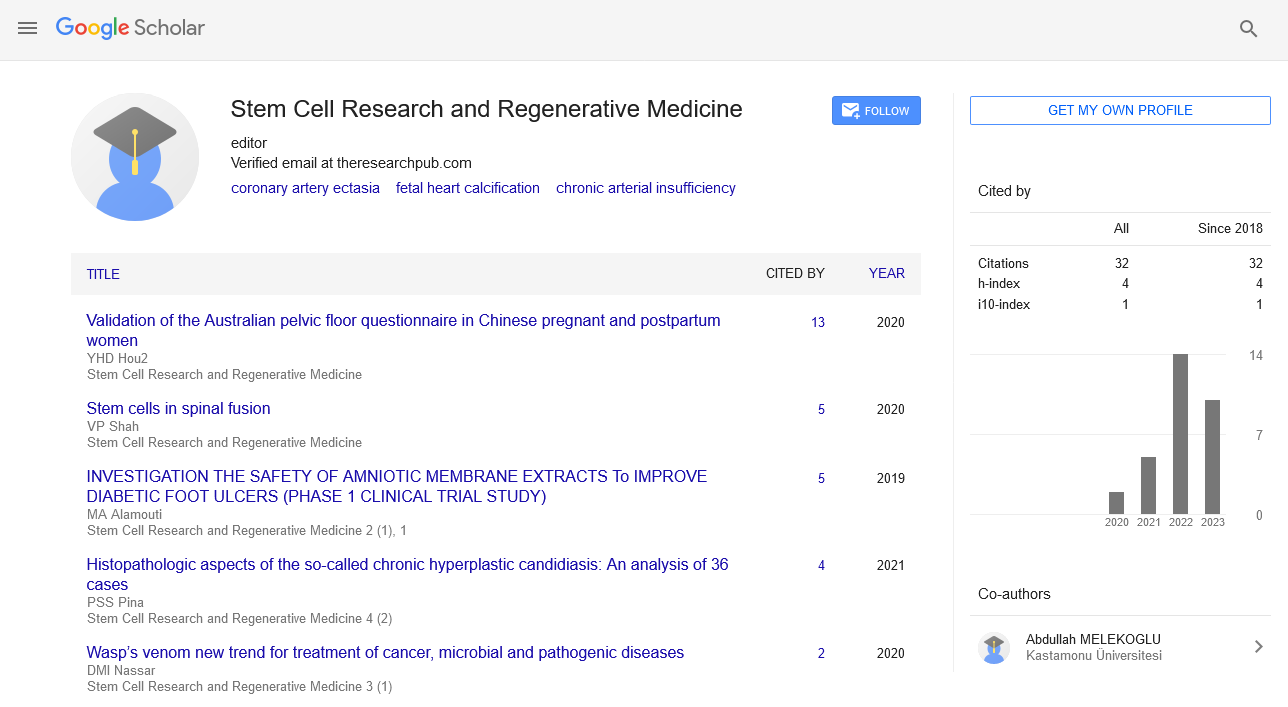
Review Article - Stem Cell Research and Regenerative Medicine (2022) Volume 5, Issue 4
Brain Tumors in Predominating the Macrophages of Stem Cell Mediators
Lingyun Li*
Department of Immunology and Rheumatology, Drum Tower Hospital, Nanjing University Medical School, Nanjing 210008, P. R. China
Department of Immunology and Rheumatology, Drum Tower Hospital, Nanjing University Medical School, Nanjing 210008, P. R. China
a E-mail: Lingyunsli2441@yahoo.com.cn
Received: 01-Aug-2022, Manuscript No. srrm-22-18564; Editor assigned: 03-Aug-2022, PreQC No. srrm-22- 18564 (PQ); Reviewed: 17-Aug-2022, QC No. srrm-22-18564; Revised: 24-Aug-2022, Manuscript No. srrm-22- 18564 (R); Published: 31-Aug-2022, DOI: 10.37532/srrm.2022.5(4).67-68
Abstract
Macrophages originate from blood monocytes that leave the circulation to differentiate in different tissues. There is a substantial heterogeneity among each macrophage population, which most probably reflects the required level of specialisation within the environment of any given tissue. This heterogeneity is reflected in their morphology, the type of pathogens they can recognise, as well as the levels of inflammatory cytokines they produce (i.e. IL-1, IL-6, tumour necrosis factor alpha). In addition, macrophages produce reactive oxygen species, such as nitric oxide, that can kill phagocytosed bacteria.The heterogeneous nature of these cells may not solely be the result of their differentiation process, but it is likely to be inherited from their monocyte precursors.
Keywords
macrophages • BALB/c mice• mesenchymal stem cells (MSCs) • systemic lupus erythematosus (SLE)
Introduction
There is a complex immunologic dysregulation in the background of SLE. It is now well established that T cells play a key role in the regulation of immunologic processes. Much evidence supports the central role of T cells in the pathogenesis and development of SLE. Depletion of T cells was shown to prevent the development of SLE in SLE-prone mice. T helper subsets can be distinguished according to their cytokine secretion capacities and contradictory data about the dominance of Th1 or Th2 cytokines in SLE were presented. On the other hand, some reports thought that autoimmune diseases might be stem cell disorders and found that defects of hematopoietic cells in the diseases. Preliminary reports on cotrans plantation of MSCs and hematopoietic stem cells (HSCs) indicated a significant reduction in acute and chronic graft-versus-host disease (GVHD) and an enhancement of HSCs engraftment [1]. In addition, in vitro culture-expanded autologous MSCs could be infused intravenously without toxicity. It was reported that co- transplantation of MSCs along with HSCs was prior to simple HSCs transplantation in MRL/ lpr mice. These mice manifest clinical and immunological abnormalities, including high levels of antinuclear antibodies, hemolytic anemia, proteinuria, and progressive immune complex glomerulonephritis. In our studies, BALB/c mice were used as control. The lupus- prone NZBWF1 animals are henceforth referred as NW, whereas the control BALB/c strain is indicated as Bc.
Results
MSCs from mouse bone marrow were isolated based on the enhanced adherence to plastic in culture plates. Homogeneous population of fibroblast-like cells with 90 % confluence in NZBWF1 and BALB/c mice were seen at a median of 7 or 10 days after initial plating, respectively. After the first passage, the cells grew exponentially, requiring weekly passages [2]. Morphologically, NW MSCs appeared very similar to normal counterparts. However, in primary and continued culture NW MSCs seemed to be more viable in the same culture conditions. As shown in Figure A2 and B2, isolated colonies of NW MSCs are more typical. We have six NZBWF1 and six BALB/c mice conducted, with each marrow sample yielding similar results.
Discussion
MSCs have shown to be poorly immunogenic and suppress allogeneic or autologous T cell response, which suggested MSCs might be used in therapeutic applications. In this paper, we have examined interactions between mice MSCs and T lymphocytes in order to understand better the mechanisms of MSC-mediated immune modulation. Some researchers have investigated effects of allogeneic bone marrow-derived mesen chymal stem cells on T lymphocytes from BXSB mice [3]. The present study is the first report showing that MSCs from lupus mice interact with T cells from normal mice and are capable of altering the outcome of immune response. The balance of Th1 and Th2 cells among different groups was then detected. We tested the expression of T-bet and GATA- 3 and intercellular cytokines in T cells co- cultured with different MSCs. T-bet and GATA- 3 are two major T helper-specific transcription factors that regulate the expression of Th1 or Th2 cytokine genes and play a crucial role in T-helper cell differentiation [4]. The results imply that lupus MSCs might be defective, but whether these defects are pathogenic to the disease remains to be explored. Normal MSCs made T-subset a shift to Th1, which might lead to an improvement of the illness and may offer one explanation for the clinical outcome observed by other authors. So we hypothesize that MSCs would influence the maturation and diffraction of T cells and hence the Th polarization of an immune response in vivo. Interestingly we also find there are differences in passage-time and proliferation between Bc MSCs and NW MSCs. The latter has higher proliferation and shorter passage-time. This implies NW MSCs may be defective in their function, which is supported by El-Badri who reported that MSCs from lupus murine model had defective structure and function when compared with MSCs from healthy mouse strains [5].
Acknowledgement
None
Conflict of Interest
No conflict of interest
References
- Wofsy D, Seaman W E.Successful treatment ofautoimmunityin NZB/NZW F1 mice withmonoclonal antibodyto L3T4. J Exp Med, 11 161, 378-391 (1985).
- Wofsy D.Administration of monoclonal anti-T cell antibodies retards murinelupusin BXSB mice. J. Immunol, 136, 4554-4560 (1986).
- Funauchi M, Ikoma S, Enomoto H, Horiuchi A et al. Decreased Th1-like and increased Th-2 likecellsin systemiclupuserythematosus. Scand J Rheumatol 27, 219-224 (1998).
- Takahashi S, Fossati L, Iwamoto M, Merino R, Motta R, Kobayakawa T et al.Imbalance towards Th1 predominance is associated with acceleration of lupus-like autoimmunesyndromein MRL mice. J. Clin. Invest 97, 1597-1604 (1996).
- Ikehara S.Autoimmune diseases asstem celldisorders: normalstem celltransplant for their treatment. Int J Mol Med 1, 5-16 (1998).
Indexed at,Google Scholar,Crossref
Indexed at,Google Scholar,Crossref
Indexed at,Google Scholar,Crossref