Case Report - Journal of Pharmaceutical Toxicology (2023) Volume 6, Issue 3
Navigating the Complexities of Drug Addiction: Understanding the Path to Recovery
Caroline Roy*
Department of Chemical Engineering, Virginia
- *Corresponding Author:
- Caroline Roy
Department of Chemical Engineering, Virginia
E-mail: roycaroline@rediff.com
Abstract
Drug addiction is a global issue that affects individuals from all walks of life. It is a complex disease that not only impacts the physical health of individuals but also takes a toll on their mental and emotional well-being. In recent years, there has been a growing recognition of the need for comprehensive approaches to tackle drug addiction, focusing not only on treatment but also prevention and harm reduction strategies. This article explores the multifaceted nature of drug addiction and highlights the importance of understanding the path to recovery.
Keywords
Drug addiction • contagious conditions • Liposomal • Lung conditions
Introduction
Drug addiction is not simply a result of weak willpower or moral failing. It is a chronic brain disease that alters the structure and function of the brain, leading to compulsive drug-seeking behaviors. This section delves into the neurological mechanisms behind addiction, shedding light on how drugs hijack the brain’s reward system and impair decision-making processes. While anyone can develop an addiction, certain factors increase an individual’s susceptibility. This section explores the various risk factors associated with drug addiction, including genetic predisposition, environmental influences, early-life experiences, and mental health conditions. Understanding these factors can help identify vulnerable populations and inform targeted prevention efforts[1,2].
Addiction is often stigmatized, leading to discrimination and barriers to treatment. This section discusses the importance of shifting societal perceptions and recognizing addiction as a chronic medical condition. By DE stigmatizing addiction, individuals are more likely to seek help without fear of judgment, facilitating their journey toward recovery. Effective treatment for drug addiction involves a comprehensive approach that addresses the physical, psychological, and social aspects of the disease. This section explores various treatment modalities, ranging from detoxification and medication-assisted therapy to behavioral interventions and support groups. It emphasizes the need for individualized treatment plans tailored to each person’s unique needs. Recovery from drug addiction is a lifelong process that extends beyond achieving sobriety.
Material & Methods
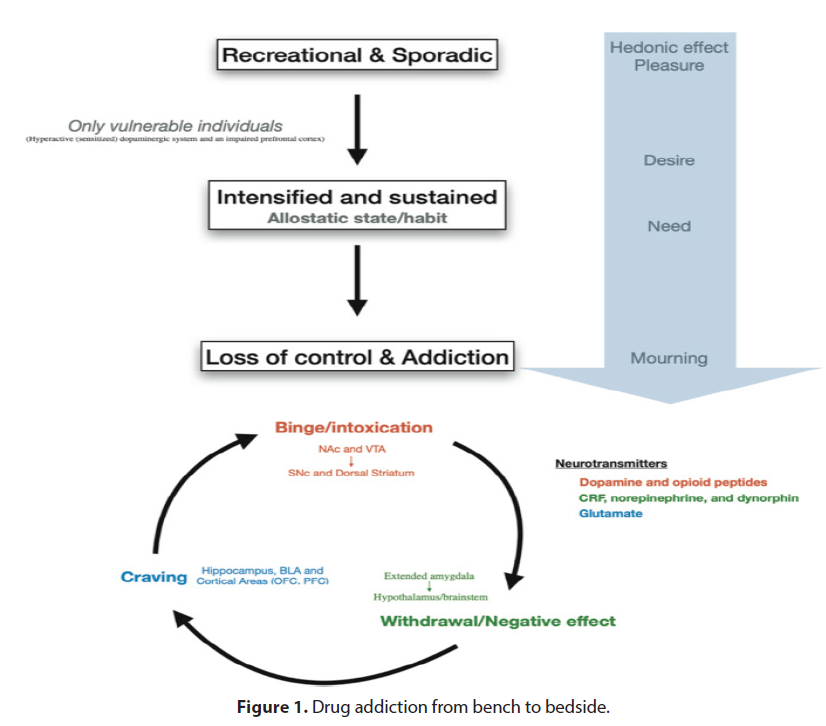
This section highlights the importance of ongoing support, relapse prevention strategies, and aftercare services to help individuals maintain their recovery and rebuild their lives. It also discusses the role of family and community support in fostering lasting positive change. Drug addiction is a complex issue that requires a multifaceted approach involving prevention, treatment, and ongoing support. By understanding the neurological underpinnings of addiction, addressing risk factors, DE stigmatizing the disease, and providing comprehensive treatment and support, we can pave the way for individuals to embark on a path to recovery. With continued efforts and a compassionate approach, we can make strides in combating drug addiction and helping individuals reclaim their lives. In recent years, there has been a growing interest in the therapeutic potential of psychedelic drugs in treating various mental health conditions[3,4]( Figure 1).
While these substances have long been associated with recreational use and counterculture movements, scientific research is now shedding light on their promising role in aiding mental well-being. This article delves into the emerging field of psychedelic-assisted therapy, exploring how these drugs are being utilized in clinical settings and their potential impact on mental health treatment. This section provides a historical overview of psychedelic substances, highlighting their traditional use in indigenous cultures and their subsequent prohibition in the mid-20th century. It then discusses the recent resurgence of interest in psychedelics, fueled by groundbreaking research studies and the shifting perspectives on their therapeutic potential. Here, the article explores the mechanisms through which psychedelic-assisted therapy operates. It explains how substances such as psilocybin (found in magic mushrooms), LSD, and MDMA (commonly known as ecstasy) can affect the brain and induce transformative experiences. The concept of “set and setting” is introduced, emphasizing the importance of a supportive environment and therapeutic integration for optimal outcomes [5,6].
Result
This section delves into specific mental health conditions that are being targeted by psychedelic-assisted therapy. It examines the potential of psychedelics in treating depression, anxiety disorders, post-traumatic stress disorder (PTSD), addiction, and end-of-life anxiety. The article presents key findings from clinical trials and discusses the observed therapeutic effects. As with any novel approach, psychedelic-assisted therapy raises ethical and regulatory questions. This part explores the current legal status of psychedelic drugs and the hurdles researchers and therapists face in conducting clinical trials and implementing these treatments. The article also addresses concerns about safety, patient selection, and the need for professional training and supervision[7,8].
In this final section, the article looks ahead and considers the future of psychedelic-assisted therapy. It explores ongoing research initiatives, potential advancements in drug development, and the integration of these therapies into mainstream mental health care. The article emphasizes the importance of continued research, responsible use, and collaboration between scientific communities, policymakers, and medical professionals. Psychedelic-assisted therapy is emerging as a promising frontier in mental health treatment. While further research and regulatory developments are needed, early findings suggest that these substances hold tremendous potential in alleviating the burden of mental health conditions. By unraveling the therapeutic benefits of psychedelics, we may be on the cusp of a paradigm shift in mental health care, offering new hope for individuals struggling with various psychological disorders[9,10].
Discussion
The world is grappling with a relentless and ever-evolving drug crisis that has far-reaching consequences on individuals, families, and society as a whole. The widespread availability and use of illicit substances have led to devastating social, economic, and health impacts. In this article, we delve into the intricacies of the escalating drug crisis, exploring its causes, effects, and potential solutions. The drug crisis is not a standalone issue but rather a culmination of various underlying factors. This section sheds light on the root causes of drug abuse, including socioeconomic disparities, mental health challenges, peer pressure, and the allure of escape. By examining these factors, we gain a deeper understanding of the complex web that contributes to the drug crisis [11, 12].
Substance abuse poses grave risks to both physical and mental well-being. This segment explores the detrimental effects of drug abuse on individuals, ranging from addiction and overdose to long-term health complications. We examine the impact on vital organs, the prevalence of co-occurring disorders, and the associated healthcare burden on communities. The drug crisis has a profound impact on crime rates and the social fabric of communities. This section delves into the intricate relationship between drugs and crime, discussing the role of drug trafficking, violence, and the strain on law enforcement agencies. We explore the cyclical nature of drug-related crimes and their ripple effects on society[13, 14].
The drug crisis extends beyond national borders, with a vast global drug trade perpetuating its growth. Here, we examine the international dimensions of drug trafficking, discussing the key players, routes, and strategies employed by criminal organizations. Additionally, we delve into existing drug policies, analyzing their efficacy and exploring potential alternative approaches [15].
Confronting the drug crisis requires comprehensive strategies encompassing prevention, treatment, and harm reduction. This segment explores evidence-based approaches such as education programs, access to rehabilitation, and the integration of mental health services. We also highlight the importance of community engagement and destigmatization efforts in fostering long-term change. The drug crisis is an urgent issue demanding attention from policymakers, healthcare providers, and society as a whole. By understanding the complex interplay of factors that contribute to drug abuse, acknowledging the consequences, and implementing effective strategies, we can begin to address this escalating crisis and strive for a healthier, safer future for all.
In recent years, the landscape of drug use has undergone significant transformations, presenting new challenges for policymakers, healthcare professionals, and society as a whole. This article explores the emerging trends in drug use, shedding light on changing patterns, novel substances, and their potential implications for public health and social well-being. The Rise of Synthetic Drugs: Exploring the Dark Web’s Role Synthetic drugs, such as synthetic cannabinoids and designer stimulants, have gained popularity in the underground drug market. The Dark Web has emerged as a major platform for the sale and distribution of these substances. The challenges posed by the accessibility and potency of synthetic drugs require innovative approaches in harm reduction strategies.
Conclusion
The lack of scientific consensus and potential risks associated with long-term micro dosing necessitate further research constantly evolving chemical structures make it difficult for legislation to keep pace. Collaboration between policymakers, law enforcement, and scientific communities is crucial to address the risks associated with NPS. The ever-changing landscape of drug use requires a multifaceted approach to mitigate the potential harms and maximize the benefits. Policymakers, healthcare providers, and researchers must stay vigilant, adapt strategies, and foster interdisciplinary collaborations to address emerging trends in drug use effectively. By understanding these trends, we can develop evidence-based interventions that prioritize public health and promote the wellbeing of individuals and communities.
Acknowledgement
None
Conflict of Interest
None
References
- Kadiyala R, Peter R, Okosieme OE et al. Thyroid dysfunction in patients with diabetes: clinical implications and screening strategies. Int J Clin Pract. 64, 1130-1139 (2010).
- Clark A, Jones LC, de Koning E et al. Decreased insulin secretion in type 2 diabetes: a problem of cellular mass or function. Diabetes. 50, 169-171 (2001).
- DeFronzo RA. Pathogenesis of type 2 diabetes: metabolic and molecular implications for identifying diabetes genes. Diabetes Reviews. 5, 177-269 (1997).
- Peppa M, Betsi G, Dimitriadis G et al. Lipid abnormalities and cardio metabolic risk in patients with overt and subclinical thyroid disease. J Lipids. 9, 575-580 (2011).
- Cettour-Rose P, Theander-Carrillo C, Asensio C et al. Hypothyroidism in rats decreases peripheral glucose utilisation, a defect partially corrected by central leptin infusion. Diabetologia. 48, 624-633 (2005).
- Ogurtsova K, Fernandes JD, Huang Y et al. IDF Diabetes Atlas Global estimates for the prevalence of diabetes. Diabetes Res Clin Pract. 128, 40-50 (2017).
- Zhou Z, Mahdi A, Tratsiakovich Y et al. Erythrocytes From Patients With Type 2 Diabetes Induce Endothelial Dysfunction Via Arginase I. J Am Coll Cardiol. 72, 769-780 (2018).
- Sprague RS, Stephenson AH, EA Bowles et al. Reduced expression of Gi in erythrocytes of humans with type 2 diabetes is associated with impairment of both cAMP generation and ATP release. Diabetes. 55, 3588-3593.
- Blaslov K, Kruljac I, Mirošević G et al. The prognostic value of red blood cell characteristics on diabetic retinopathy development and progression in type 2 diabetes mellitus. Clin Hemorheol Microcirc. 71, 475-481 (2019).
- Venerando B, Fiorilli A, Croci G et al. Acidic and neutral sialidase in the erythrocyte membrane of type 2 diabetic patients. Blood. 99,1064-1070 (2002).
- Kadiyala R, Peter R, Okosieme OE et al. Thyroid dysfunction in patients with diabetes: clinical implications and screening strategies. Int J Clin Pract. 64, 1130-1139 (2010).
- Clark A, Jones LC, de Koning E et al. Decreased insulin secretion in type 2 diabetes: a problem of cellular mass or function. Diabetes. 50, 169-171 (2001).
- DeFronzo RA. Pathogenesis of type 2 diabetes: metabolic and molecular implications for identifying diabetes genes. Diabetes Reviews. 5, 177-269 (1997).
- Peppa M, Betsi G, Dimitriadis G et al. Lipid abnormalities and cardio metabolic risk in patients with overt and subclinical thyroid disease. J Lipids. 9,575-580 (2011).
- Cettour-Rose P, Theander-Carrillo C, Asensio C et al. Hypothyroidism in rats decreases peripheral glucose utilisation, a defect partially corrected by central leptin infusion. Diabetologia. 48,624-633 (2005).
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at