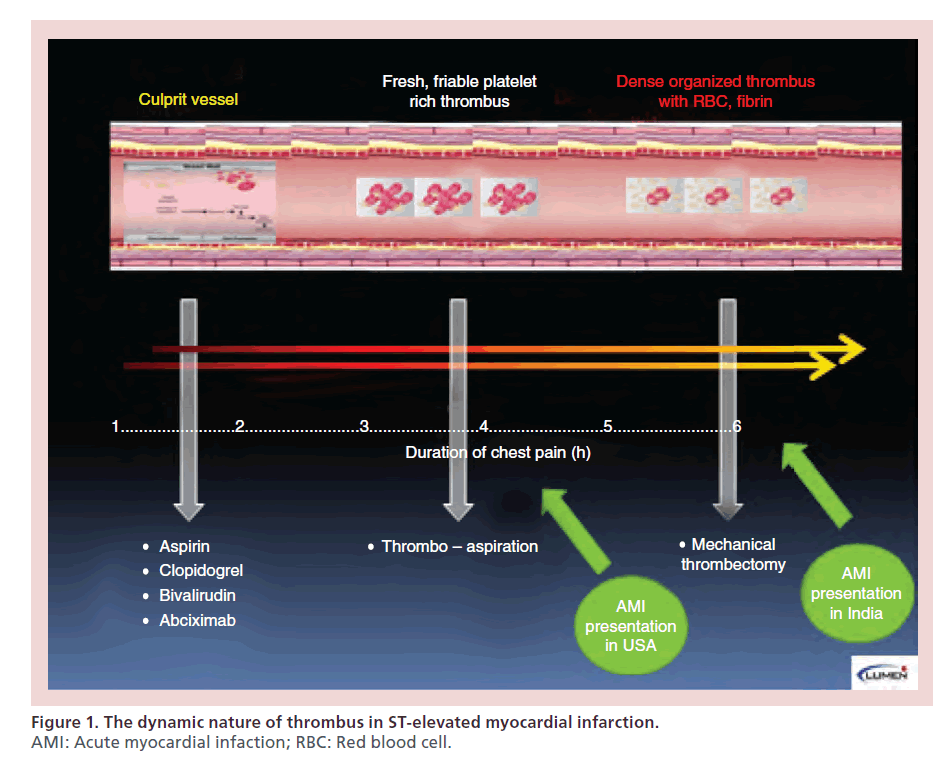
In the early presenting STEMI patient, the thrombus is white, soft, friable and composed primarily of platelets. It is easily extracted by employing simple aspiration catheters [3]. Careful attention of aspirating techniques greatly minimizes distal embolization. Sophisticated STEMI systems (patient advocacy, pre-hospital management, early activation and emergency department bypass) with short D2B times, will often confront such easyto- treat thrombus. White thrombus in a STEMI lesion is easily extracted by aspiration, mechanical thrombectomy devices are often not required and their routine use for treating such lesions increases distal embolization of the soft, friable thrombus. Improvements in the STEMI process and short D2B times therefore directly help the STEMI procedure, as the operators engage the easier-to-treat white thrombus. Unless the fresh thrombus in the early presenting patient is voluminous (myocardial blush grade [MBG] 4 or 5), using the Angiojet in these cases is an overkill and it is associated with higher complications. This observation should explain why several Angiojet trials demonstrated higher major adverse cardiac events [4,5].
Late STEMI presentations, as occurs commonly in developing countries and where STEMI systems are rudimentary, are composed of red thrombus, that is more dense and organized and that is composed of red blood cells and fibrin strands. Management of this thrombus is completely different to that of the soft, friable thrombus. Mechanical thrombectomy devices are of particular benefit in treating such thrombotic lesions provided the anatomy is suitable – large vessels without excessive tortuosity. Although it is not commonly used in this particular situation, laser angioplasty is also an attractive modality for ablating thrombus in these dense, organized, late-presenting lesions. With this essential comprehension of dynamism of thrombus it should also be evident why aspiration thrombectomy is relatively ineffective in treating the organized thrombus. Figure 1 illustrates the dynamic nature of thrombus and the pathophysiological rationale of employing a different strategy to manage white or red thrombus.
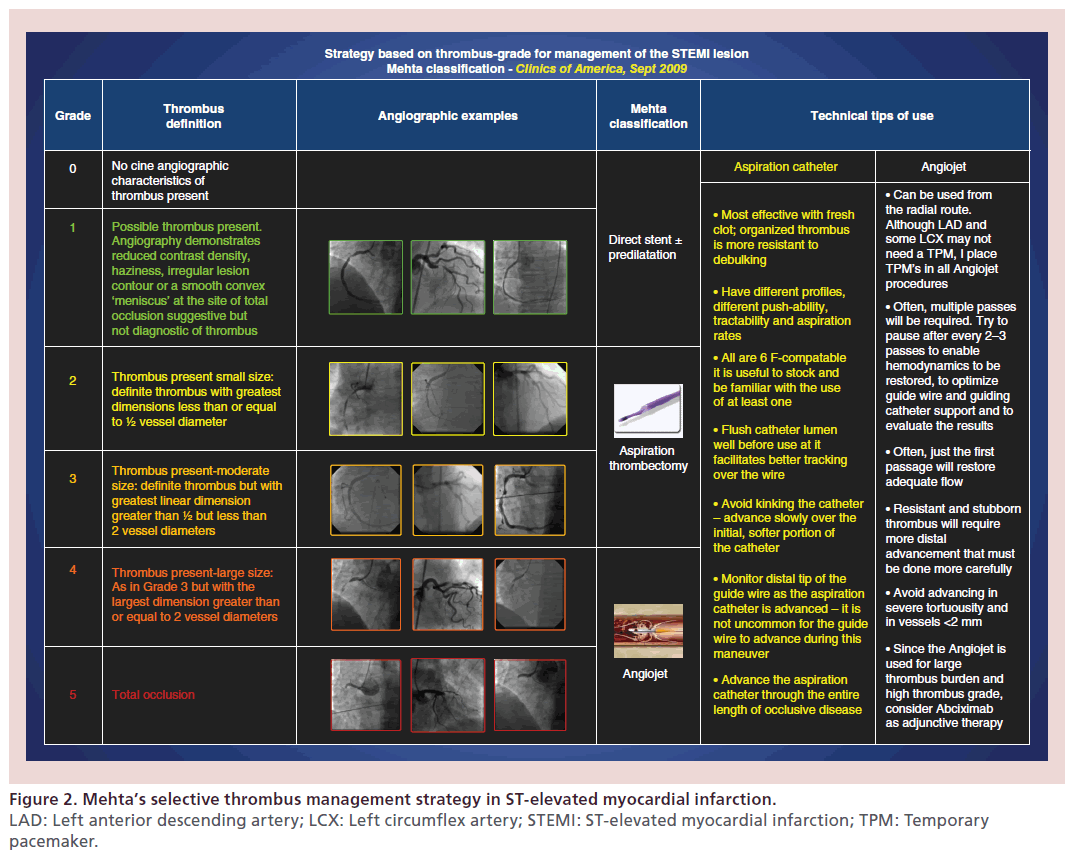
A selective thrombus management strategy is clearly superior to an all-comer strategy that has been advocated in several thrombectomy trials. SINCERE has pioneered and employed a selective strategy for thrombus management in over 1200 consecutive STEMI interventions [6]. With this strategy, low-grade thrombus can be treated with direct stenting, moderate thrombus benefits with aspiration thrombectomy and large-grade thrombus is treated with mechanical thrombectomy. Figure 2 demonstrates this strategy and provides technical tips for using aspiration and mechanical thrombectomy.
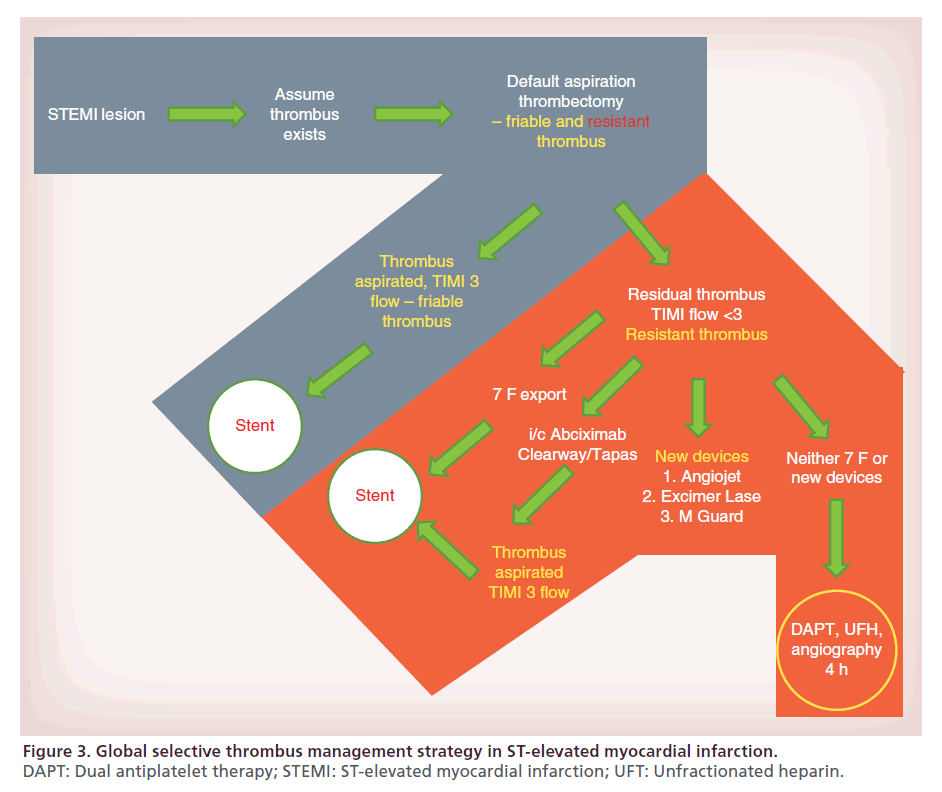
We have further expanded our selective thrombus management strategy to a global environment – as illustrated in Figure 3. This management algorithm mandates a firm conviction that a STEMI lesion contains thrombus. We propose simple aspiration thrombectomy as the initial therapy as it is inexpensive, globally available and extremely easy to use. In addition, as the time course of STEMI is mostly unknown (and difficult to predict), selecting aspiration or mechanical thrombectomy on the basis of duration of chest pain is less certain. One may lean on the electrocardiogram for this approximation, using ST segment elevation as a surrogate for white thrombus and early Q waves with residual ST segment elevation as a proxy for red thrombus [7]. The vast majority of white thrombus will be aspirated with proper aspiration techniques (see Figure 2) – in fact, it has become a norm to make a reverse conclusion – if the thrombus aspirates, the lesion is often, though not always, white thrombus. With restoration of flow in the infarct-related vessel, stenting with either bare metal stent or drug-eluting stent should follow with one major caveat – be mindful that STEMI lesions are often under-sized. We resist balloon expansion at this stage as its use can result in distal embolization of residual thrombus. Its use, that should be rare, is more appropriate to dilate a lesion that does not permit advancement of the aspiration catheter. Post-stenting, intra-coronary vasodilators augment distal microvasculature flow and improve MBG. If aspiration results in incomplete thrombus resolution and/or inadequate improvement in flow (red thrombus, delayed presentation), there are a variety of options that are depicted in Figure 3 and that provide a rationale for a global application of this algorithm.
Our favored strategy, based upon the emphatic comprehension of dynamic thrombus, is mechanical thrombectomy using the Angiojet device. Vessel anatomy must exclude tortuosity and the vessel should be at least 2.5 mm (3.0 or higher is more optimal) and the lesion must have Grade 4 or 5 thrombus. For such suitable lesions, the Angiojet appears an extremely effective device. Some specific tricks of its use are also described in Figure 2. Such lesions are the true niche for Angiojet and we have long advocated a clinical trial to demonstrate the effectiveness for using the Angiojet for treating such lesions rather than its non-selective and haphazard use. Laser angioplasty and emboli protection stent also fall in this group of effective therapies. In particular, M Guard stent may be very useful in such situations [8]. If large randomized clinical trials can demonstrate that it does not increase TVR, this device could become a front line management for treating STEMI lesions. The most common scenario, in particular in late-presenting lesions with dense thrombus, is where these devices are either unavailable or do not work. In such cases that demonstrate residual thrombus and inadequate flow, we strongly recommend not to stent (our best caveat of this manuscript), use ample anti-platelet and anti-coagulants, and return the patient to the catheterization laboratory for a staged and definitive management of thrombus and the STEMI lesion.
Financial & competing interests disclosure
S Mehta is Chief Medical Officer, Asia Pacific, for The Medicines Company. The authors have no other relevant affiliations or financialinvolvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
- O’Gara PT, Kushner FG, Aschreim DD et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J. Am. Coll. Cardiol. 61(4), 78–140 (2013).
- Vecchio S, Varani E, Chechi T et al. Coronary thrombus in patients undergoing primary PCI for STEMI: prognostic significance and management. World J. Cardiol. 6(6), 381–392 (2014).
- Sardella G, Mancone, , Bucciarelli-Ducci C et al. Thrombus aspiration during primary percutaneous coronary intervention improves myocardial reperfusion and reduces infarct size: the EXPIRA (thrombectomy with export catheter in infarct-related artery during primary percutaneous coronary intervention) prospective, randomized trial. J. Am. Coll. Cardiol. 53(4), 309–315 (2009).
- Szerlip M, Grines CL. The current role of AngioJet rheolytic thrombectomy in acute myocardial infarction. J. Invasive Cardiol. 22(10B), 21B–22B (2010).
- Migliorini A, Stabile A, Rodriguez AE et al. Comparison of AngioJet rheolytic thrombectomy before direct infarct artery stenting with direct stenting alone in patients with acute myocardial infarction. The JETSTENT trial. J. Am. Coll. Cardiol. 56(16), 1298–1306 (2010).
- Mehta S, Oliveros E, Ishmael A, Peña C, Dahya Z. Selective strategy for thrombus management in STEMI interventions. J. Invasive Cardiol. 22(10B), 26B–33B (2010).
- Quadros AS, Cambruzzi E, Sebben J et al. Red versus white thrombi in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention: clinical and angiographic outcomes. Am. Heart J. 164(4), 553–560 (2012).
- Stone GW, Abizaid A, Silber S et al. Prospective, randomized, multicenter evaluation of a polyethylene terephthalate micronet mesh-covered stent (MGuard) in STsegment elevation myocardial infarction: the MASTER trial. J. Am. Coll. Cardiol. 60(19), 1975–1984 (2012).