Short Communication - Interventional Cardiology (2024) Volume 16, Issue 1
Double outlet both ventricles: An overview
- Corresponding Author:
- Maruti Haranal
Department of Pediatric Cardiac Surgery, U N Mehta Institute of Cardiology and Research, Ahmedabad, India,
E-mail: marusurg@gmail.com
Received date: 15-Jan-2024, Manuscript No. FMIC-24-124330; Editor assigned: 17-Jan-2024, PreQC No. FMIC-24-124330 (PQ); Reviewed date: 31-Jan-2024, QC No. FMIC-24-124330; Revised date: 08-Feb-2024, Manuscript No. FMIC-24-124330 (R); Published date: 16-Feb-2024, DOI: 10.37532/1755-5310.2023.16(1).810
Abstract
Double Outlet Both Ventricles (DOBV) is a rare discordant ventriculo-arterial connection. Although the reported cases are sparse, there is growing awareness of this entity among the clinicians. Recently, DOBV has been included in the International Pediatric Congenital Cardiac code (ICD). Biventricular repair is feasible with appropriate diagnosis and surgical planning.
Keywords
Double outlet both ventricles; Ventriculo-arterial; Biventricular repair; Diagnosis
Introduction
Double Outlet Both Ventricles (DOBV) is an extremely rare discordant ventriculo- arterial connection in which both the arterial trunks are committed to both the ventricles. In these cases the orientation of the interventricular communication is such that both arterial trunks override the muscular ventricular septum. The first description of the DOBV was given by Brandt et al. and also, cases have been recognize at autopsy [1-3]. Only a limited number of cases have been reported in the literature. However, there is growing awareness in the knowledge of DOBV. This article outlines an overview of the lesion.
Embryology
It has been well established that, during normal development the aorta is transferred from the morphological right ventricle to the morphological left ventricle. The observed variation and the extent of transfer dictates the various spectrum of conotruncal anomalies. In Tetralogy of Fallot (TOF), the antero-cephalad location of the outlet septum that anchors the pulmonary root within the right ventricle. In the setting of discordant ventriculo-arterial connections, it is the pulmonary root that is thus transferred, leading to so called Taussig-Bing malformation. In this latter setting, it is the postero-caudal attachment of the outlet septum relative to the interventricular communication that anchors the aortic root within the right ventricle. When the outlet septum is at right angles to the muscular outlet septum, then both arterial roots are free to override the crest of the muscular outlet septum, thus producing the spectrum in which double outlet from both ventricles is the midpoint [4]. The essence of the DOBV is the relationship of the outlet septum to the muscular ventricular septum.
Morphology
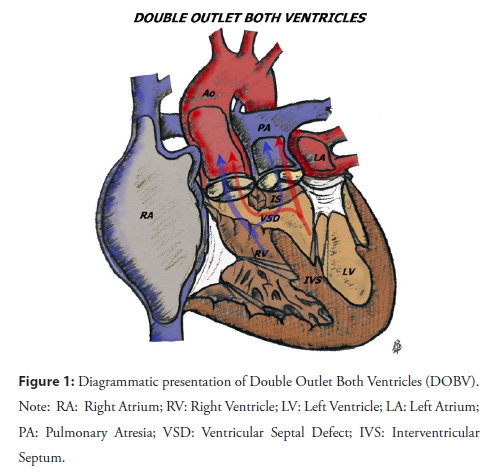
The lesion is characterized by large interventricular communication extending from the tricuspid valve to the farthest extent of the pulmonary valve, subtended inferiorly by the crest of the inter-ventricular septum. The aortic valve lies adjacent to the tricuspid valve and usually separated from the pulmonary valve by the muscular outlet septum. However, the outlet septum may be rudimentary or absent. The great arterial relations can be side-by-side or antero-posterior. DOBV can be associated with any form of atrial arrangements, ventricular morphology and atrioventricular connections. Association of other intracardiac lesions or arch anomalies is known (Figure 1).
Presentation and diagnosis
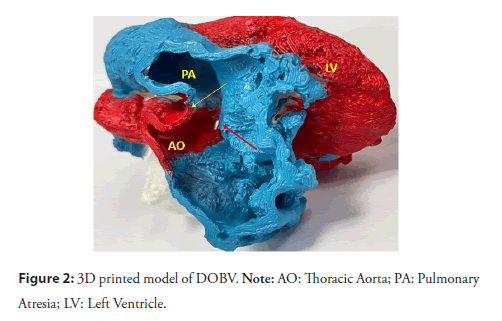
Usual presentation includes failure thrive, respiratory tract infection, feeding difficulty or cyanosis. Chest X ray usually demonstrate cardiomegaly with plethoric lung fields and narrow pedicle. The diagnosis of DOBV can be established using cross sectional 2D Echocardiography. CT angiography can be considered for the diagnosis. 3D printed models are of great value in assessing the anatomy and planning appropriate surgical strategy (Figure 2).
Figure 2: 3D printed model of DOBV. Note: AO: Thoracic Aorta; PA: Pulmonary Atresia; LV: Left Ventricle.
Surgery
In a selected group of patients biventricular repair is feasible. The biventricular repair is accomplished using the “two patch technique” described by Dr Iyer, et al., [5], In majority of the cases repair is performed using hypothermic cardiopulmonary bypass through the trans-atrial approach (right atrium) however, right ventricular approach can be used in difficult cases. Associated lesions are corrected simultaneously. Outflow tracts (right ventricular or left ventricular) obstruction is the potential complication hence, needs careful evaluation intraoperatively. Some cases need right ventricular muscle bundle excision to widen the Right Ventricular Outflow Tract (RVOT).
Follow up
Regular follow up is required to assess the outflow tracts and ventricular function, and atrio-ventricular valves.
Although the literature on the DOBV is sparse, there is increasing awareness of DOBV among the treating physicians. Currently, DOBV has been included in the International Pediatric Congenital Cardiac Code (ICD). K S Iyer, et al., drew the attention of clinicians to this lesion. They have reported their experience with DOBV in 7 patients. Out of which one patient lost for follow up. Among the remaining 6 patients, they used single patch for routing the left ventricle to the aorta in only one patient. With their increasing experience, they realized that “two patch” repair yielded a better outcome by tunneling the ventricles into the respective outflow tracts thus into the great arteries. They used trans-atrial approach for the repair. At midterm follow up (range: 3 months to 8 years) all biventricular function. One patient had mild Left Ventricular Outflow Tract Obstruction (LVOTO).
Katewa, et al., published 6 cases of DOBV with good clinical outcomes. All patients underwent “two patch” repair of the lesion. Trans-ventricular approach was used in one patient and trans-atrial approach in remaining 5 cases. At a mean follow up period of 7 ± 4 months, all patients are keeping well. Although, one patient showed mild LV dysfunction and another had moderate Right Ventricular Outflow Tract Obstruction (RVOTO, Peak gradient-40 mm Hg) but were asymptomatic and are under regular follow up. They also emphasized the importance of 3D printed model in surgical planning [6].
Recently, Genc et al also highlighted the importance of CT- Angiography and 3D printed model in the diagnosis of DOBV [7].
Conclusion
There is growing awareness of DOBV among the treating clinicians. Biventricular repair is feasible with appropriate diagnosis and surgical planning. 3D printed models ease the understanding of the anatomy and helps in surgical planning.
References
- Brandt PWT, Calder AL, Barratt-Boyes BG, et al. Double outlet left ventricle morphology, cineangiocardiographic diagnosis and surgical treatment. Am J Card.38(7):897-909 (1976).
- Aiello VD, Spicer DE, Anderson RH, et al. The independence of the infundibular building blocks in the setting of double outlet right ventricle. Cardiol Young; 27(5):825-836 (2017).
- Ueda M, Becker AF. Classification of hearts with overriding of aortic and pulmonary valves. Int J Cardiol; 9(3):357-369 (1985).
- Hikspoors JPJM, Kruepunga N, Mommen GMC, et al. A pictorial account of the human embryonic heart between 3.5 and 8 weeks of development. Com-mun Biol. 5(1):226 (2022).
- Iyer KS, Garg A, Girotra S, et al. Double outlet of both ventricles: Morphological, echocardiographic and surgical considerations. Eur J Cardiothorac Surg. 59(3):688-696 (2021).
- Katewa A, Haranal M, Madkaiker AN, et al. Experience with surgical correction of double outlet both ventricles. Indian J Thorac Cardiovasc Surg. 39(5):497-500 (2023).
- Genc H, Ozyilmaz I, Baş S, et al. A rare ventriculoarterial connection: Double outlet of both ventricles. Cardiol Young. 33(11):2390-2392 (2023).