Research Article - Clinical Investigation (2022) Volume 12, Issue 9
Refractive outcomes of phacoaspiration in paediatric cataract : a retrospective cohort study
- Corresponding Author:
- Dr. Sana Parveen
Department of Otorhinolaryngology, Jawahar Lal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, Maharashtra, India
E-mail: sanaparveen23@yahoo.com
Received: 03-Aug-2022, Manuscript No. FMCI-22-71111; Editor assigned: 06-Aug-2022, PreQC No. FMCI-22-71111 (PQ); Reviewed: 20-Aug-2022, QC No. FMCI-22-71111 (Q); Revised: 04-Sep-2022, Manuscript No. FMCI-22-71111 (R); Published: 28-Sep-2022; DOI: 10.37532/2041-6792.2022.12(9).175-180
Abstract
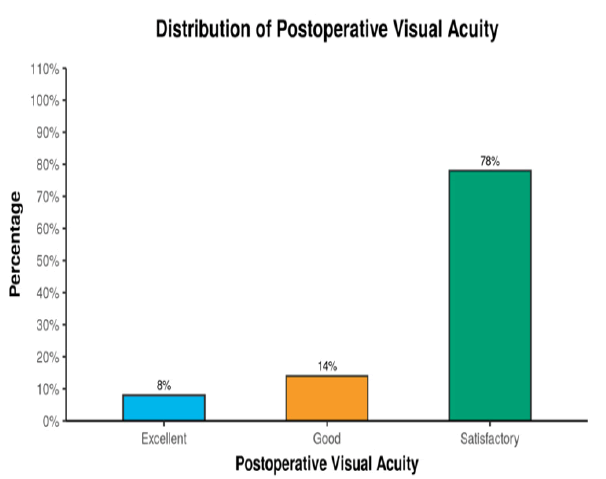
Background: Cataract is the mechanism of opacification of the lens of the eye, which is mostly seen in adults as a result of old age, associated comorbid conditions and systemic diseases. Globally, around 70 million blind- person-years are due to childhood blindness, out of which around 14%, i.e. 10 million blind-person-years are because of childhood cataract3. India has a huge burden of approximately 280,000–320,000 children with impaired vision, which leads to loss of millions of dollars. Hence we conducted a hospital based retrospective study on the presentation patterns, visual impairment and surgical outcomes of patients suffering from pediatric cataract in central India. Aim: To determine safety and visual outcomes for pediatric cataract done under RBSK in Ratan Jyoti Netralaya Ophthalmic Institute and Research Centre Gwalior (M.P.). Objective: To determine safety and visual outcomes for pediatric cataract done under RBSK at an Ophthalmic Research Institute in developing country. Methods: This retrospective cohort study was conducted was conducted on patients diagnosed with congenital and developmental cataract under the age of 18 years presenting to the hospital and undergoing phacoaspiration surgery at xxx institute in Central India. For each patient, the Best Corrected Visual Acuity (BCVA) using snellen’s Chart and age at presentation was assessed. Clinical presentation, management and surgical outcomes were recorded. Results: The postoperative vision of 50 eyes was analyzed (Figure 2). 4 (8%) eyes had vision >6/12 (excellent), 7 (14%) eyes had vision between 6/24 and 6/12 (good), 39 (78%) of the eyes had vision between 6/60 and 6/36 (satisfactory). Conclusions: Our study revealed that cataract extraction with IOLs implantation done with anterior vitrectomy+ primary posterior capsulotomy is the procedure of choice for management of pediatric cataract. Cataracts associated with anterior segment abnormalities have a poor postoperative outcome. Early diagnosis and prompt surgical intervention are extremely important in the management of pediatric cataract, as also adequate visual rehabilitation in the form of spectacles with both distance and near correction.
Keywords
Paediatric • Cataract • childhood • blindness • India
Introduction
Cataract is the mechanism of opacification of the lens of the eye, which is mostly seen in adults as a result of old age, associated comorbid conditions and systemic diseases [1]. At present, the most important cause of treatable childhood blindness is paediatric cataracts. The World Health Organization’s (WHO) initiative for the global elimination of blindness has targeted avoidable causes and has given utmost priority to childhood blindness [2]. It is extremely necessary to identify and manage cataracts in children because they can lead to tremendous economic, emotional and social burdens to the family, child, and society. Most of these cases are diagnosed on routine screening in OPDs, whereas some are diagnosed after parents noticed strabismus or leukocoria [3].
Globally, around 70 million blind-person-years are due to childhood blindness, out of which around 14%, i.e. 10 million blind-person-years are because of childhood cataract3. India has a huge burden of approximately 280,000–320,000 children with impaired vision, which leads to the loss of millions of dollars [4].
Therefore, a thorough understanding of the critical period of the development of vision is extremely crucial to initiate early diagnosis and treatment within the first 3 months of life, which can even be as early as the first 6 weeks from birth.
Hence we conducted a hospital-based retrospective study on the presentation patterns, visual impairment and surgical outcomes of patients suffering from pediatric cataracts in central India.
Materials and Methods
The target population enrolled were children below 18 years of age operated at the hospital from 2016 to February 2020. Informed consent was obtained from the parents of all patients participating in the study and it has been approved by the institutional Ethics Committee of the institute.
This retrospective cohort study was conducted on patients diagnosed with congenital and developmental cataracts under the age of 18 years presenting to the hospital and undergoing phacoaspiration surgery at xxx institute in Central India. For each patient, the Best Corrected Visual Acuity (BCVA) using Snellen's Chart and age at presentation was assessed. Clinical presentation, management and surgical outcomes were recorded.
Inclusion criteria
• All congenital and developmental cataract patients identified under RBSK undergoing surgery at RJN below 18 years of age.
• Minimum follow-up of 3 months duration.
Exclusion criteria
•Traumatic cataract
• Steroid-induced cataract
•Patients having retinal disorders and (ROP babies requiring treatment)
Statistical Analysis
Data were entered into SPSS Software. The analysis was done in SPSS version 16.0 in the windows operating system. Measures of descriptive analysis namely percentage, mean and standard deviation were utilised to depict the clinical parameters in the research Pro-forma. All statistical tests were examined with a 5% level of significance of P ≤ 0.05.
Outcome Measures
Visual acuity postoperatively and on follows for a minimum of up to 3 months was the main method of measuring the outcome of surgery, along with the status of the other eye and the development of any squint has to be ruled out.
The parameters assessed at follow-up were Best corrected visual acuity, Intra-Ocular Pressure, complications preoperatively and postoperatively and other notable findings if any.
Results
The study included 50 eyes and 33 cataracts from January 2016 to February 2020. 34 eyes of 17 patients had bilateral cataracts and 16 eyes of 16 patients had a cataract in a single eye.
The follow-up days were postop day 1, day 7 and 5-6 weeks after surgery. Residual ametropia was corrected with occlusion therapy and spectacle correction, which was initiated soon after surgery. A typical occlusion therapy regimen for infants lasted 6 to 8 hrs every day and for late-onset, it was done for 2 to 6 hours a day in single-eye cataracts, with adjustment according to the degree of amblyopia in cases with cataracts in both eyes. Table 1 shows the distribution of patients according to age.
Table 1: Age-wise distribution of patients
| Age Group (yrs) | Number (%) |
|---|---|
| <2 | 5 (15.1) |
| 2-10 | 16 (48.4) |
| >10 | 16 (48.4) |
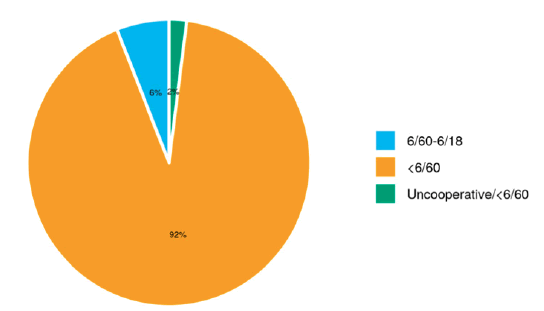
Preoperative visual acuity was recorded by Snellen's chart and fixation pattern. 46 (92%) of the eyes had vision less than 6/60 (which is defined as visual acuity less than 6/60 or poor fixation), 3(6%)of the eyes had vision 6/60-6/18, while in one (2%) eye visual acuity cannot be recorded as the child was uncooperative (uncooperative/<6/60)(Table 2). In the greatest proportion of cases, nearly 92 % had a preoperative visual acuity <6/60 (Figure 1).
Table 2: Distribution of the participants in terms of preoperative visual acuity (n=50)
| Preoperative Visual Acuity | Frequency | Percentage |
|---|---|---|
| 6/60-6/18 | 3 | 6.00% |
| <6/60 | 46 | 92.00% |
| Uncooperative/<6/60 | 1 | 2.00% |
| Total | 50 | 100.00% |
Out of the 50 eyes, 4 (8%) eyes were left aphakic in 2 children with bilateral congenital cataracts less than 1 year of age. The postoperative vision of 50 eyes was analyzed (Figure 2). 4 (8%) eyes had vision >6/12 (excellent), 7 (14%) eyes had vision between 6/24 and 6/12 (good), 39 (78%) of the eyes had vision between 6/60 and 6/36 (satisfactory) (Table 3)
Table 3: Association between postoperative visual acuity and IOL implantation (n=50).
| IOL Implantation | Postoperative Visual Acuity | Fisher's Exact Test | ||||
|---|---|---|---|---|---|---|
| Excellent (>6/12) | Good (6/24- 6/12) | Satisfactory (6/60-6/36) | Total | X^2 | P Value | |
| Yes | 4 (8.7%) | 7 (15.2%) | 35 (76.1%) | 46 (100.0%) | 1.226 | 1 |
| No | 0 (0.0%) | 0 (0.0%) | 4 (100.0%) | 4 (100.0%) | ||
| Total | 4 (8.0%) | 7 (14.0%) | 39 (78.0%) | 50 (100.0%) |
The follow-up duration with postoperative visual acuity(>6/12) ranged from 11 days–473 days. The follow-up duration with postoperative visual acuity(6/24-6/12) ranged from 1 day–413 days. The follow-up duration with postoperative visual acuity(6/60-6/36) ranged from 1 day–238 days (Table 4) (Figure 3).
Table 4: Comparison of the 3 subgroups of the variable postoperative visual acuity in terms of follow-up duration (Days)(n=50)
| Follow-up duration (Days) | Postoperative visual acuity | Kruskal Wallis test | |||
|---|---|---|---|---|---|
| Excellent (>6/12) | Good (6/36-6/24) | Satisfactory (6//60-6/36) | X^2 | p-value | |
| Mean (SD) | 154.25 (215.37) | 164.86 (165.59) | 57.77 (61.27) | 2.693 | 0.26 |
| Median (IQR) | 66.5 (31.25-189.5) | 107 (39.5-277) | 34 (18.5-75) | ||
| Range | 11–473 | 1-413 | 1-238 |
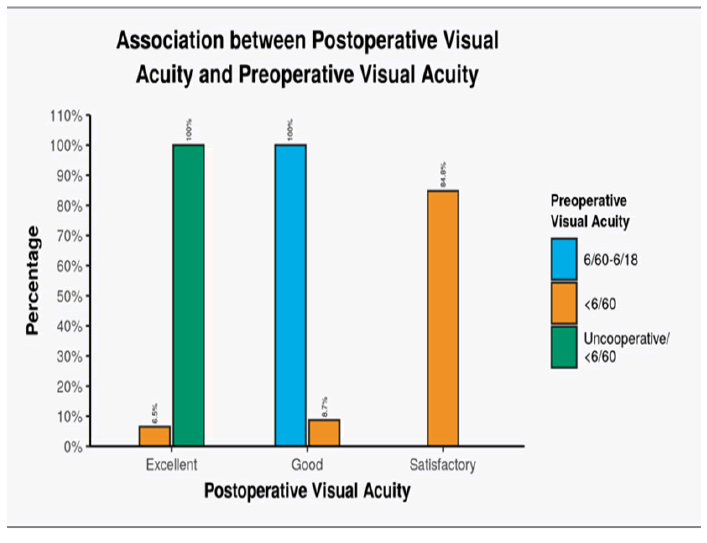
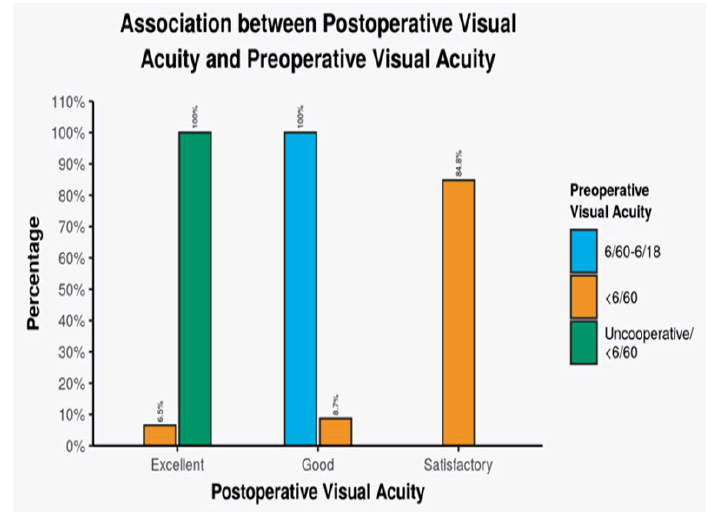
Out of 46 (92%) eyes with preoperative visual acuity <6/60, 3(6.5%) eyes had postoperative visual acuity >6/12 (excellent), 4 (8.7%) eyes had visual acuity 6/24-6/12(good) and 39(84.8%) eyes had visual acuity 6/60- 6/36 (satisfactory).
3(6%) eyes with preoperative visual acuity 6/60-6/18 had postoperative visual acuity 6/24-6/12(good). 1 (2%) eye with preoperative visual acuity uncooperative/<6/60 had postoperative visual acuity >6/12(excellent) (Figure 4).
There was a significant difference between various groups concerning the distribution of visual acuity in the postoperative period (X^2=31.250, p≤0.001) (Table 5).
Table 5: Association between postoperative visual acuity and preoperative visual acuity (n=50)
| Preoperative Visual Acuity (=50) | Postoperative Visual Acuity | Fisher's exact test | ||||
|---|---|---|---|---|---|---|
| Excellent (>6/12) | Good (6/36-6/24) | Satisfactory (6/60-6/36) | Total | X^2 | P Value | |
| 6/60-6/18(n=3) | 0(0.0%) | 3(100.0%) | 0(0.0%) | 3(100.0%) | 31.25 | <0.001 |
| <6/60(n=46) | 3(6.5%) | 4(8.7%) | 39(84.8%) | 46(100.0%) | ||
| Uncooperative/<6/60(n=1) | 1 (100.0%) | 0(0.0%) | 0(0.0%) | 1(100.0%) | ||
| Total | 4(8.0%) | 7(14.0%) | 39(78.0%) | 50(100.0%) |
Eyes with preoperative visual acuity: 6/60-6/18 had the largest proportion of postoperative visual acuity 6/24-6/12(Good). Eyes with preoperative visual acuity <6/60 had the largest proportion of postoperative visual acuity 6/60-6/36 (Satisfactory)
Discussion
According to the World Health Organization (WHO), every minute, a child goes blind somewhere in the world2. In 1992 they estimated that there are around 15 lakh children with SVI or severe visual impairment in the world. The prevalence of childhood cataracts is approximately 1 to15 per 10,000 children.
In our study, 50 eyes of 33 patients with cataracts were evaluated concerning the laterality, age at the time of surgery and follow-up duration. It is difficult to compare our study with others because of the difficulty in recording visual acuity in the paediatric age group due to non-cooperation. The imprecision of this acuity assessment is a limitation of our study. It is suggested that younger children may have better results because they may have had less delay between the onset of cataract and surgical treatment, or that they may have worse results because of the onset of cataract at a younger age [5]. The limitations of our data prevent us from definitively resolving this issue. The mean age at surgery was 7.74 years, this is similar to the findings in the study done in Ethiopia (mean of 7.9 years) and other studies in low/middle-income countries [6-8]. However, the age at surgery in our study was higher than a report from developed countries [3]. A study from Kenya also showed a younger age at surgery compared with our study [9]. The age of our patients varied from 4 months to 17 years.
Our study included an almost equal number of males and females. There are 17 male children and 16 female children, there is no gender disparity in our study. However, a study done by Gogate et al included significantly more males (18) than females (8) [10]. They attributed the reason to less access to eye care facilities for females in India. A study conducted in Nepal by Chaudhary S et an in 2017 found male: female ratio of 1.3:1, 57% were males [l1]. Sex had no correlation with visual outcome (p=0.286). Though there is no evidence that the incidence of childhood cataract is more in males, more males were brought for surgery. This may be because the parents concern for their sons which is common in many parts of developing world including India. Thus pointing towards a gender bias in these two studies as compared to our study
Our study did not show significant correlation with postoperative final visual outcome in relation to IOL implantation or aphakia (P=1.000), this may be because of early correction of aphakia with glasses in aphakic cases and amblyopia therapy. This is consistent with the study done by Chaudhary S et a in Nepal which did not show any significant correlation with postoperative final visual outcome in relation to IOL implantation or aphakia (p=0.129) [l1].
In a study done by Shah MA et al (2012), Bowman et al12 (2007), and Hochstrasser et al13(1994) has shown that insertion of IOL resulted in significant improvement in visual outcome [l1-13]. A study done by Khanna RC et al in south India reported postoperative visual acuity of >6/18 in 39.5% of the patient , Ghodke A et al conducted a study on pediatric cataract in July 2017 and on assessment of visual acuity with Snellen’s chart, 17 eyes (36.2%) had best corrected visual acuity better than 6/18 after cataract extraction at last visit i.e. at 6 months [5]. Gogate et al14 reported 42.2% having best corrected visual acuity (BCVA) >6/18. Postoperatively there was a significant improvement in visual acuity [14].
Management of pediatric cataract poses an important problem with respect to changing refraction, technical aspects of surgery as well as functional outcome [15]. The timing of surgery is crucial for successful optical restoration and good postoperative outcome, especially in case of children [16]. Strict follow up and adequate rehabilitation are necessary for good results. In order to address blindness due to cataract, counselling of parents with active case finding combined with and clear referral pathways are extremely important [17]. Surgery must be undertaken by a paediatric ophthalmologist in a fully equipped unit, with trained and supportive staff. Multiple strategies are most likely to be required to improve follow-up after surgery [18-20].
Conclusions
Our study revealed that cataract extraction with IOLs implantation done with anterior vitrectomy+ primary posterior capsulotomy is the procedure of choice for the management of pediatric cataract. Cataracts associated with anterior segment abnormalities have a poor postoperative outcome. Early diagnosis and prompt surgical intervention are extremely important in the management of pediatric cataract, as also adequate visual rehabilitation in the form of spectacles with both distance and near correction.
Source of funding
No funding from any Institution or Organization.
References
- Chaudhary S, Lavaju P, Govinda B, et al. Factors affecting the visual outcome of pediatric cataract surgery: A hospital based prospective study in eastern Nepal. Nepal J Ophthalmol. 9(2):143-148(2017).
- World Health Organization. Prevention of childhood blindness. World Health Organ. 1992. [google scholar] [Crossref]
- Khokhar SK . Pediatric cataract. Indian J Ophthalmol. 65(12):1340(2017).
- Chak M , Wade A, Rahi JS. Long-term visual acuity and its predictors after surgery for congenital cataract: Findings of the British congenital cataract study. Investig Ophthalmol Vis Sci.47(10):4262-4269(2006).
- Ghodke A, Ingole A, Rathod S, et al. Review Of Surgical Outcomes In Pediatric Cataract. Int J Contemp Med Res. 4(7):1591-1594(2017).
- Asferaw M. Outcome of paediatric cataract surgery in Northwest Ethiopia: A retrospective case series. Br J Ophthalmol. 103(1):112-118(2019).
- Bowman RJ, Kabiru J, Negretti G, et al. Outcomes of bilateral cataract surgery in Tanzanian children. Ophthalmol. 114(12):2287-2292(2007).
- Umar MM, Abubakar A, Achi I, et al. Pediatric cataract surgery in National Eye Centre Kaduna, Nigeria: Outcome and challenges. Middle East Afr J Ophthalmol. 22(1):92(2015).
- Khanna RC, Foster A, Krishnaiah S, et al. Visual outcomes of bilateral congenital and developmental cataracts in young children in south India and causes of poor outcome. Indian J Ophthalmol. 61(2):65(2013).
- Bhattacharje H, Das K, Borah R, et al. Causes of childhood blindness in the northeastern states of India. Indian J Ophthalmol. 56(6):495(2008).
- Yorston D, Wood M, Foster A. Results of cataract surgery in young children in East Africa. Br J Ophthalmol.85:267-271 (2001).
- Gogate PM, Sahasrabudhe M, Shah M, et al. Long term outcomes of bilateral congenital and developmental cataracts operated in Maharashtra, India. Miraj pediatric cataract study III. Indian J Ophthalmol. 62:186-195 (2014).
- Shah MA, Shah SM, Shikhangi KA, et al. Factors affecting visual outcome following surgical treatment of cataracts in children. Open J Ophthalmo. 2:131-139 (2012).
- Bowman RJC, Kabiru J, Negretti G, et al. Outcomes of bilateral cataract surgery in tanzanian children. Ophthalmology.114:2287- 2292 (2007).
- Hochstrasser P, Gloor B. Surgical results of uni- and bilateral congenital and traumatic cataract in infancy to adolescence. Klin Monbl Augenheilkd. 204:274-278 (1994).
- Gogate P, Patil S, Kulkarni A, et al. Barriers to follow-up for pediatric cataract surgery in Maharashtra,India: How regular follow- up is important for good outcome. The miraj pediatric cataract study II. Indian J Ophthalmol. 62:327-332 (2014).
- Panahi-Bazaz MR, Zamani M, Abazar B. Hydrophilic acrylic versus PMMA intraocular lens implantation in pediatric cataract surgery. J Ophthalmic Vis Res. 4(4):201 (2009).
- Singh A, Kumar R, Mishra C, et al. Moving from survival to healthy survival through child health screening and early intervention services under Rashtriya Bal Swasthya Karyakram (RBSK). Indian J pediatr. 82(11):1012-1018 (2015).
- Foster A, Gilbert C, Rahi J. Epidemiology of cataract in childhood: A global perspective. J Cataract Refract Surg. 23:601-604 (1997).
- Sudarshan AP. Infantile cataracts. Surv Ophthalmol. 40(6):427-458 (1996).