Commentary - Interventional Cardiology (2016) Volume 8, Issue 2
Clinical outcome when left atrial posterior wall box isolation is included as a catheter ablation strategy in patients with persistent atrial fibrillation
- Corresponding Author:
- Louisa O’Neill
Department of Cardiology, St Vincent’s
University Hospital, Dublin, Ireland
Tel: 00353879136176
E-mail: louisaoneill@yahoo.co.uk
Submitted: 28 January 2016; Accepted: 01 March 2016; Published online: 04 March 2016
Abstract
Commentary
Despite on-going advances in the field of catheter ablation, the optimum strategy for ablation of persistent atrial fibrillation (AF) remains unclear. While pulmonary vein isolation (PVI) remains the cornerstone of treatment for AF, success rates remain considerably lower in patients with persistent versus paroxysmal AF.
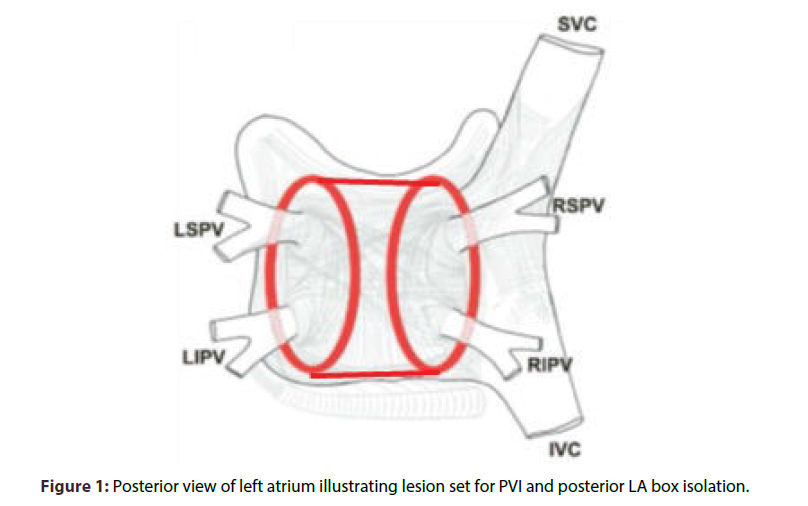
The technique of posterior left atrial wall box isolation has been in increasing use since first described by Kumagai in 2007 [1] however only limited and conflicting data exists with regards to its efficacy. The rationale behind isolation of left atrial wall is based on its common embryonic origin with that of the pulmonary veins and the frequent finding of drivers and rotors in this area (see ‘Supplemental Material’). In our small single centre study [2], we sought to evaluate a strategy of PVI plus posterior left atrial box isolation, consisting of a left atrial (LA) roof line and inferior transverse line in a group of 100 patients whose pattern of AF was predominantly persistent (72%). Isolation of the posterior left atrial wall was achieved in all but one of our patients.
Freedom from recurrent AF on follow-up was achieved in 75%. Obvious limitations include the size of the study and lack of a comparative arm. More specifically the majority of our patients who remained arrhythmia free also underwent additional ablation to sites of high frequency activity elsewhere in the atria based on intraprocedural findings and clinical factors at the discretion of the operator. While this limited our ability to attribute success solely to the box isolation set it did suggest that our ‘real world’ strategy of box isolation combined with more extensive substrate ablation as deemed appropriate may be an effective one particularly when compared to other real world data of PVI alone for patients with persistent AF. In addition there were no adverse outcomes associated with this more extensive procedure. Our findings support the current guidelines that recommend adjuvant substrate modification in addition to pulmonary vein isolation in persistent AF.
The STAR AF 2 trial, which was presented at the ESC by Dr. Verma in 2014 and the results of which were published in the New England Journal of Medicine earlier this year, casts doubt over these guidelines [3]. STAR AF 2 is significant in that it is one of the few recent large scale randomised multi-centre trials comparing ablation strategies in persistent AF (Table 1). Patients were randomly assigned to PVI alone, PVI plus ablation of complex fractionated atrial electrograms (CFAEs) or PVI plus linear ablation of LA roof line and mitral isthmus line. At 18 months rates of the primary outcome of freedom from atrial fibrillation after one procedure were not significantly different between groups. Lower success rates were seen when compared to our study. In addition, procedure and fluoroscopy time was longer for those receiving supplemental ablation although actual rates of adverse events were similar between groups.
| STAR AF 2 Trial Verma et al. |
‘Clinical outcome when left atrial box isolation is included as a catheter ablation strategy in patients with persistent atrial fibrillation’ O’Neill et al. | |
|---|---|---|
| Type of study | Multicentre, randomised controlled trial | Single centre, non-comparative series |
| Patient numbers | 589 | 100 |
| Pattern of AF | Persistent – 100% | Persistent-72% Paroxysmal-28% |
| Lesion set | PVI vs PVI plus mitral isthmus and LA roof line vs PVI plus ablation of CFAEs | PVI plus LA box isolation |
| Follow up monitoring | 12 lead ECG and Holter monitoring at 3, 6, 9, 12 and 18 months. Trans telephonic monitor for duration of follow up |
Holter monitoring at 2, 6 and 12 months |
Table 1: Comparing aspects of STAR AF 2 trial with our single centre study. PVI- pulmonary vein isolation; LA-left atrial; CFAEs-complex fractionated atrial electrograms.
The reason for the lack of benefit in the groups who underwent additional ablation is unclear. It is worth considering that a comprehensive strategy of PVI plus lines and CFAE ablation as performed in the majority of our patients was not evaluated in this trial. Furthermore only 74% of patients who underwent linear ablation in STAR AF achieved complete conduction block across both lines. In addition the lesion set selected did not include posterior box isolation. Our favourable results may be partly explained by less rigorous monitoring on follow up and possible under detection of subclinical AF (see ‘Figure 1’ for further comparison).
In summary the optimum therapeutic ablative strategy in patients with atrial fibrillation remains uncertain. Our small single centre study suggested a benefit from a comprehensive ‘real world’ approach including complete posterior LA box isolation however the STAR AF 2 trial, while neither evaluating such a combination strategy nor including a complete box isolation set, demonstrated no additional benefit for further ablation beyond PVI alone. More work is needed in terms of both evaluating the contribution of the box isolation set in large scale comparative trials and identification of additional non pulmonary vein targets such as rotational activity within the atria which may guide future ablation strategies on a more individualistic basis.
References
- Kumagai K, Muraoka S, Mitsutake C, Takashima H, Nakashima H. A new approach for complete isolation of the posterior left atrium including pulmonary veins for atrial fibrillation. J. Cardiovasc. Electrophysiol. 18, 1047-1052 (2007).
- O'Neill L, Hensey M, Nolan W, Keane D. Clinical outcome when left atrial posterior wall box isolation is included as a catheter ablation strategy in patients with persistent atrial fibrillation. J. Interv. Card. Electrophysiol. 44, 63-70 (2015).
- Verma A, Jiang CY, Betts TR, et al. Approaches to Catheter Ablation for Persistent Atrial Fibrillation. N. Engl. J. Med. 372, 1812-1822 (2015).