Research Article - Clinical Practice (2017) Volume 14, Issue 4
Treatment of extensive post-burn deformities using extra-large sheets of full thickness skin grafts
- Corresponding Author:
- Mohamed Elsayed
Mohamed
Fellow of Plastic Surgery, Ahmed Maher
Teaching Hospital, Cairo, Egypt
Abstract
Post burn scarring and contractures that affect function remain one of the most frustrating late complications of burn injury. Split thickness skin grafting (STSG) is still the most commonly used method for achieving skin coverage of massive raw areas. In this study, we were able to harvest 14 extra-large sheets of full thickness skin grafts (FTSGs) taken from different areas (back, abdomen and breasts after reduction mammoplasty) to treat extensive post burn contractures and scarring in 10 patients. We could cover raw areas up to 7% Of the TBSA which regained function with less morbidity and more aesthetic results than do STSGs. The results were also satisfactory in 9 patients, yet, only one patient was not satisfied with the result.
Keywords
post-burn deformities, extra-large sheets, full thickness skin grafts
Introduction
Burns may cause large areas of scarring and disfigurement; unfortunately, scarring is the rule because healing in humans does not occur through a process of tissue regeneration [1].
Burn scars dramatically affect patient’s quality of life due to associated psychological problems like anxiety, social avoidance, and depression. Problems in wound-healing may lead to the formation of pathologic scars [1].
Hypertrophic scars (HSc) may occur following trauma, inflammation or due to burns and (possibly HSc) are often associated with contractures of the healing tissues that results in deformities [2].
When a large raw area is needed to be covered, skin grafting by either split-thickness or less commonly full thickness skin grafts is the key. The use of full-thickness skin grafts (FTSGs.) to cover raw areas is limited to relatively smaller recipient areas [3].
Large areas of burned skin may require multiple skin grafting sessions to achieve complete wound coverage, which may lead to significant deformities [4].
In 1984, Feldman described “the single sheet concept” in resurfacing of the face as an aesthetic unit using one large full thickness skin grafts. The grafts were taken from the neck and chest areas. [5]
In 2013, Kim et al., tried to harvest larger FTSGs. He found that the groin area is highly elastic and can provide a relatively large area of skin. The grafts (width and length) ranged from (2-8 cm and 3-13 cm), respectively [6].
Full-thickness skin grafts are ideal for exposed areas of the face that cannot be closed by local flaps. Full-thickness skin grafts are superior to split thickness skin grafts in having more of the characteristics of donor skin; Fullthickness grafts also undergo less contraction while healing [7].
In general, full-thickness grafts contract less than do split-thickness grafts. Contraction can be prevented by splinting or compression devices [8].
Pigmentation of full-thickness skin grafts returns gradually, and these grafts are closer in color to the donor site more predictably than split-thickness skin grafts. It is preferable to protect the grafted areas from exposure to sunlight for at least 6 months post-grafting or longer. Hyper pigmentation can be treated with dermabrasion and laser resurfacing [9].
Patients and methods
Patients
From September 2013 to September 2014, 10 patients including 9 females and one male with extensive post burn deformities were admitted to plastic surgery department, Ahmed Maher teaching hospital. The age of patients ranged from 17 to 41 years. They were treated by aggressive excision of the scarred areas and complete release of contractures together with coverage of the resulting defects with extralarge sheets of FTSGs. 14 sheets (of extralarge FTSGs) were used. Follow up period was 6 months post-operatively for each patient (TABLE 1).
| No | Age | Sex | Type of deformity | Donor sites | Size of ellipse | Areas covered |
Percent Covered (TBSA.)* |
Complications | |
|---|---|---|---|---|---|---|---|---|---|
| Recipient site | Donor site | ||||||||
| 1 | 33 | F | Neck contracture Scarring of both breasts. | Abdomen | 40 × 20 cm | Neck Breasts Both axillae |
7% | Superficial desquamation | ------ ------ ------ |
| Breast reduction 2 sheets |
(30 × 20 cm) (29 × 18 cm) |
||||||||
| 2 | 30 | F | Neck contracture Lower lip ectropion. |
Back (transverse) | 40 × 12 cm | Neck Lower lip |
2% | Superficial desquamation | ------ |
| 3 | 20 | F | Neck contracture. | Back (transverse) | 39 × 12 cm | Neck | 1.5% | ------ | ------ |
| 4 | 17 | F | Scarring of left half of chest Left. breast synechia |
Back (transverse) | 40 × 13 cm | Left Breast Left half of trunk |
6% | Hypertrophic scarring | Partial wound disruption Hypertrophic scarring |
| 5 | 40 | F | Neck contracture Deformity of the chin Bilateral breast adhesions. |
Back (transverse) | 50 × 15 cm | Neck Chin Lower breasts |
3% | ------ | ------ |
| 6 | 23 | M | Neck contracture Deformed lower lip. |
Abdomen (grafted by STSG.) |
25 × 15 cm | Neck Lower lip |
2% | ------ | Hypertrophy of the grafted donor |
| 7 | 22 | F | Neck contracture Lower lip ectropion. Contracted left elbow. |
Back (transverse) | 38 × 12 cm | Neck Lower lip Left elbow |
3% | ------ | ------ |
| 8 | 34 | F | Neck contracture. | Back (transverse) | 30 × 10 cm | Neck | 1.5% | ------ | ------ |
| 9 | 41 | F | Neck contracture Adhesion of both breasts Adhesion of both axillae. | Back (2 oblique sheets) |
50 × 15 cm 30 × 10 cm |
Neck Both breasts Both axillae |
7% | Superficial desquamation | Partial wound disruption hypertrophic scarring -------- -------- |
| Abdomen (one sheet) | 40 × 8 cm | ||||||||
| 10 | 28 | F | Scarring of the whole face. | Abdomen | 30 × 15 cm | lower 2/3 of the face | 2% | Superficial desquamation | ------- |
| Total | 14 sheets | 5/14** | 3/14 | ||||||
*Total body surface area
**4 grafts showed superficial desquamation, while one graft showed loss of about half of the surface area.
Table 1: Patients sheet including the dimensions of the defects, the skin grafts and complications.
Methods
Preoperative
Full history including cause, time of injury and previous operations was taken from each patient. Consent for the use of the skin from the suggested donor areas was also taken.
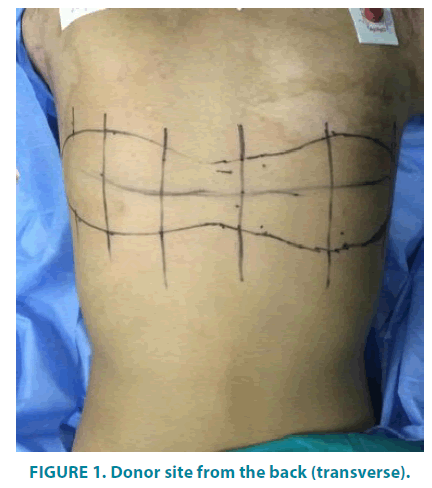
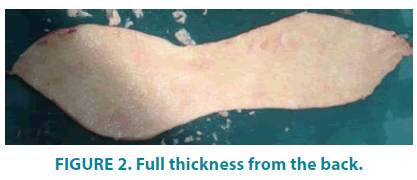
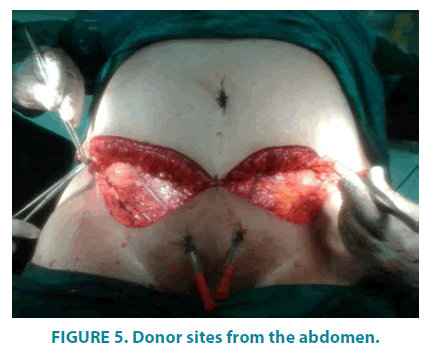
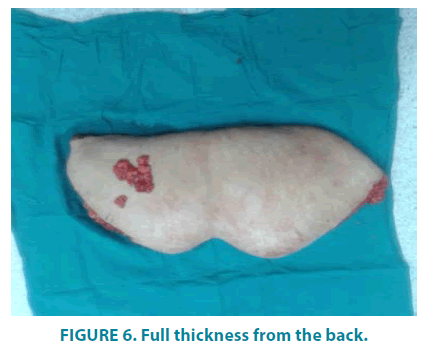
Careful examination of the deformed areas was done regarding scarring, presence or absence of contractures, and if the patient had any grafting operation before. Suggested donor areas (for the full thickness skin grafts) were examined for the skin color, texture and presence or absence of hair. Photographing of the scars, contractures and donor sites was done (FIGURES 1-6).
Operative
All patients were treated by aggressive excision of the scarred areas and complete release of contractures together with coverage of the resulting defects with 14 extra-large sheets of FTSGs. These grafts were taken from the back, the abdomen and Skin gained after breast reduction. All 14 donor sites were closed primarily except for one site was grafted with STSG.
Postoperative management
Patients were dressed in the hospital for the first 3 dressings to look for the take of the grafts. After release of contractures patients were advised to wear different appliances (neck collars, splinting or compression devices).
Follow up of patients
Topical antibiotics creams were used for some patients who had superficial desquamation or wound dehiscence. Patients were examined in the clinic every week for the 1st month, then every two weeks for the 2nd month then monthly for 4 months.
Patients were examined for postoperative complications of the treated areas and donor sites morbidity. Aesthetic results were assessed regarding color of the grafts, Texture of the grafts, and matching with the characters of the recipient areas. Assessment of the function of the reconstructed area and evaluation of the patients’ satisfaction were also done.
Results
During the period of follow up, The 10 patients included in the study were presented as follows:
Size and dimensions of the extralarge sheets
14 extra-large sheets were harvested with the following dimensions:
The length ranged from 25 cm to 50 cm with a mean length of about 36.5 cm while the width ranged from 8 cm to 20 cm with a mean width of about 13.9 cm.
From TABLE 1 areas that could be covered by FTSGs. Ranged from 1.5% up to 7% TBSA.
Donor site morbidity
Only 3 donor sites (2 back wounds closed primarily and one abdominal wound closed with STSG) in 3 patients (about 21% ) showed some problems (the 2 back wounds showed small disruption and hypertrophic scarring, while the abdominal grafted wound showed some hypertrophy in the split thickness graft). Even though, the resulted scarring was minimal and accepted by the 3 patients.
Take of the grafts (recipient sites)
9 and half sheets out of the 14 sheets (68%) showed complete take without any loss.4 sheets showed superficial desquamation (29%) while only one sheet (3%) showed loss of its half surface area.
The aesthetic results
In those who passed the postoperative period without complications (5 patients) showed very good accepted aesthetic results with good color match with the recipient areas.
4 patients had good aesthetic results and one only had poor result.
Function of the reconstructed areas
All patients regained good function of the treated areas, with no recurrence of contractures during the 6 months follow up period.
Patients’ satisfaction
9 patients were satisfied with the aesthetic and functional results of both the donor and recipient sites. Only, one patient was not satisfied with result due to hypertrophic scarring at the reconstructed area.
Postoperative complications of the reconstructed area
5 patients passed the postoperative period smoothly with no abnormal postoperative events (50% of the cases), 4 patients presented with some superficial desquamation of the grafts and all were treated conservatively with creams enhancing healing process (40%) of the cases. 1 patient (10% of the cases) had partial loss of half of the grafts and also was treated conservatively but for a longer period of time. A hypertrophic scarring of half of the reconstructed area occurred.
Discussion
Post burn scarring and contractures are the most common late complications of burns. Split-thickness skin grafting can achieve massive amounts of skin coverage. Still, there are some complications of the use of STSGs. for reconstruction of burn areas, One of the most important complication is contracture of the grafted area or re-contracture of the released one [8]. The second most important complication is poor cosmetic appearance of the reconstructed areas [7].
During our study, Full thickness skin grafting was used as the choice for reconstruction of large extensive post burn deformities. We tried to harvest extra-large sheets of FTSGs. from different donor areas with the least possible affection of the donor areas. We harvested extralarge sheets with length ranged from 25 cm to 50 cm with a mean length of 36.5 cm, while the width ranged from 8 cm to 20 cm with a mean width of 13.9 cm. using these grafts we covered areas up to 7% TBSA.
Out of the 14 sheets 68% showed complete take, 29% showed superficial desquamation, and only 3% showed loss of the graft.
Out of the 14 donor sites we experienced 2 sites of partial wound dehiscence and hypertrophic scarring while the third site showed hypertrophic changes of the STSG covering the raw area with overall 21% donor site morbidity.
Our results were comparable and remarkable to the results of (Somi Kim, 2013) length and width of the grafts he reached [6].
Also, our results were comparable to the results of Krishna et al. in 2008. Their results showed 28 patients with 30 FTSG on the lower limbs, the mean size of the defect was roughly equal to a defect of 6 cm × 4 cm. He classified graft take into good take (>80%) in 18 patients, partial take (50-75%) in 7 patients and poor take (<25%) in 5 patients [13].
During the study, no re-contracture occurred in any of the patients (FIGURE 7A-E). This almost matches with the results of Chandrasegaram and Harvey in 2009 that compared between the use of STSGs. and FTSGs. in pediatric hand burns. They revealed an overall 1 of 45 (2%) incidence of contractures with FTSGs. versus 34 of 126 (27%) with STSGs. Scar release incidence was 15% in the SSG group and 2% in the FTSGs group [10].
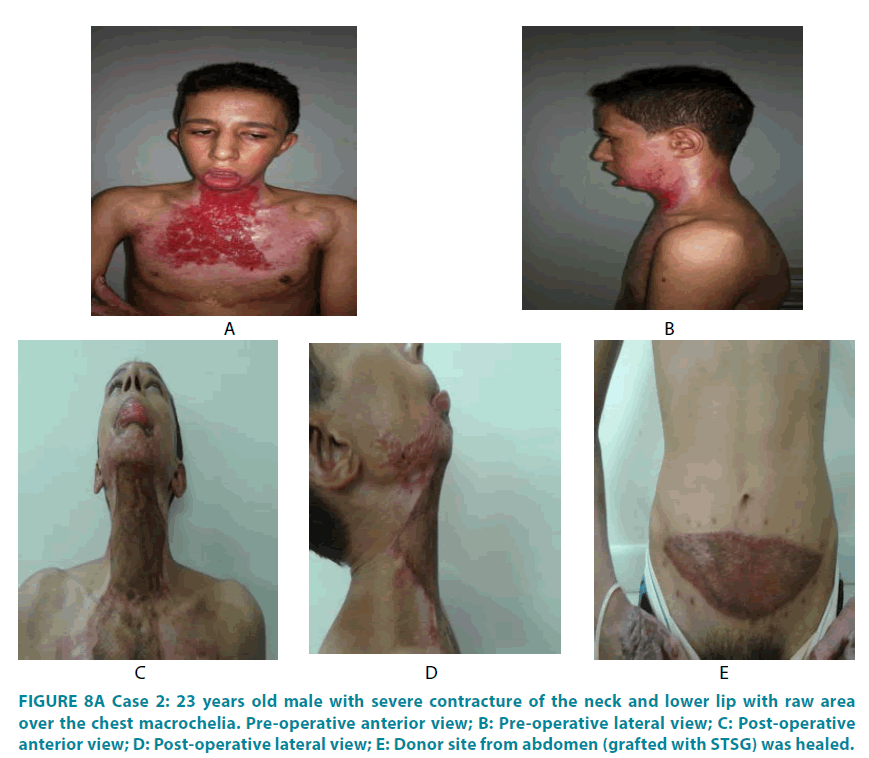
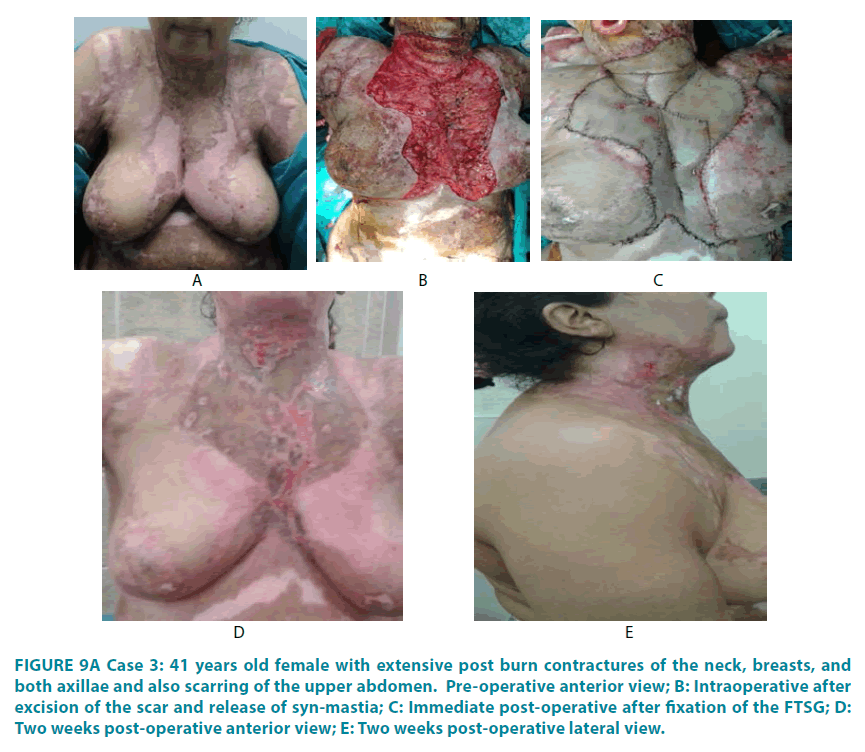
During the study, we found that the use of FTSGs is reliable and they still have more of the characteristics of donor site, like texture, color, and thickness (FIGURE 8A-E). Also, even with harvesting large sheets they can give more accepted cosmetic appearance of the reconstructed areas than do the split thickness grafts in patients who had previous operations with STSGs (FIGURE 9A-E). This agrees with the results of Iwuagwu et al., in 1999. He reviewed 129 patients in 10 years and preferred the use of full-thickness skin grafts to splitthickness skin grafts in post burn contracture release [11].
Figure 8:A Case 2: 23 years old male with severe contracture of the neck and lower lip with raw area over the chest macrochelia. Pre-operative anterior view; B: Pre-operative lateral view; C: Post-operative anterior view; D: Post-operative lateral view; E: Donor site from abdomen (grafted with STSG) was healed.
Figure 9:A Case 3: 41 years old female with extensive post burn contractures of the neck, breasts, and both axillae and also scarring of the upper abdomen. Pre-operative anterior view; B: Intraoperative after excision of the scar and release of syn-mastia; C: Immediate post-operative after fixation of the FTSG; D: Two weeks post-operative anterior view; E: Two weeks post-operative lateral view.
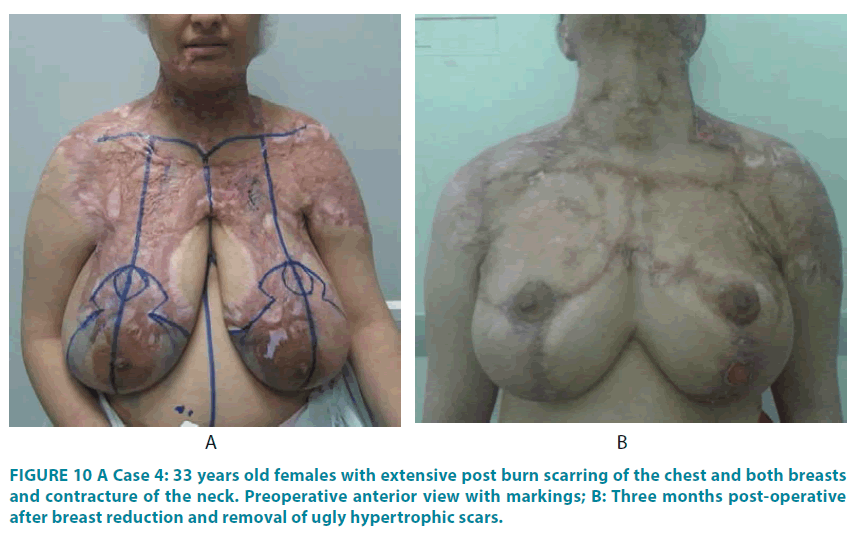
Throughout our study, 90% of patients were satisfied with the results (regarding the color match to the reconstructed area and the minimal donor site affection), while the other 10% (one patient) was unhappy with the early complications and the aesthetic results (FIGURE 10A and B).
This matches with the results of Rathore et al., in August 2014 who reviewed the results of use of full thickness skin grafts in peri-ocular reconstruction and found that (94%) of the cases had good eyelid position and color match, (91%) of the early postoperative cicatricial sequelae can be eliminated by massage, steroid ointment, and silicone gel application. They stated that full thickness skin grafts have excellent graft take and have less donor site morbidity [12].
During the study, we found that FTSGs can be harvested in extra-large sheets with the least affection of the donor areas, and so can provide coverage for very large areas of burns and reconstruct extensive post burn deformities and regain function with less morbidity and more aesthetic and functional outcome.
Declaration of interest
The authors declare no conflict of interest.
Consent
Mohamed Elsayed Mohamed, MD, PhD is fellow of plastic and reconstructive surgery, Ahmed Maher Teaching Hospital, Cairo, Egypt.
Belal A Almubarak, MD, PhD, MRCS is fellow of plastic and reconstructive surgery, Ahmed Maher Teaching Hospital, Cairo, Egypt.
Mohamed I Hassan, MD, PhD is fellow of plastic and reconstructive surgery, Ahmed Maher Teaching Hospital, Cairo, Egypt.
References
- Gangemi EN, Gregori D, Berchialla P, et al. Epidemiology and Risk Factors for Pathologic Scarring After Burn Wounds free. Arch. Facial Plast. Surg. 10(2), 93-102 (2008).
- Tredget EE, Nedelec, B, Scott PG, Ghahary A. Hypertrophic scars, keloids and contractures: The Cellular and Molecular Basis for Therapy. Surg. Clin. North Am. 77(3), 701-30 (1997).
- Branham GH, Thomas JR. Skin grafts. Otolaryngol. Clin. North Am. 23(5), 889-897 (1990).
- Yannas IV, Orgill DP, Burke JF. Template for skin regeneration. Plast. Reconstr. Surg. 127(Suppl. 1), 60S-70S (2011).
- Feldman JJ. Reconstruction of the burned face in children. In Serafin, Georgiade NG, editors: Pediatric Plast. Surg. (1984).
- Kim S, Seung-Won C, In-Ho C. Full thickness skin grafts from the groin: donor site morbidity and graft survival rate from 50 cases. J. Korean Assoc. Oral Maxillofac. Surg. 39(1), 21-26 (2013).
- Robson MC, Krizek TJ. Predicting skin graft survival. J Trauma. 13(3), 213-217 (1973).
- Rudolph R. Inhibition of myofibroblasts by skin grafts. Plast. Reconstr. Surg. 63(4),473-480 (1979).
- Vecchione TR. A technique for obtaining uniform split-thickness skin grafts. Arch Surg. 109 (1974).
- Chandrasegaram MD, Harvey J. Full-thickness vs split-skin grafting in pediatric hand burns-a 10-year review of 174 cases. J. Burn Care Res. 30(5),867-871 (2009).
- Iwuagwu FC, Wilson D, Bailie F. The Use of Skin Grafts in Postburn Contracture Release: A 10-Year Review. Plast. Reconstr. Surg. 103(4), 1198-1204 (1999).
- Rathore DS, Chickadasarahilli S, Crossman R, Mehta P, Ahluwalia HS. Full Thickness Skin Grafts in Periocular Reconstructions: Long-Term Outcomes. Ophthal. Plast. Reconstr. Surg. 30(6), 517-520 (2014).
- Rao K, Tillo O, Dalal M. Full thickness skin graft cover for lower limb defects following excision of cutaneous lesions. Dermatol. Online J. 14(2), 4 (2008).