Case Report - Clinical Practice (2021) Volume 18, Issue 7
A successful treatment of incontinence associated dermatitis (IAD) using combination stomahesive powder and pasta: a case study
- Corresponding Author:
- Suriadi
Postgraduate Nursing Program
Institute of Nursing Muhamadiyah Pontianak, Indonesia
E-mail: suriadif@yahoo.com.au
Abstract
Introduction: Incontinence Associated Dermatitis (IAD), sometimes referred to as perineal dermatitis, is characterized by inflammation and/or erosion of the skin associated with exposure to urine or stool, this case study is presented the successful management of IAD using a combination of stomahesive powder and pasta in-home care setting. Method: This case study describes the management of IAD, an 84-year-old lady who was admitted into a home care setting. She has a history of diseases such as stroke, diabetes, diarrhoea, and Incontinence-associated dermatitis is caused by exposure to stool (diarrhoea). Results: The rapid improvement within the first week was reduced from IAD. After 1 week of using stomahesive powder and paste, the skin condition had improved and by the second week, the skin was not inflamed and no longer excoriated. Within 14 days, the IAD had resolved, and the lesions were healing rapidly with skin normally present. Conclusion: This study presented that a combination of stomahesive powder and pasta was found useful as a treatment for IAD in clinical practice.
Keywords
Incontinence associated dermatitis, stomahesive powder and pasta, diarrhoea
Introduction
IAD is interpreted as skin breakdown related to faecal and/or urinary incontinence [1] and or IAD as erythema and oedema of the skin surface, which may be characterized by bullae with serous exudate, erosion or secondary cutaneous infection [2]. Damage to the epidermis may be present in varying depths and, in some instances, the epidermis may be completely eroded, exposing a moist, weeping dermis [3]. The prevalence of IAD is estimated from 5.2% to 46% [4]. In Asia country was 14.6% and Indonesia was 5.8% [5]. Skin assessments and characteristics should provide guidance and help clinicians when determining the care plan for the prevention and healing of IAD-damaged skin. There are three basic components to the plan of care: cleansing, moisturizing, and protecting the skin [6]. Products needed to achieve this care may comprise these three factors individually or as products that combine two or three components in one product. Products with fewer ingredients (dyes, fragrances, preservatives) may be an option to avoid allergies. Therefore, clinicians must know the composition of the products they use for skincare. Some studies support a single-step intervention (where cleanser, moisturizer, and skin protectants are incorporated into a single product such as a soft washcloth) for efficiency and staff adherence to the skincare regimen [6]. The principle of skincare for applying skin barrier products is to avoid tissue breakdown. Several products on the market can be used. These help to maintain the natural barrier function of the skin and should be applied according to manufacturers’ instructions. A study reported that principal skin protectant ingredients include; Petrolatum (petroleum jelly), Zinc oxide (powder and pasta), Dimethicone (silicon base), Acrylate terpolymer (transparent film) Cyanoacrylate skin bonding polymer [7]. Another study presented that stomahesive powder was an effective treatment for IAD [8]. This study was to evaluate the effectiveness of combination stomahesive powder and pasta for the treatment IAD.
Clinical presentation
■ Clinical history and assessment
An 84-year-old lady was admitted to the hospital with a Urinary Tract Infection (UTI) and she also had a history disease of diabetes mellitus and stroke. She stayed at the hospital from 31 July to 4 September 2020. During hospitalised, she developed urinary incontinence and diarrhoea. Because of the diarrhoea, the patient developed IAD for one month. IAD had been treated with a skin cream, but the ulcer did not heal and she showed pain and discomfort during application and the condition of the skin had deteriorated. A urinary catheter was inserted to manage the urinary incontinence, but the diarrhoea required management with the constant use of incontinence pads. She had been discharged because she was no more infection of UTI. She had been taken care of at home by nurses from the hospital with three shift schedules. The nurses consulted with a Wound Ostomy Continence Nurse (WOCN) specialist to overcome IAD. The patient was found to the presenting IAD grade II and very red skin with lesions to both buttocks (an example of which is shown in FIGURE 1, and her perianal skin was an ulcer, very painful and causing her distress. IAD. She had reduced mobility and the Braden scale score was 14, then the visual analogy scale was the worst pain possible. Her blood pressure was 130/80 mmHg with HbA1c 4.6%. During home care, the patient was given traditional medicine only for the treatment of diarrhoea. The nurses provided total care to the patient because of independence in activities of daily living. The laboratory test results presented still within the normal range (TABLE 1). The written informed consent obtained from the patient included his permission to take photos.
| Home care day | Hb (g/dl) | RBC (× 106/mm3) | WBC (× 103/mm3) | PLT (× 103/mm3) | HCT (%) | ALB (g/dl) | BUN (mg/dl) | Creatinine (mg/dl) | Kalium | Natrium mmol/L |
|---|---|---|---|---|---|---|---|---|---|---|
| mmol/L | ||||||||||
| Day 1 | 10.4 | 3.65 | 4.44 | 219 | 28.7 | 3.1 | 21.7 | 0.73 | 3 | 132 |
| Day 7 | 11.4 | 4.1 | 6.7 | 207 | 33 | 3.2 | 55.9 | 1.09 | 4.5 | 140 |
| Day 14 | 10.6 | 3.81 | 4.43 | 153 | 30.1 | 3.3 | 27.3 | 0.98 | 4.7 | 139 |
| Day 21 | 12.2 | 4.08 | 4.97 | 280 | 35.6 | 3.6 | 26.7 | 0.8 | 4.3 | 140 |
| Note: Hb: Haemoglobin; RBC: Red Blood Cell Count; WBC: White Blood Cell Count; PLT: Platelet; HCT: Hematocrit; ALB: Albumin; BUN: Blood Urea Nitrogen | ||||||||||
TABLE 1. Patient’s laboratory measurements during home care.
■ Management of IAD
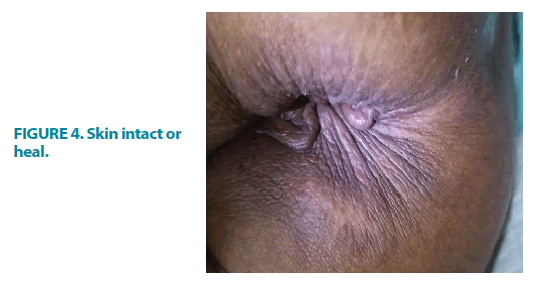
A combination of stomahesive powder and pasta (ConvaTec, USA) were applied as the primary dressing, and an incontinence pad was applied as a secondary dressing (FIGURE 2). The dressing was changed three times a day and even more by the staff nurse according to consultant nurse instruction. IAD lesion was washed with mild soap, warm water, and dried with clean gauze, then apply the stomahesive powder and pasta to both buttocks to repair the skin damage and protect the surrounding skin. The next day, after five and six days of application, the condition of the skin had already improved and the patient’s pain had decreased (3 out of 10 on a VAS scale). While slight redness remained after one week, the patient was no longer reporting pain or discomfort during the application of treatments. Stomahesive powder was continued owing to the positive results and to continue treating the erythema that remained (FIGURE 3). At the 12 days, IAD assessment showed the condition of the skin improved with no ulcer, erythema and irritation (FIGURE 4), the affected skin was now smoother and no longer inflamed, the skin was soft and fully intact, and also the patient did not feel pain with VAS score 0 out of 10. Overall, the IAD showed a good prognosis for healing. The patient’s underlying condition had not changed, but there was an improvement in skin health, and after healing of IAD and pressure ulcer risk had been prevented and she was more comfortable. Then after four weeks, her diarrhoea showed healing.
Discussion
This study was to evaluate the use of Stomahesive powder and pasta as skin protection in patients with IAD on which conventional dressings cannot be applied. The products have been indicated for protecting stomas and peristomal skin from frequent faecal contamination our case study, the patient was treated with combination stomahesive powder and pasta. Despite the patients’ skin being at high risk of damage and high-risk status, there was an improvement in skin condition, in all the conditions observed. The patient showed a reduction in pain and discomfort in the affected skin area. Clinicians commented that the combination of stomahesive powder and pasta was easy to use and apply, with no stickiness or residue. According to preventing and treating the cause of IAD, the principle management of IAD includes assessment, cleansing and treatment [6]. A previous study presented the use of stoma powder as the main skin protective agent to isolate urine and feces and often indifferent IAD [8]. This study was confirmed previous studies on the effectiveness of stomahesive powder and pasta for the treatment of IAD [8,10]. Our study presented that stomahesive powder and paste, which was applied to IAD lesions as a protective agent that protects the skin from frequent faecal and urine discharge, thus providing an opportunity in the repair of damaged skin. Stomahesive powder usually was used for skin irritants and as form a protective barrier against discharge on open areas of peristomal skin. In the future, the effectiveness of Stomahesive powder and pasta may be improved by mixing it with a medication to aid the healing process of skin injury, such as IAD. This study showed that the use of topical products for the treatment of IAD provided skin improvement and pain relief. We postulated that Stomahesive powder and pasta have potential strengths as a skin protectant for the prevention or treatment of IAD.
References
- Beeckman D, Schoonhoven L, Verhaeghe S, et al. Prevention and treatment of incontinence-associated dermatitis: Literature review. J Adv Nurs. 65, 1141-1154 (2009).
- Gray M, Beeckman D, Bliss DZ, et al. Incontinence-associated dermatitis: A comprehensive review and update. J Wound Ostomy Cont Nurs. 39, 61-74 (2012).
- Lee Y-C, Campbell J, Doubrovsky A, et al. A descriptive exploratory survey of incontinence-associated dermatitis in the intensive care setting: The address study. Wound Pract Res. 26, 170-181 (2018).
- Kayser SA, Phipps LA, Vangilder CA, et al. Examining prevalence and risk factors of incontinence-associated dermatitis using the international pressure ulcer prevalence survey. J Wound Ostomy Cont Nurs. 46, 285-290 (2019).
- Ramadhani DW. The influence of empowerment education on preventing the incidence of IAD (Incontinence Associated Dermatitis) in immobility patients at RSUD Arifin Ahmad Pekanbaru, Riau. USU (2020).
- McNichol LL, Ayello EA, Phearman LA, et al. Incontinence-associated dermatitis: State of the science and knowledge translation. Adv Ski Wound Care. 31, 502-513 (2018).
- Ousey K, O’Connor L. IAD. Wounds UK. 13, 1-6 (2017).
- Jian‑Hua D, Xiu‑Li, Li LN, et al. Control effect of structured skin care plan of integrated Chinese and Western medicine in elderly patients with incontinence-associated dermatitis. J Integr Nurs. 3, 6-10 (2021).
- Ohura N, Kurita T, Takushima A, et al. Efficacy of a skin-protection powder for use as a dressing for intractable ulcers. J Wound Care. 15, 471-476 (2006).
- Gray M. Optimal management of incontinence-associated dermatitis in the elderly. Am J Clin Dermatol. 11, 201-210 (2010).