Case Series - Clinical Investigation (2022) Volume 12, Issue 8
WHO five moments of hand hygiene practice among nurses: A study of tamale teaching hospital, Ghana
- Corresponding Author:
- Abdul Rauf Alhassan
Department of Surgery, Tamale Teaching Hospital, Tamale, Ghana
E-mail: alhassana84@yahoo.com
Received: 9-August-2022, Manuscript No. FMCI-22-71559; Editor assigned: 11-August-2022, PreQC No. FMCI-22-71559 (PQ); Reviewed: 22-August-2022, QC No. FMCI-22-71559 (Q); Revised: 23- August-2022, Manuscript No. FMCI-22-71559 (R); Published: 30-August-2022; DOI: 10.37532/2041-6792.2022.12(8).156-162.
Abstract
The main aim of this study was to assess WHO's five moments of hand hygiene practice among nurses at the surgical department of Tamale Teaching Hospital. This study was conducted using a descriptive cross-sectional survey. Data entry and analysis were done using Statistical Package for the Social Sciences version 20. Frequencies and percentages were used for descriptive analysis and chi-square analysis was done for association and predictors were identified with multiple regression models. A total of 118 questionnaires were administered of which 107 were satisfactorily filled and returned. The mean age of the respondents was 32.21 ± 6.48 with minimum and maximum ages of 21 and 58 respectively. The mean years of occupational and departmental experience were 6.48 ± 5.39 and 3.16 ± 3.15 respectively. The majority (82.2%) of the respondents had good knowledge concerning nosocomial infection prevention. Only 10.3% of the respondents indicated IPC materials or services were always available to them. About 64.5% of the respondents practiced good hand hygiene and factors associated with hand hygiene were: were age group of respondents X2 (2,107)=0.201, p=0.006 and IPC materials or services availability level X2 (2,107)=9.982, p=0.007. And factors that predicted hand hygiene were: Years of experience in occupation (β=0.372. p=0.040) and IPC knowledge score (β=0.306. p=0.001).
Keywords
Knowledge • Hand hygiene • Infection • Prevention • Control • Tamale • Ghana
Introduction
Competent Infection Prevention and Control (IPC) methods such as hand hygiene are elementary necessities for all healthcare providers and the general public to reduce the morbidity and mortality associated with nosocomial infections or Hospital Acquired Infections (HAI). The most efficient, easiest, and least-cost method of infection prevention and control is hand hygiene etiquette in our healthcare environment [1]. Although hand hygiene practice is a good way to prevention of infection in our healthcare settings, studies have revealed that, on average, healthcare providers do not practice hand hygiene half the number of times they are expected and this has contributed to HAI increase [2].
According to World health organisation guidelines on hand hygiene in healthcare, there are five moments of hand hygiene and they are: before touching a patient, before a clean or aseptic procedure, after body fluid exposure risk, after touching a patient, and after touching patient environment [3]. The contributory factor implicated in nosocomial infections in our healthcare settings is poor IPC practice including hand hygiene among healthcare providers [4]. Nakamura and Tompkins study has revealed that about 5 to 10.0% of all admitted patients develop nosocomial infections and 70.0% of the identified pathogens are resistant to one or more of the antimicrobial medicine currently in use [5].
Sub-Saharan African countries including Ghana records a high prevalence rate of HAI, ranging from 2%-49%; this is particularly high among critically ill patients admitted to the critical intensive unit where the rate is projected to range from 21.2%-35.6%. The prevalence of nosocomial in some African countries such as Burkina Faso, Mali, Gabon, Uganda, Cameroon varies between 1.6% to 28.7%, for instance, the prevalence of nosocomial infections in Ghana is reported to be 6.7% [6]. A survey by Labi et al., in Ghana, reported a national prevalence rate of 8.2% and that of Tamale Teaching Hospital (TTH) to be 8.0% the survey further identified surgical site infection to be the leading nosocomial infection nationwide [7].
In Apanga et al. study, they recommended institutional-based such as work practices of healthcare providers to evaluate or identify other factors accounting for the increased nosocomial infection in the surgical department of TTH [8]. This encouraged this study to assess the practice of WHO's five moments of hand hygiene among nurses at the surgical department of Tamale Teaching Hospital.
Materials and Methods
This study was conducted using a descriptive Crosssectional survey to collect data among nurses at the surgical department of Tamale Teaching Hospital using a survey questionnaire.
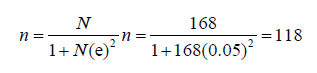
Sampling and sample size determination
The sample size was calculated using the Yamane formula for calculating sample size which is stated below; where n is the sample size, N is the population size, and e is the level of precision. With the acknowledged population of 168 (from the report of 2017 annual performance review), a sample size of 118 was used for this study, and simple random sampling was used in selecting the study respondents.
Method of data analysis
Data entry and analysis were done using Statistical Package for the Social Sciences (SPSS) version 20. Continuous variables were summarized into means and proportions, while categorical variables were summarized into frequencies and percentages and presented using tables and figures. Scores for knowledge on the prevention of nosocomial infection, IPC materials or services availability, and hand hygiene practice were done using a sum score of correct responses from respondents. For the knowledge level, those who scored correctly 6-7 were considered to have good knowledge and those with scores below 5 considered poor knowledge. With IPC materials or service availability level those who scored 0-2 assume to have rated IPC materials or services not always available, scores of 3-5 were considered sometimes available and scores of 6-8 were considered always available. On hand hygiene practice level scores of 4-5 were considered good practice and scores before 4 were considered poor practice. Bivariate analysis was done using chi-square and multivariate analysis was done using multiple regression models at a significance level of 95%.
Ethical consideration
Approval to conduct this research in the hospital was gained from the research department of the hospital after reviewing the proposal and tool for data collection. Respondents’ consented to participate in the study and they were made to know that they had the right to skip any question they feel uncomfortable answering and can draw from participating at any time they will. Confidentiality was assured and any form of harm avoid. All materials used for this study were duly referenced.
Results
Demographic Characteristics
A total of 118 questionnaires were administered of which 107 were satisfactorily filled and returned. The majority (60.7%) of the respondents were males and the mean age of the respondents was 32.21 ± 6.48 with minimum and maximum ages of 21 and 58 respectively. The majority (57.9%) of them were within the age group of 30 years-39 years. The mean years of occupational and departmental experience were 6.48 ± 5.39 and 3.16 ± 3.15 respectively. The majority (73.8%) of the years of experience in terms of their occupation was less than 10 years (Table 1).
Table 1: Demographic characteristics of the respondents’.
| Characteristics of the respondents’ | Frequency (n=107) | Percentage (%) | |
|---|---|---|---|
| Sex of respondents | Male | 65 | 60.70% |
| Female | 42 | 39.30% | |
| Age of respondents' in years | 20-29 | 36 | 33.60% |
| 30-39 | 62 | 57.90% | |
| 40-49 | 5 | 4.70% | |
| 50-59 | 4 | 3.70% | |
| Marital status | Married | 75 | 70.10% |
| Single | 32 | 29.90% | |
| Years of occupational experience | Less than 10 years | 79 | 73.80% |
| 10 years and above | 28 | 26.20% | |
| Years of departmental experience | Less than 10 years | 101 | 94.40% |
| 10 years and above | 6 | 5.60% | |
Knowledge of nosocomial infection prevention
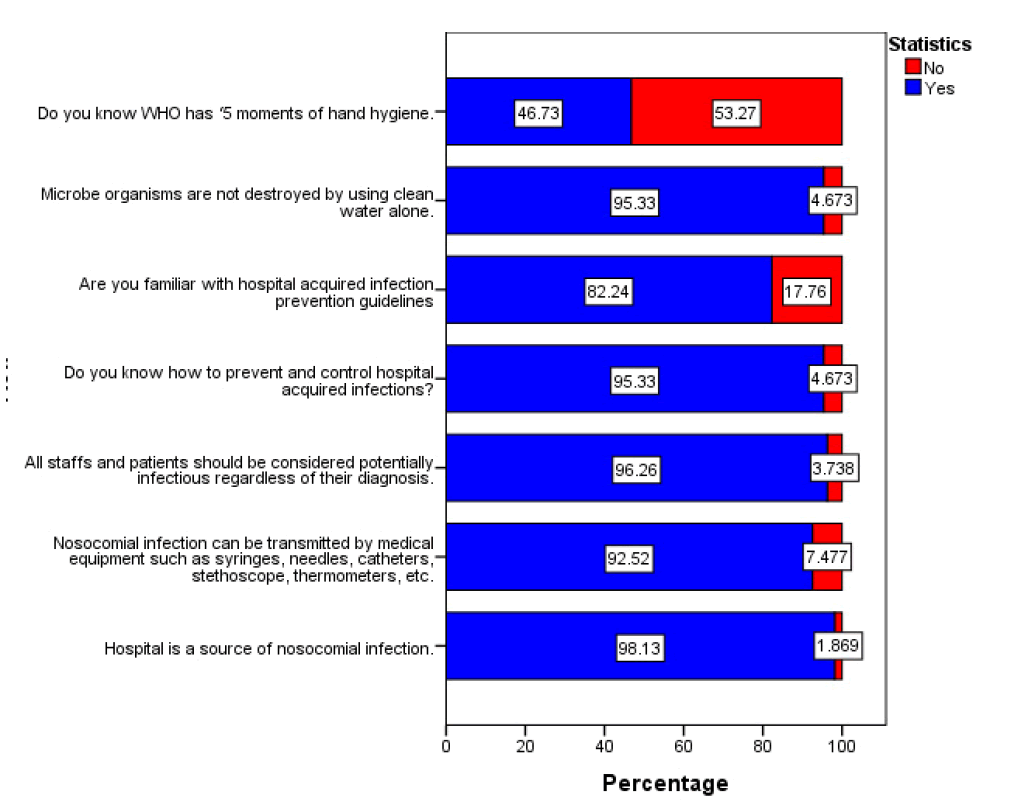
The majority (98.1%) of the respondents knew that the hospital is a source of nosocomial infection and also majority (96.3%) knew that all staffs and patients regardless of their diagnosis are potential sources of nosocomial infection. Meanwhile, with knowledge on WHO, five moments of hand hygiene only (46.7%) of the respondents knew about it in Figure 1. The respondents' mean knowledge on prevention of nosocomial infection was 6.07 ± 1.00 with minimum and maximum scores of 0 and 7 respectively. The majority (82.2%) of the respondents had good knowledge concerning nosocomial infection prevention.
Figure 1: Respondents’ knowledge of nosocomial infection prevention
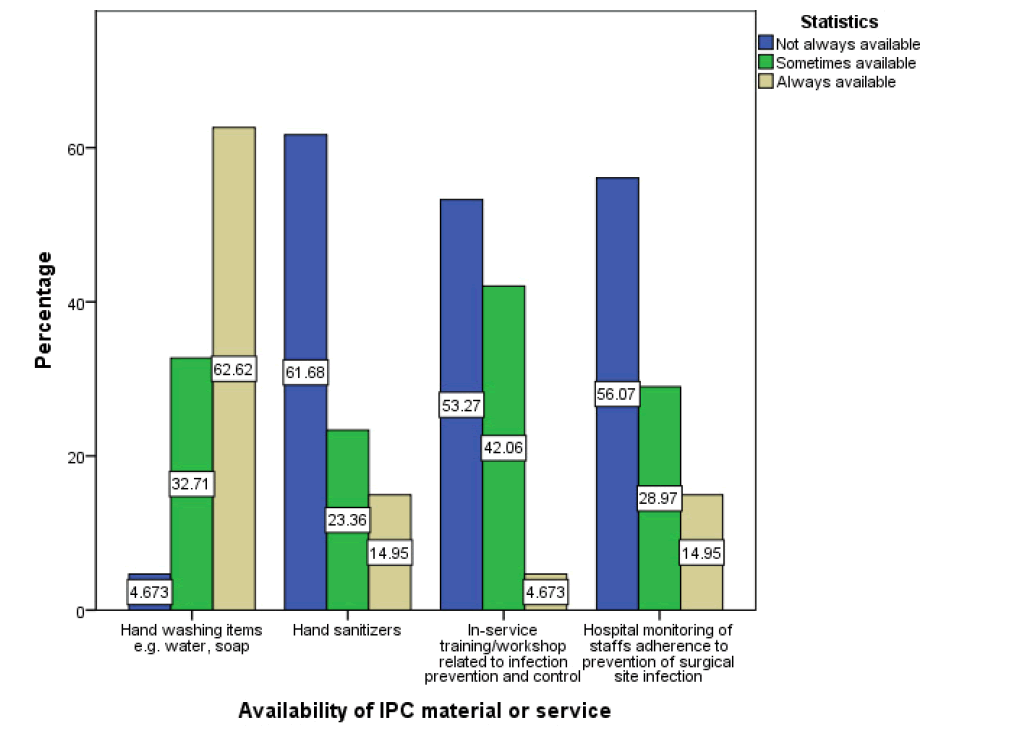
IPC materials or service availability
On hand washing materials such as water and soap most (62.6%) of the respondents indicated they were always available and 32.7% indicated they were sometimes available and only 4.7% indicate they were not always available. Hand sanitizers were not always available according to 61.7% of the respondents. Hospital services to staff towards the prevention of nosocomial in terms of training or workshops on IPC were not always available according to 53.3% of the respondents in Figure 2. According to 10.3% of the respondents, on the whole, IPC materials or services were always available to them, while about 50.5% of the respondents indicated that IPC materials or services were sometimes available to them and the remaining indicated not always availability.
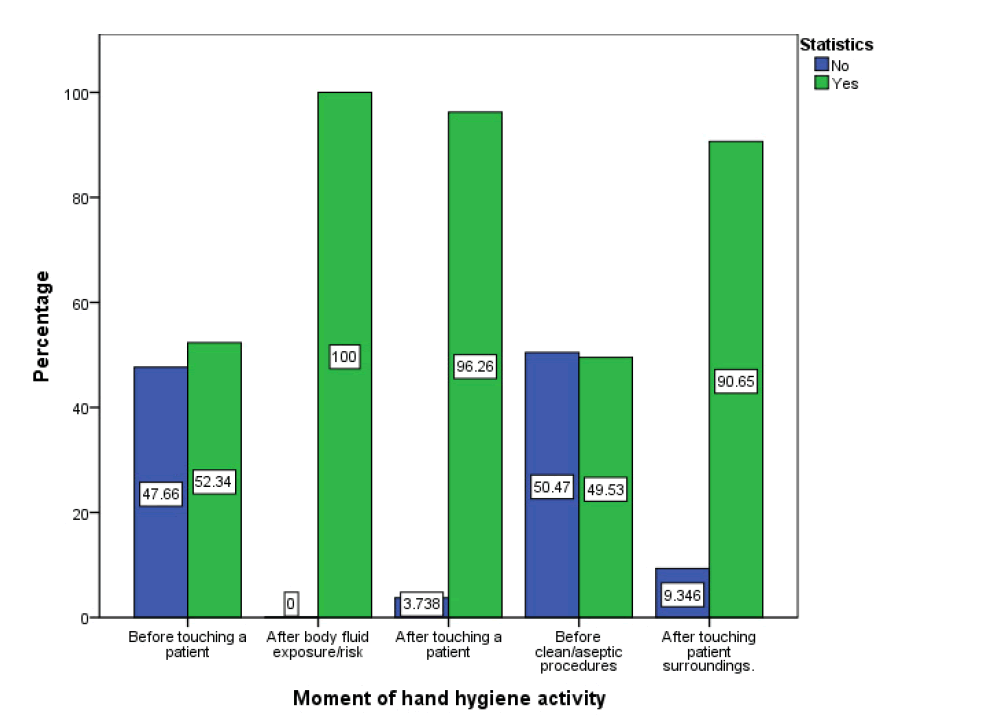
The practice of WHO five moments of hand hygiene
All the respondents indicated hand hygiene practice after body fluid exposure and the majority (96.3%) indicated hand hygiene practice after touching a patient. Also, more (90.7%) of the respondents practiced hand hygiene after touch the patient's surroundings. Meanwhile, the practice was less (50.5%) before the clean or aseptic procedure and 47.7% of respondents indicate no practice before touching a patient (Figure 3). Overall WHO fivemoment hand hygiene practice level was good among 64.5% of the respondents.
Association between factors and practice level of WHO five moments of hand hygiene
Factors significantly associated with hand hygiene practice were age group of respondents X2(2, 107)=201, p=0.006 and IPC materials or services availability level X2(2, 107)=9.982, p=0.007. However, the remaining factors were not significantly associated with the WHO's five moments of hand hygiene practice (P>0.5) (Table 2).
Table 2: Chi-square association between factors and hand hygiene practice.
| Respondents’ | Hand hygiene practice level | ||||
|---|---|---|---|---|---|
| Good practice | Poor practice | X2 | p-value | ||
| Sex of respondents | Male | 43 | 22 | 0.201 | 0.654 |
| Female | 26 | 16 | |||
| Age groups | 20-29 | 27 | 9 | 10.127 | 0.006 |
| 30-39 | 33 | 29 | |||
| 40-59 | 9 | 0 | |||
| Marital Status | Married | 48 | 27 | 0.026 | 0.872 |
| Single | 21 | 11 | |||
| Years of occupational experience | Less than 10 years | 48 | 31 | 1.831 | 0.176 |
| 10 years and above | 21 | 7 | |||
| Years of departmental experience | Less than 10 years | 64 | 37 | 0.986 | 0.321 |
| 10 years and above | 5 | 1 | |||
| Knowledge level | Good | 59 | 29 | 1.418 | 0.234 |
| Poor | 10 | 9 | |||
| IPC material or service availability level | Always available | 10 | 1 | 9.982 | 0.007 |
| Sometimes available | 39 | 15 | |||
| Not always available | 20 | 22 | |||
Predictors of WHO five moments of hand hygiene practice
Multiple regression was run to predict WHO's five moments of hand hygiene practice score from age, years of experience in the occupation, years of experience in the surgical department, IPC materials or services availability score, and IPC knowledge score. These variables (years of experience in occupation and IPC knowledge score) statistically significantly predicted WHO five moments of hand hygiene practice, F (5,101)=18.637, p<0.005, R2=0.175. Only years of experience in occupation and IPC knowledge score added statistically significantly to the prediction, p<0.05. Years of experience in occupation had the highest prediction (β=0.372, p=0.040) than IPC knowledge score (β=0.306. p=0.001) (Table 3).
Table 3: Multiple regression analysis for predictors of WHO five moments of hand hygiene practice.
| Model | Unstandardized Coefficients | Standardized Coefficients | 95.0% Confidence Interval for B | ||||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | t | Sig. | Lower | Upper | |
| (Constant) | 2.309 | 0.911 | 2.533 | 0.013 | 0.501 | 4.116 | |
| Age of respondents in years | -0.027 | 0.027 | -0.17 | -1.021 | 0.31 | -0.081 | 0.026 |
| Years of experience in the occupation | 0.069 | 0.033 | 0.372 | 2.076 | 0.04 | 0.003 | 0.135 |
| Years of experience in the surgical department | -0.007 | 0.038 | -0.023 | -0.198 | 0.844 | -0.083 | 0.068 |
| IPC materials or services availability score | 0.057 | 0.056 | 0.098 | 1.026 | 0.308 | -0.053 | 0.167 |
| IPC knowledge score | 0.306 | 0.094 | 0.306 | 3.265 | 0.001 | 0.12 | 0.492 |
Discussion
The study found the respondents to be young with a mean age of 32.21 ± 6.48 years, and most (65.4%) being males. Again, the majority (60.7%) were married. This differs from two previous studies conducted in Ghana where most of the participants were females [9,10]. For instance, a study by Hayeh, at the La General Hospital in Accra found 71.4% of their study population to be females [10]. The mean years of occupational work experience of respondents were 6.48 ± 5.39 years. However, the great majority (94.4%) had worked for less than 10 years in the surgical department, this is in line with other previous publications [9, 10].
Nosocomial infection prevention knowledge was good among the majority (82.2%) of the respondents and this differs as compared to other studies in Ghana and other West African Countries, [9, 11, 12]. A study in Ghana LA General hospital recorded higher-good IPC knowledge among 97.0% of the respondents [9], but similar to this study finding is Cawich et al, study finding where 81% of staff knew infection control [13]. However, a study in a Tertiary Referral Center in North-Western Nigeria, reported an overall median knowledge of 70.0% [11].
According to 98.1%, of the respondents in this current study, the main source of nosocomial infection is in the hospital. They also agreed that all staff and patients should be considered potentially infectious regardless of their diagnosis and 95.3% of the respondents knew how to prevent and control hospital-acquired infections, this is in line with Stubblefield's work [14]. The majority (92.5%) agreed nosocomial infection can be transmitted by medical equipment such as syringes, needles, catheters, stethoscopes, and thermometers, and that microbe organism are not destroyed by using clean water alone. This supports a study by Al-Khalidi, that nosocomial infections are acquired during healthcare delivery from patients or healthcare staff or through contaminated equipment, instruments, hands, bed linen, or air droplets [15].
Less than average (46.7%) of the respondents knew about the WHO ‘5 moments of hand hygiene, meanwhile the five moments of hand hygiene by WHO is a proven tested approach, which is reasonable and user-friendly for hand hygiene in all healthcare settings that all healthcare must know [3].
In this current study at the TTH, the majority (62.62%) of the respondents’ hand washing items such as water and soap were always available. This is very good since hand hygiene compliance will be positive relative to the availability of IPC materials. This is high as compared to a similar study in La General Hospital, which indicated (31.4%) availability of IPC materials (soap, water, and towel) for healthcare care workers to comply with IPC [9]. According to WHO, 2004 practical guidelines on infection control in healthcare facilities, the role of providing IPC materials in a healthcare facility is on the administrators of the healthcare facilities [16]. The problem of healthcare worker exposure to blood-borne pathogens like HIV and hepatitis B while caring for patients is on increase in both developed and developing countries due to inadequate IPC resources [17].
Hand hygiene after touching patient contacts was reported practiced by 96.3% of the respondents and this is in line with the study result of Alice et al., where 3.9% of the respondents reported never hand hygiene practice after patient contact and this practice is in line with the recommendation from WHO and CDC [2,3,18]. Most (90.7%) of the respondents reported hand hygiene after contact with patient surrounding and this is low as compared to a study by Abdulraheem et al., [19]. Meanwhile, only 52.3% of the respondents reported hand hygiene before patient contact, this is not good compare to 96.3% hand hygiene after patient contact and opposite to Abdulraheem et al., which reported 97% of the respondents’ did wash their hands before or after taking care of patients [19]. Hand hygiene before a clean or aseptic procedure was poorly practiced by 50.5% of the respondents, this is low as compare to Alice et al., a study that reported 57.5% practice and this is against WHO recommendation on hand hygiene [3].
On overall hand hygiene practice according to WHO five moments of hand hygiene, about 64.5% of the respondents had good practice level. This is almost in line with Randle et al., observational study on hand hygiene adherence following the introduction of an education intervention [20]. Randle et al found that educational program on hand hygiene is a good predictor of hand hygiene practice among healthcare workers. There was an increased adherence to hand hygiene practice from the baseline of 53.0% post educational intervention to 67.7% for point 2 observation and 70.8% for point 3 observation [20]. However, this will be reported low as compared to 87.5% performance from Sharif et al., study [21].
Factors significantly associated with WHO's five hand hygiene practices were age group of respondents (p=0.006), and this is not the same in another study which reported no significant association between age group and compliance to hand hygiene, p-value >0.05 [22].
IPC materials or services availability level was significantly associated with WHO's five hand hygiene practices (p=0.007). This was in line with earlier studies by Engdaw et al., Randle et al., and Alhassan et al., where availability of training or education on hand hygiene had a positive influence on hand hygiene practice [20,23-26]. Respondents' years of occupational experience was identified as a major positive predictor of hand hygiene practice, meaning an increase in year occupational experience will increase hand hygiene practice and also respondents IPC knowledge was identified as a positive predictor of hand hygiene practice among respondents and this reported in a similar study [24].
This study's limitation is the use of self-reports to collect data on the practice of hand hygiene among the respondents. Even though self-reporting is the easiest method to gather data, bias can be introduced as respondents may report better practice than their real practice.
Conclusion
More than half the nurses self-report good practice of hand hygiene, more than eighty percent selfreported good knowledge with regards to the prevention of nosocomial infection, and IPC materials or service was mostly not available. Factors associated with hand hygiene practice were the age of the respondents and the availability of IPC materials and services. IPC knowledge and years of occupational experience predicted hand hygiene practice.
Data Availability
All data relating to the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
There is no conflict of interest with this submission.
Funding Statement
Funding for this study was completed by the author without any external funding.
Acknowledgment
The authors would like to thank the management and research department of TTH. Also, we would like to thank all the staff of the surgical department of TTH for their cooperation.
References
- Mathur P. Hand hygiene: Back to the basics of infection control. Indian J Med Res. 134(5):611-620 (2011).
- CDC. CDC Features. Centers for Disease Control and Prevention. (2018).
- WHO. WHO guidelines on hand hygiene in health care: first global patient safety challenge clean care is safer care. Geneva: World Health Organisation. (2009).
- Jain M, Dogra V, Mishra B, et al. Infection control practices among doctors and nurses in a tertiary care hospital. Ann Trop Med Public Health. 5(1):29-33 (2012).
- Nakamura RK, Tompkins E. Nosocomial infection. Compend Contin Educ Vet. 34(4):1-10 (2012).
- Mbim EN, Mboto CI, Agbo BE. A review of nosocomial infections in sub-saharan. Br Microbiol Res J. 15(1):1-11 (2016).
- Alhassan AR. Nurses hand hygiene compliance: An observational study in tamale teaching hospital, Ghana. 6(2):28-34. (2020)
- Apanga S, Adda J, Issahaku M, et al. Post Operative Surgical Site Infection in a Surgical Ward of a Tertiary Care Hospital in Northern Ghana. Int J Res Health Sci.2(1): 207-212 (2014).
- Kondor VD. Health worker compliance with infection prevention and control policy in ghana: A case study of la general hospital. Texila Int J Public Health.9(2):1-37 (2018).
- Hayeh PA. Infection prevention and control practices among health workers at ridge regional hospital. Accra: University of Ghana. (2012).
- Iliyasu G, Dayyab F, Habib ZG, et al. Knowledge and practices of infection control among healthcare workers in a tertiary referral center in north-western Nigeria. Ann Afr Med.15(1):34-40 (2016).
- Sha A. Knowledge attitude and practice towards infection control measures amongst healthcare workers in a medical teaching hospital of Calicut District, Kerala, India. Antimicrob Resist Infect Control. 4(1):270 (2015).
- Cawich SO, Tennant IA, McGaw CD, et al. Infection control practice in the operating room: Staff adherence to existing policies in a developing country. Perm J. 17(3):114-118 (2013).
- KhanHA, Ahmad A, Mehboob R. Nosocomial infections and their control strategies. Asian Pac J Trop Biomed. 5(7):509-514 (2015).
- Inweregbu K. Nosocomial infection. 5(1):14-17 (2005).
- WHO. Practical Guidelines for Infection Control in Healthcare Facilities. WHO. (2004).
- Ojulong J, Mitonga K, Lipinge S. Knowledge and attitudes of infection prevention and control among health sciences students at the University of Namibia. Afr Health Sci.13(4):1071-1078 (2013).
- Alice TE, Akhere AD, Ikponwonsa O, et al. Knowledge and practice of infection control among health workers in a tertiary hospital in Edo State, Nigeria. Direct Res J Health Pharm. 1(2):20-27 (2013).
- Abdulraheem I, Amodu M, Saka M, et al. Knowledge, Awareness, and Compliance with Standard Precautions among Health Workers in North-Eastern Nigeria. J Community Med Health Edu. 2(3):1-5 (2012).
- Randle J, Arthur A, Vaughan N, et al. An observational study of hand hygiene adherence following the introduction of an education intervention. J Infect Prev. 15(4):142-147 (2014).
- Sharif A, Arbabisarjou A, Balouchi A, et al. Knowledge, Attitude, and Performance of Nurses toward Hand Hygiene in Hospitals. Glob J Health Sci.8(8):57- 65 (2016).
- Ho S, Ho C, Hng S, et al. Nurses compliance to hand hygiene practice and knowledge at Klang Valley hospital. Clin Ter. 164(5):407-411 (2013).
- Engdaw GT. Gebrehiwot M. and Andualem Z. Hand hygiene compliance and associated factors among health care providers in central Gonder zone public primary hospitals, Northwest Ethiopia. Antimicrob Resist Infect Control. 8(190):1-7 (2019).
- Cruz JP, Bashtawi MA. Predictors of hand hygiene practice among Saudi nursing students: Across-sectional self-reported study. J. Infect. Public Health.9(4):485-493 (2016).
- Alhassan AR. Kuugbee E, Der E. Surgical healthcare providers’ compliance to hand hygiene and facemask use: A case of tamale teaching hospital, Ghana. J Prev Infec Contr. 6(4):51 (2020).
- Alhassan AR. Nurses Hand Hygiene Compliance: An Observational Study in Tamale Teaching Hospital, Ghana. ARC J Nurs Healthc. 6(2):28-34 (2020).