Research Article - Journal of Interventional Nephrology (2024) Volume 7, Issue 3
Audit of Haemodialysis Vascular Access in a Sub-Saharan Tertiary Hospital
- Corresponding Author:
- Dada Samuel Ayokunle
Department of Medicine,
Nephrology Unit,
Ekiti State University Teaching Hospital,
Ado Ekiti,
Nigeria
E-mail: ayokunle.dada@eksu.edu.ng
Received: 12-Apr-2024, Manuscript No. OAIN-24-132163; Editor assigned: 15-Apr-2024, PreQC No. OAIN-24-132163 (PQ); Reviewed: 29-Apr-2024, QC No. OAIN-24- 132163; Revised: 06-May-2023, Manuscript No. OAIN-24-132163 (R); Published: 15-May-2023, DOI: 10.47532/oain.2024.7(3).256-261
Abstract
Background: Guidelines recommend using Arteriovenous Fistulas (AVFs) as the preferred vascular access route for haemodialysis patients. However, in resource-poor settings, establishment and maintenance of AVFs can be challenging. This research aims to audit the current practices and outcomes of vascular access routes for haemodialysis at a tertiary hospital in sub-Saharan Africa.
Method and materials: This retrospective, descriptive analysis examines vascular access routes for haemodialysis at our dialysis centre over 11 years, utilising data collected from the medical records of patients who received haemodialysis.
Results: Among the 318 patients, males were more prevalent (61.3% vs. 38.7%). The average age was 49.7 years. Femoral catheters were most commonly used compared to other catheters. Catheter use lasted less than a month for two-thirds of patients (66.4%), while 24.8% used them beyond 6 months. Catheter-related infection (49.8%) was the most frequent complication followed by discomfort (25.8%). Discontinuation reasons included clinical improvement (especially in acute kidney injury patients, 52.0%), death (17.3%), transplantation (3.1%), bleeding (2.8%), and recurrent infection (6.0%). Conclusion: The implications of these findings are far-reaching, as suboptimal vascular access can negatively impact patient outcomes, quality of life, and the overall effectiveness of haemodialysis.
Keywords
Haemodialysis ● Catheters ● Vascular access ● Femoral vein ● Outcome
Introduction
Haemodialysis is a life-saving treatment for End-Stage Renal Disease (ESRD) patients. However, in resource-poor settings, particularly in sub-Saharan Africa, access to haemodialysis remains a significant challenge [1-3]. One of the critical factors determining the success and longevity of haemodialysis is establishing a reliable and well-functioning vascular access route. Vascular access serves as the conduit through which blood is removed from the body, circulated through the dialysis machine, and returned to the patient during haemodialysis.
The three main types of vascular access are Arteriovenous Fistulas (AVFs), Arteriovenous Grafts (AVGs), and Central Venous Catheters (CVCs). However, AVFs are considered the gold standard for long-term vascular access due to their lower risk of infection and longer patency rates compared to CVCs and AVGs [4-6].
Guidelines recommend using AVFs as the preferred vascular access route for haemodialysis patients [6,7]. However, in resource-poor settings, the establishment and maintenance of AVFs can be challenging due to various factors, including late presentation, poverty and limited access to skilled surgeons [1,3,8,9]. Consequently, many patients in resource-poor settings rely on CVCs as their primary or sole means of vascular access. While CVCs provide immediate access for haemodialysis, they are associated with higher risks of infection, thrombosis, and central venous stenosis, which can lead to significant morbidity and mortality [10,11].
Materials and Methods
This is a retrospective analysis of vascular access routes for haemodialysis in our dialysis centre. The data was collected from the medical records of patients who received haemodialysis between 2012 and 2023. The nephrologist in our centre did the placement of the access routes except for the AV fistula and graft.
Data extracted include socio-demographic characteristics (age, gender, comorbidities), type of vascular access (arteriovenous fistula, arteriovenous graft, central venous catheter or femoral catheter), indication for insertion (acute kidney injury or end stage kidney disease), duration of vascular access before removal or discontinuation of use and complications. Approval for the use of the data was obtained from the ethical committee of the hospital.
Data analysis
The data was entered into and analysed using IBM SPSS version 25 for Windows (IBM Corp., Armonk, NY). The frequency of use and outcomes of different vascular access types was determined using descriptive analysis and tables and charts were used to present the data.
Results
Among the patients, 318 (94.9%) had complete data and were included in the analysis. Male patients were almost twice as much as female 61.3% versus 38.7%. The age ranges from 16 years to 95 years with a mean age of 49.7 ± 16.5 years. The frequency of the age distribution is shown in Table 1.
| Age group (years) | Frequency (n) | Percentage (%) |
|---|---|---|
| < 30 | 42 | 13.2 |
| 31-40 | 63 | 19.8 |
| 41-50 | 62 | 19.5 |
| 51-60 | 65 | 20.4 |
| 61-70 | 51 | 16 |
| >71 | 35 | 11 |
Table 1. Frequency and age group distribution of patient.
About one-quarter of the patients 65 (20.4%) and only 35(11.0%) were respectively in the age 51-60 and above 70 years category.
The frequency of access route is shown in Table 2 below. The majority (64.2%) used femoral catheters while less than one-third (31.8%) had jugular access route.
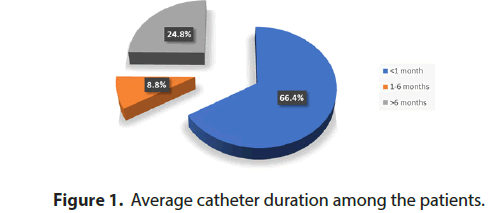
In about two-thirds (66.4%) of the patients, the duration of catheter use is less than one month while 80 (24.8 %) used the permanent catheter beyond 6 months (Figures 1 and 2).
| Access route | Frequency | % |
|---|---|---|
| Jugular catheter* | 101 | 31.8 |
| Femoral | 204 | 64.2 |
| AV fistular | 7 | 2.2 |
| Subclavian | 6 | 1.9 |
Note: *Tunnel and Non-tunnel
Table 2. Frequency of access route among the patient.
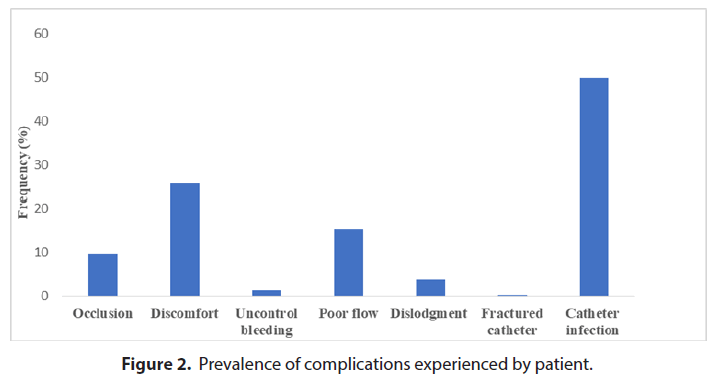
The most common complication is catheterrelated infection in about half of the patients (49.8%) closely followed by reports of discomfort (25.8%). Others include a patient with a fractured catheter.
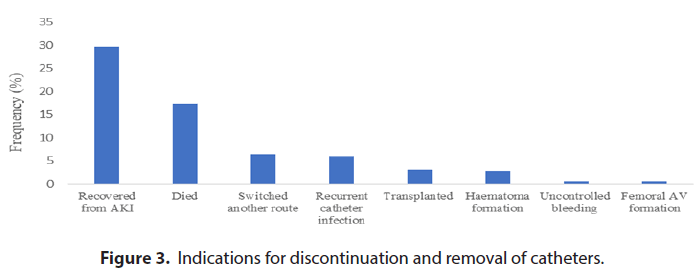
Indications for discontinuation of use of catheters include clinical and laboratory improvement, especially among patients with acute kidney injury (52.0%), died (17.3%), transplanted (3.1%), haematoma formation (2.8%) and recurrent catheter infection (6.0%). This is shown in the Figure 3 below.
Discussion
The findings of this retrospective study, which examined vascular access routes for haemodialysis patients at our tertiary hospital’s dialysis centre between 2012 and 2023 revealed concerning trends that highlight the challenges faced in providing optimal vascular access for haemodialysis patients in resource-limited settings.
The prevalent use of femoral catheters as the primary vascular access route accounts for 61.8% in this study. This is similar to the report of Bahadi et al. where the majority of their patients were placed on a femoral catheter [12]. This is a significant cause for concern because catheterbased access route is generally associated with higher rates of complications. This complication includes catheter infection, occlusion and poor blood flow with the attendant increased morbidity, mortality and healthcare costs [10]. This is in contrast to the report of Hamadneh et al. the majority (77.0%) had AV access and only 23.0% were placed on temporary non-tunnel catheters [13]. Similarly reports from other centres documented various prevalence rates of central venous catheter insertion ranging from 3- 69% [14,15].
The overreliance on catheters in our study population can be attributable to various factors commonly encountered in resource-poor settings, such as poverty, inadequate government health support and prioritization of renal care services, late presentation and limited access to skilled vascular surgeons [9,16].
These barriers can hamper the successful creation and maintenance of Arteriovenous Fistulas (AVFs) and grafts, which are considered the gold standard for long-term vascular access [6,7,15].
In this audit, about one-quarter of the patients complained of catheter discomfort while a significant proportion also developed poor blood flow while on the machine [17,18].
Almost half of our patient cohort (49.8%) had catheter-associated infections. This is comparable to the study by Manuti et al. that evaluated catheter-related bacteraemia in patients with end-stage renal disease on haemodialysis. Nearly two-thirds of their patients had positive culture [19]. A remarkably lower rate of infection was reported by another report that documented incidence of infection as 9.1% and found the risk factors to include length of hospital stay and insertion of the catheter in the left femoral vein [20]. This underscores the risks associated with catheter use in this vulnerable patient population.
In this study, indications for removal of the catheter include clinical recovery in about onethird (29.6%) while a patient developed an aneurysm of the femoral vein and had a switch to another access type. The report of Beigi et al. on placement of long-term haemodialysis catheter (permcath) in patients with endstage renal disease documented two cases of catheter removal following the development of thrombosis and catheter infection respectively [21]. Compared to this study, the complications of haemodialysis catheters which were observed among our patients that require removal or discontinuation include uncontrol bleeding, thrombus formation and catheter fracture [6,22]. Other rare complication includes perforation of the superior vena cava, adhesion, migration, and perforation by the catheter tip [23,24].
Chronic haemodialysis requires durable vascular access that can be utilized over extended periods, spanning months to years. Arteriovenous Fistula (AVF) is regarded as the optimal permanent vascular access [22]. Clinical practice guidelines recommend the use of arteriovenous fistula as the optimal vascular access for haemodialysis due to its overall advantages over other access routes [6]. Conversely, catheters are best reserved for acute dialysis or when there are immediate challenges in establishing permanent vascular access [25].
The regular use of temporary catheters, particularly femoral catheters, among haemodialysis patients remains a major concern for nephrologists in many underdeveloped countries, especially in sub-Saharan Africa [12,26]. This pragmatic approach balances the challenges posed by limited resources with the need to provide essential haemodialysis access in resource-constrained settings as femoral catheters are favoured due to their relatively low cost and ease of placement and replacement. However, these advantages come with significant drawbacks that create concern for the nephrologists. Femoral catheters are associated with a higher risk of infection, blood clots (thrombosis), and malfunction compared to AVFs [27,28]. Additionally, femoral catheters can limit blood flow rates, potentially affecting the effectiveness of haemodialysis and patient well-being [29]. These complications can lead to increased morbidity and mortality and require frequent replacements, ultimately negating potential cost saving [11]. Increasing the burden on both patients and healthcare systems.
Conclusion
The implications of these findings are farreaching, as sub-optimal vascular access can negatively impact patient outcomes, quality of life, and the overall effectiveness of haemodialysis treatment. Addressing the barriers to establishing and maintaining AVFs should be a priority in our setting and similar resource-limited environments. While we advocate for adherence to clinical practice guidelines recommendations on the use of arteriovenous fistula as the optimal vascular access for haemodialysis, collaborative efforts between healthcare providers, policymakers, and stakeholders are necessary to address the systemic barriers. Exploring opportunities for alternative vascular access options beyond central venous catheters, strengthening the training and availability of skilled vascular surgeons and establishing dedicated vascular access teams and multidisciplinary care models are potential strategies to improve vascular access in resourcelimited settings.
References
- Bamgboye EL.The challenges of ESRD care in developing economies: sub-Saharan African opportunities for significant improvement. Clin Nephrol. 86, 18-22 (2016).
[Crossref] [Google Scholar] [PubMed]
- Ashu JT, Mwangi J, Subramani S et al. Challenges to the right to health in sub-Saharan Africa: reflections on inequities in access to dialysis for patients with end-stage kidney failure. Int J Equity Health. 21, 26 (2022).
[Crossref] [Google Scholar] [PubMed]
- Meremo AJ, Ngilangwa DP, Mwashambwa MY et al. Challenges and outcomes of haemodialysis among patients presenting with kidney diseases in Dodoma, Tanzania. BMC Nephrol. 18, 1-6 (2017).
[Crossref] [Google Scholar] [PubMed]
- Lee T. Fistula first initiative: historical impact on vascular access practice patterns and influence on future vascular access care. Cardiovasc Eng Technol. 8, 244-254 (2017).
[Crossref] [Google Scholar] [PubMed]
- Horio M, Aitken EL. Optimising vascular access in incident haemodialysis patients: University of Glasgow; 2017.
- Lok CE, Huber TS, Lee T et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am J Kidney Dis. 75, S1-s164 (2020).
[Crossref] [Google Scholar] [PubMed]
- Sequeira A, Naljayan M, Vachharajani TJ. Vascular Access Guidelines: Summary, Rationale, and Controversies. Tech Vasc Interv Radiol. 20, 2-8 (2017).
[Crossref] [Google Scholar] [PubMed]
- Naicker S, Ashuntantang G. End stage renal disease in sub-Saharan Africa. Chronic Kidney Disease in Disadvantaged Populations: Elsevier; 125-37 (2017).
- Arogundade FA, Barsoum RS. CKD prevention in Sub-Saharan Africa: a call for governmental, nongovernmental, and community support. Am J Kidney Dis. 51, 515-523 (2008).
[Crossref] [Google Scholar] [PubMed]
- Ravani P, Gillespie BW, Quinn RR et al. Temporal risk profile for infectious and noninfectious complications of hemodialysis access. J Am Soc Nephrol. 24, 1668-1677 (2013).
[Crossref] [Google Scholar] [PubMed]
- Patel AR, Patel AR, Singh S et al. Central Line Catheters and Associated Complications: A Review. Cureus. 11, e4717 (2019).
[Crossref] [Google Scholar] [PubMed]
- Bahadi A, El Farouki MR, Zajjari Y et al. Initiating hemodialysis in Morocco: Impact of late referral. Nephrol Ther. 13:525-531 (2017).
[Crossref] [Google Scholar] [PubMed]
- Hamadneh SA, Nueirat SA, Shurrab M et al. Vascular access mortality and hospitalization among hemodialysis patients in Palestine. Saudi J Kidney Dis Transpl. 29, 120-126 (2018).
[Crossref] [Google Scholar] [PubMed]
- Antón-Pérez G, Pérez-Borges P, Alonso-Almán F et al. Vascular accesses in haemodialysis: a challenge to be met. Nefrologia. 32, 103-107 (2012).
[Crossref] [Google Scholar] [PubMed]
- Donca IZ, Wish JB. Systemic Barriers to Optimal Hemodialysis Access. Semin Nephrol. 32, 519-529 (2012).
[Crossref] [Google Scholar] [PubMed]
- Ashuntantang G, Osafo C, Olowu WA et al. Outcomes in adults and children with end-stage kidney disease requiring dialysis in sub-Saharan Africa: a systematic review. Lancet Glob Health. 5, e408-e17 (2017).
[Crossref] [Google Scholar] [PubMed]
- Kukavica N, Resic H, Sahovic V. Comparison of complications and dialysis adequacy between temporary and permanent tunnelled catheter for haemodialysis. Bosn J Basic Med Sci. 9, 265 (2009).
[Crossref] [Google Scholar] [PubMed]
- Huriaux L, Costille P, Quintard H et al. Haemodialysis catheters in the intensive care unit. Anaesth Crit Care Pain Med. 36, 313-319 (2017).
[Crossref] [Google Scholar] [PubMed]
- Manuti JK, Saadoon AM, Lawn AGA et al. Evaluation of Catheter-Related Bacteremia in Patients with End-Stage Renal Disease on Hemodialysis. Arab Board Med J. 24, 101-110 (2023).
- Schwanke AA, Danski MTR, Pontes L et al. Central venous catheter for hemodialysis: incidence of infection and risk factors. Rev Bras Enferm. 71, 1115-1121 (2018).
[Crossref] [Google Scholar] [PubMed]
- Beigi AA, Sharifi A, Gaheri H et al. Placement of long-term hemodialysis catheter (permcath) in patients with end-stage renal disease through external jugular vein. Adv Biomed Res. 3, 252 (2014).
[Crossref] [Google Scholar] [PubMed]
- Bream PR, Jr. Update on Insertion and Complications of Central Venous Catheters for Hemodialysis. Semin Intervent Radiol. 33, 31-38 (2016).
[Crossref] [Google Scholar] [PubMed]
- Li X, Ran F, Guo Y. Perforation of the superior vena cava by a tunnel-cuffed hemodialysis catheter via the right internal jugular vein in an elderly woman. Pak J Med Sci. 39, 619-623 (2023).
[Crossref] [Google Scholar] [PubMed]
- Sequeira A, Sachdeva B, Abreo K. Uncommon complications of long-term hemodialysis catheters: adhesion, migration, and perforation by the catheter tip. Semin Dial. 23, 100-104 (2010).
[Crossref] [Google Scholar] [PubMed]
- Bonfante GM, Gomes IC, Andrade EI et al. Duration of temporary catheter use for hemodialysis: an observational, prospective evaluation of renal units in Brazil. BMC Nephrol. 12, 63 (2011).
[Crossref] [Google Scholar] [PubMed]
- Dada SA, Ajite AB, Ibitoba FA et al. Challenges of haemodialysis: A single centre experience in South West Nigeria. J Clin Nephrol. 3, 055-60 (2019).
- Rafik H, Bahadi A, Aatif T et al. Bacteremia and thrombotic complications of temporary hemodialysis catheters: Experience of a single center in Morocco. Ibnosina J Med Biomed Sci. 9, 159-163 (2017).
- Raina R, Joshi H, Chakraborty R et al. Challenges of long‐term vascular access in pediatric hemodialysis: recommendations for practitioners. Hemodial Int. 25:3-11 (2021).
[Crossref] [Google Scholar] [PubMed]
- Swift O, Vilar E, Farrington K. Haemodialysis. Med. 47, 596-602 (2019).