Case Report - Interventional Cardiology (2025) Volume 17, Issue 4
Central Shunt as Palliation in a 30-Year-Old with Unrepaired Tetralogy of Fallot and Pulmonary Atresia: A Case Report
- Corresponding Author:
- Aniket Sinha
Department of Cardiology, BM Birla Heart Research Centre, Kolkata, India
E-mail: as303631@gmail.com
Received date: 22-Oct-2025, Manuscript No. FMIC-25-172107; Editor assigned: 24-Oct-2025, PreQC No. FMIC-25-172107 (PQ); Reviewed date: 07-Nov-2025, QC No. FMIC-25-172107; Revised date: 14-Nov-2025, Manuscript No. FMIC-25-172107 (R); Published date: 21-Nov-2025, DOI: 10.37532/1755-5310.2025.17(4).1020
Abstract
Late presentation of complex congenital heart disease is uncommon in adults, particularly in regions with established pediatric cardiac services. We report a case of a 30-year-old male with unrepaired Tetralogy of Fallot (TOF) and Pulmonary Atresia (PA) who presented with severe shortness of breath. Imaging revealed TOF with atresia of the proximal main pulmonary artery and Multiple Aortopulmonary Collateral Arteries (MAPCAs). Given the unfavorable anatomy and prohibitive risk for complete repair, a central aortopulmonary shunt was performed as a palliative measure. Postoperatively, oxygen saturation improved from 65% to 90%, and the patient reported significant symptomatic relief. This case highlights the role of central shunt as a viable palliative option in adult patients with late-presenting complex congenital heart disease where complete repair is not feasible.
Keywords
Tetralogy of fallot; Pulmonary atresia; Central shunt; Adult congenital heart disease; Palliation
Introduction
TOF with PA represents one of the most severe forms of cono-truncal anomalies. Surgical correction is typically performed in childhood, with palliation achieved through systemic-to-pulmonary artery shunts or primary repair, depending on the pulmonary artery morphology. Survival to adulthood without surgical intervention is exceedingly rare, particularly in cases of pulmonary atresia, where pulmonary blood flow depends on patent ductus arteriosus or MAPCAs.
Adults with unrepaired TOF and PA present a unique clinical and surgical challenge. Prolonged cyanosis results in secondary erythrocytosis, coagulopathy, and multiorgan effects, while distorted anatomy and hypertrophied collaterals complicate operative strategies. The primary objective of a central shunt is to ensure adequate pulmonary blood flow, promoting the development and growth of the hypoplastic pulmonary artery bed, alleviating hypoxia and cyanosis, and supporting overall growth [1].
We report the case of a 30-year-old man with unrepaired TOF and PA, in whom a central shunt was chosen as a palliative intervention due to anatomical limitations precluding complete repair.
Case Presentation
A 30-year-old male presented with worsening exertional dyspnea, cyanosis, and reduced exercise tolerance. He reported lifelong bluish discoloration of fingers, clubbing and progressive limitation of activity. He had no prior cardiac interventions.
Clinical findings
On examination, the patient was thin built, with marked central cyanosis and grade IV digital clubbing (Figure 1). Oxygen saturation on room air was 65%. Hemoglobin was elevated to 25.4 g/dL with haematocrit of 74%. Cardiac auscultation revealed a single second heart sound and continuous murmurs along the back, suggestive of MAPCAs.
Investigations
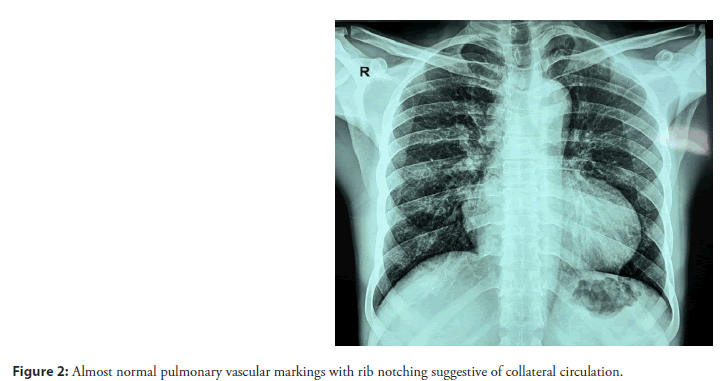
Electrocardiogram demonstrated right ventricular hypertrophy. Chest radiograph revealed almost normal pulmonary vascular markings with rib notching suggestive of established collateral circulation (Figure 2).
Two-dimensional echocardiography showed features of TOF with pulmonary atresia with hypoplastic confluent branch pulmonary arteries (RPA-Small 9mm, LPA-Small 9mm, MPA-11mm) with a large malaligned sub-aortic ventricular septal defect and absent PDA.
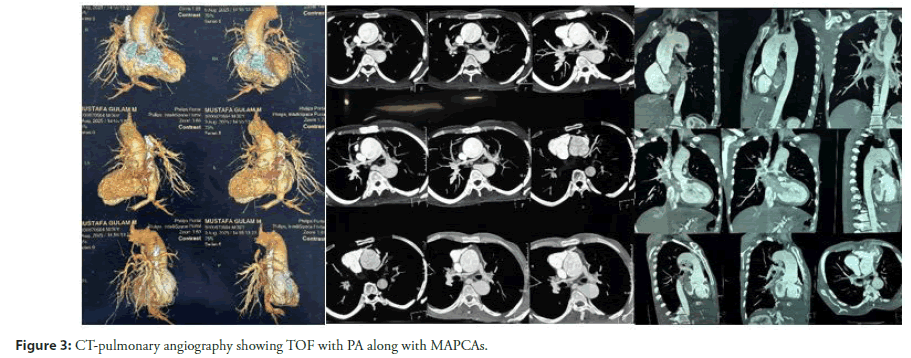
CT pulmonary angiography revealed TOF, Atresia of the proximal main pulmonary artery, thin distal main pulmonary artery and right and left branch pulmonary arteries with confluent branching. Multiple MAPCAs were present. The right ventricle was hypertrophied, and ascending aorta was dilated-43mm (Figure 3).
Figure 3: CT-pulmonary angiography showing TOF with PA along with MAPCAs.
Surgical decision-making
A multidisciplinary heart team reviewed the case. Complete repair was deemed technically unfeasible given severely hypoplastic pulmonary arteries and extensive MAPCAs. The decision was made to perform a central aortopulmonary shunt (ascending aorta to main pulmonary artery) using a prosthetic graft, aiming for symptomatic relief and improved oxygenation.
Operative details
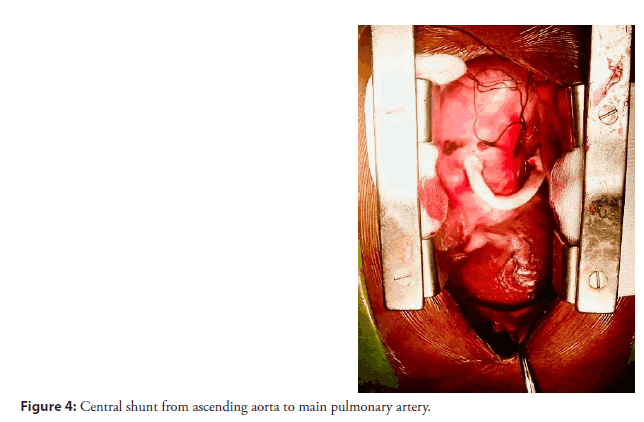
The patient underwent median sternotomy. Extensive collateral circulation was encountered, requiring meticulous dissection and hemostasis. A 6 mm Polytetrafluoroethylene (PTFE) graft was anastomosed between the ascending aorta and the confluence of the right and left pulmonary arteries (Figure 4). Cardiopulmonary bypass was not required. Anomalous origin of the Left anterior descending artery from the Right coronary ostium was noted (Figure 5).
Postoperative course
The patient was extubated within 8 hours. Postoperative oxygen saturation improved to 90%. Minimal inotropes were needed which were gradually weaned off. Heparin infusion was ongoing till day 3 post surgery. Patient was discharged on day 5 post surgery on aspirin prophylaxis. The patient has shown symptomatic improvement and is presently classified as New York Heart Association (NYHA) functional class II.
Discussion
Survival into adulthood with unrepaired TOF and pulmonary atresia is rare, with only isolated case reports in the literature [2,3]. Most patients succumb to hypoxemia or complications of longstanding cyanosis in childhood or early adulthood. Those who survive have well developed MAPCAs that provide pulmonary blood flow [4].
Adult patients with unrepaired TOF and PA pose formidable challenges: Anatomical complexity hypoplastic or absent central pulmonary arteries, extensive MAPCAs, and right ventricular hypertrophy. Physiological consequences longstanding cyanosis results in secondary erythrocytosis, coagulopathy, hyper-viscosity, and multiorgan dysfunction [5]. Surgical risks include fragile collaterals which increase the bleeding risk and pulmonary arteries may be too small for an effective repair.
Role of central shunt
The central aortopulmonary shunt, first described by Waterston and later modified with prosthetic grafts, remains a valuable palliative option in select patients. In adults, it provides several benefits:
• Augments pulmonary blood flow when MAPCAs are insufficient [6].
• Improves systemic oxygen saturation.
• Relieves symptoms and enhances quality of life.
• May serve as a bridge to future staged interventions if pulmonary arteries show growth.
In the present case, complete repair was not feasible due to diminutive pulmonary arteries and unfavorable anatomy for unifocalization. A central shunt offered a safe, technically straightforward, and effective palliative solution.
Learning points
• Adult survival in TOF+PA is extremely rare and usually associated with MAPCAs.
• Preoperative imaging is critical to evaluate pulmonary artery anatomy and collateral circulation.
• Central shunt remains a useful option for palliation in adults where complete repair is not feasible.
Such cases underscore disparities in access to early diagnosis and surgery for congenital heart disease.
Conclusion
This case illustrates that a central aortopulmonary shunt can be a safe and effective palliative strategy in adults with unrepaired TOF and PA when complete repair is not possible. It provides meaningful improvement in oxygenation and functional status, highlighting the importance of individualized surgical planning in late-presenting congenital heart disease.
References
- Sharma S, Kaur B, Baldinger SH. Central aortopulmonary shunt. (2025).
- Ciltea R, Filipoiu F, Bordejevic DA, et al. The case of a 44-year-old survivor of unrepaired tetralogy of fallot, right aortic arch and abdominal aortopulmonary collateral vessels. Medicina (Kaunas). 58(8):1011 (2022).
- Alkashkari W, Alharbi A, Alzahrani H, et al. An adult patient with a tetralogy of fallot case. Cureus. 12(8):e9661 (2020).
- Bull K, Somerville J, Ty E, Spiegelhalter D. Presentation and attrition in complex pulmonary atresia. J Am Coll Cardiol. 25(2):491-499 (1995).
- Eren NK, Dönmez K, Güler A, et al. A late presentation of tetralogy of fallot with pulmonary atresia and coronary-pulmonary artery collateral and a congenital aortic stenosis. Congenit Heart Dis. 3(5):360-363 (2008).
- Duncan BW, Mee RB, Mesia CI, et al. Staged repair of tetralogy of fallot with pulmonary atresia. J Thorac Cardiovasc Surg. 126(3):694-702 (2003).