Case Report - Clinical Practice (2021) Volume 18, Issue 8
Migration of fractured tracheostomy tube into bronchus: a case report with literature review
- Corresponding Author:
- Radhi M EL Hafed
ENT department
CHU ibn Rochd Casablanca, Morocco
E-mail: medelhafedradhi@gmail.com
Abstract
Tracheostomy is an opening created in the anterior wall of the trachea inferior to the cricoid cartilage. This procedure is primarily done on patients who have airway obstruction, difficulty with airway clearance, or those who will be intubated for a long period. We share a rare case for migration of fractured tracheostomy tube in the right main bronchus successfully managed in our ENT department of the military hospital of Nouakchott. If the tracheostomy tube is retained for a long time, several late complications can occur, including fracture and dislodgement of the tube. A fractured tracheostomy tube with aspiration is a rare cause of respiratory distress and death, but early diagnosis and the presence of a skillful otolaryngological surgeon can lead to successful management.
Keywords
foreign body, fractured cannula, tracheostomy
Introduction
Tracheostomy is an opening created in the anterior wall of the trachea inferior to the cricoid cartilage. This procedure is primarily done on patients who have airway obstruction, difficulty with airway clearance, or those who will be intubated for a long period [1].
However, it can be associated with serious late complications including tracheostomy stenosis, erosion of the innominate artery, and tracheoesophageal fistulas. Fracturing and hence aspiration of the tracheostomy tube in the tracheobronchial tree is a rare late complication, which can be potentially life-threatening [2].
Hence, there is a need to understand the factors contributing to this complication, prevent its occurrence and recognize and manage it promptly.
Therefore, we share a rare case for migration of fractured tracheostomy tube in the right main bronchus successfully managed in our ENT department of the military hospital of Nouakchott.
Case Presentation
A 54-year old man, with a known case of laryngeal stenosis caused by laryngeal traumatism from 3 years previously, since the patient is tracheotomized. He was admitted to an emergency ward with a principal complaint of respiratory distress. On examination, we found only the outer neck plate and the inner tracheal portion of the tube were missing. The patient reported cough and dyspnea installed after he remove the tracheostomy cannula for cleaning; the cannula was fractured. On examination, we found a low oxygen saturation of 85%, tachypnea (30/minute), and tachycardia (160/ minute), and body temperature of 37.4ºC.
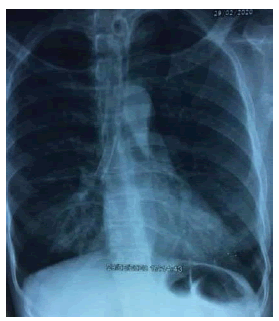
We proceed primarily to an oxygen supply by mask, with saturation at 98%. A chest examination revealed reduced air entry in the right lung; therefore, a chest X-ray was performed immediately. This revealed a foreign body structure, possibly a fractured flange from the inner tracheal tube, in the right main bronchus (FIGURE 1). He was immediately shifted to the operating room for a rigid bronchoscopic removal under general anesthesia.
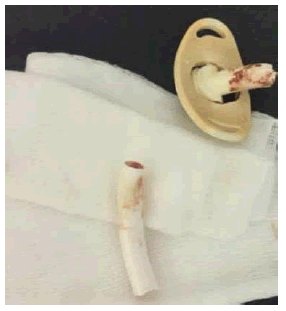
After the bronchoscope was introduced into the tracheal lumen, the foreign body was seen in the right bronchus. It was a fractured curved piece for the inner flange of the tracheostomy tube (polyvinyl chloride tracheostomy) (FIGURE 2). He was removed through the tracheostomy stoma with the aid of foreign body forceps. He was discharged the following day following a complete recovery.
Discussion and Conclusion
Tracheostomy is a life-saving procedure undertaken for various indications including relieving airway obstruction, and laryngeal stenosis. In most cases, it is performed as a temporary measure and is removed once the patient has recovered from the disease process for which it was indicated. But in some cases, as in this case, the tracheostomy tube has to be kept permanently due to the persistence of laryngeal stenosis. If the tracheostomy tube is retained for a long time, several late complications can occur, including fracture and dislodgement of the tube.
Fracturing and hence aspiration of the tracheostomy tube in the tracheobronchial tree are considered a rare late complication of tracheostomy. Bassoe and Boe were the first to report this in the literature in 1960 [3]. This rare complication was also reported with various tracheostomy tube materials such as silver, sterling silver, stainless steel, polyvinyl chloride, and silicone [4]. This situation is more com006D on in children but rarely occurs in adults. Swallowing and cough reflexes are two important mechanisms to prevent this problem.
Unlike children, presentation in adults can range from asymptomatic to pneumonia and may be tolerated as a non-specific respiratory problem, such as chronic cough, hemoptysis, dyspnea, or fever [5,6]. Diagnosis of foreign body aspiration is based on radiography, Computed Tomography (CT) scan, and bronchoscopy [7]. Therapeutic bronchoscopy is the mainstay of the treatment. If it fails, the opinion varies from the second bronchoscopy to thoracotomy.
Any foreign body in the airway poses a risk of obstruction. Tracheostomy tubes usually have a large lumen that enables airflow. However, deaths secondary to acute airway obstruction have been noted in several cases, mostly in the pediatric population-possibly due to the smaller airway caliber [8].
A fractured tracheostomy tube with aspiration is a rare cause of respiratory distress and death, but early diagnosis and the presence of a skillful otolaryngological surgeon can lead to successful management. Moreover, education aimed at increasing awareness about tracheostomy tube care among caregivers and family members is important to reduce the morbidity and mortality associated with the tracheostomy tube.
Acknowledgment
None.
Conflict of Interest
No conflict of interest.
References
- Docherty B. Clinical practice review. Tracheostomy care. Prof Nurse. 16, 1272 (2001).
- St John RE, Malen JF. Contemporary issues in adult tracheostomy management. Crit Care Nurs Clin North Am. 16, 413-430 (2004).
- Bassoe HH, Boe J. Broken tracheotomy tube as a foreign body. Lancet. 1, 1006-1007 (1960).
- Sullivan MJ, Hom DB, Passamani PP, et al. An unusual complication of tracheostomy. Arch Otolaryngol Head Neck Surg. 113, 198-199 (1987).
- Baharloo F, Veyckemans F, Francis C, et al. Tracheobronchial foreign bodies: Presentation and management in children and adults. Chest. 115, 1357-1362 (1999).
- Willett LL, Barney J, Saylors G, et al. An unusual cause of chronic cough. Foreign body aspiration. J Gen Intern Med. 21, C1-C3 (2006).
- Zissin R, Shapiro-Feinberg M, Rozenman J, et al. CT findings of the chest in adults with aspirated foreign bodies. Eur Radiol. 11, 606-611 (2001).
- Lynrah ZA, Goyal S, Goyal A, et al. Fractured tracheostomy tube as foreign body bronchus: our experience with three cases. Int J Pediatr Otorhinolaryngol. 76, 1691-1695 (2012).