Review Article - Clinical Practice (2016) Volume 13, Issue 2
Improved intensive patient prognosis by earlier activation of rapid response teams and timely response
- Corresponding Author:
- Sergio Castaño-Ávila
Servicio Medicina Intensiva del Hospital Universitario Araba
Sede Santiago Olaguibel 29, Vitoria, C.P. 01004, Spain
E-mail: sergio.castanoavila@osakidetza.net
Abstract
Background: The prognosis of hospitalised patients requiring ICU admission depends on the time since onset of clinical deterioration. The objective of this study was to assess differences between hospital-ward patients admitted to the intensive care unit (ICU) with persistent clinical deterioration measured by a patient at risk (PR) score and those admitted at an earlier stage of deterioration. Methods: Retrospective analysis was conducted of patients admitted to the ICU from hospital wards between January and July 2013. During this period, a protocol was in place to assess the PR on hospital wards. We gathered data on demographic characteristics, clinical risk scores, PAR scores and trigger criteria. A delayed alert was defined as a PAR score >2, or ≥2 warning signs in systemic blood pressure or peripheral pulse oximetry saturation assessments between 8 and 24 h before ICU admission. Delayed alerts and other variables were compared using Student’s t, Mann Whitney U or X2 tests, as appropriate, with p<0.05 considered significant. Results: During the study, there were 80 admissions of 69 patients (Mean age: 67.91 years, standard deviation: 13.85). Alerts were most frequently circulatory (33.7%) or respiratory (30%) related, and made by physicians on duty (85.2%). In the 33 delayed alerts, patients had higher APACHE II and SAPS II scores and incidence of multiple organ dysfunction syndrome (MODS), and tended to have longer ICU admission; while other variables were similar. Conclusions: Patients admitted to the ICU after late assessment of their clinical status using a PR score have higher APACHE and SAPS scores and MODS rate and possibly longer ICU stays. Scoring systems may promote timely assessment and treatment on hospital wards.
Keywords
Critical care, critical illness, scoring systems, rapid responsesystem, vital signs
Introduction
Medical practice is based on knowledge, judgement and the recognition of patterns in illnesses, and focuses on determining the risk illnesses pose to patients and deciding on their management in terms of treatment. A consensus conference on the identification of atrisk patients [1] concluded that all hospitalised patients should have their vital signs monitored, as aberrations in these are predictive of lifethreatening conditions. The importance of monitoring for outcomes has mainly started to be documented from the introduction of early warning systems [1-4] and patient at risk (PR) scores that include vital signs, mental status [5] and subjective assessment of clinical status by clinicians [6]. Traditionally, physicians are alerted to the need to assess the severity of patients on the basis of the deviation of clinical parameters and blood test results from normal. Multidisciplinary rapid response teams (RRTs) are usually coordinated by intensive care units [2] (ICUs) and aim to achieve early assessment of at-risk patients on hospital wards, before their condition deteriorates significantly [1-3], to enable the timely and proportionate interventions and thereby improve outcomes [4,7]. Establishment of such teams is one of six strategies recommended by the Institute for Healthcare Improvement [8] to reduce in-hospital mortality, but their effectiveness is still unclear [9-12], given the high heterogeneity between studies, with study populations and activation protocols that are difficult to compare [5].
It is recognised, however, that the prognosis of hospitalised patients who require ICU admission depends on the time since the onset of clinical deterioration, outcomes being better in those admitted at an early stage of deterioration. Timely detection of patient deterioration [13,14] on the ward based on clinical alerts, and the introduction of protocols for rapid assessment of patients by RRTs (Their nurse and doctor, together with an intensivist), may improve outcomes. Such teams may be especially useful in surgical units [5], guiding decision making for complex patients, providing objective assessment tools, and facilitating continuity of care after patient discharge from ICUs [2,9].
The objective of this study was to assess differences in severity and outcome between patients admitted to the ICU in early stages of deterioration and those admitted after persistent clinical deterioration measured using a PR score.
Material and Methods
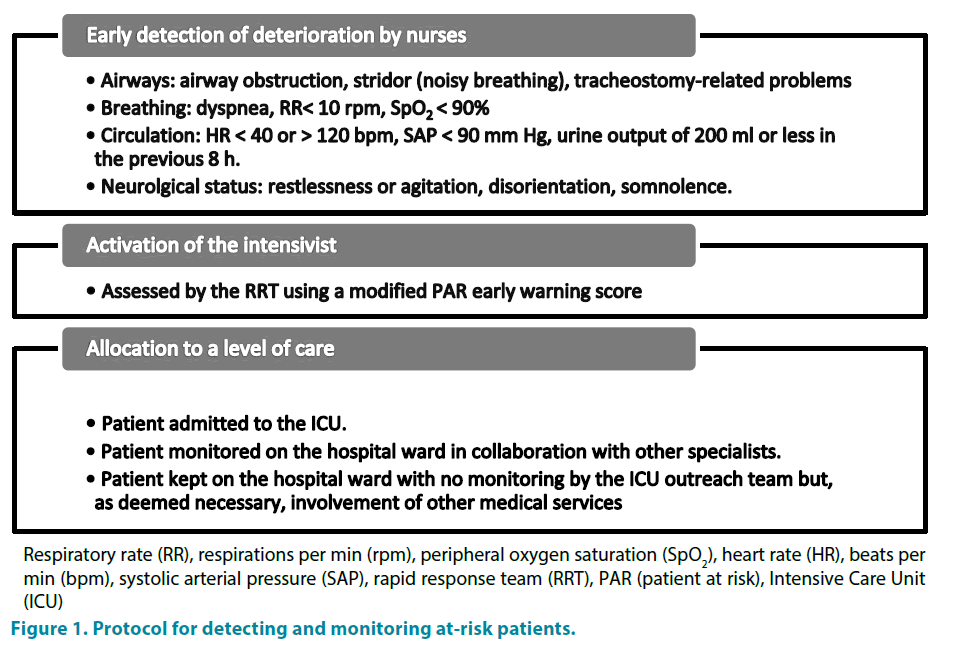
We conducted a retrospective descriptive study between 1 January and 30 June 2013 of all admissions from hospital wards to our ICU. It is a multipurpose unit with 13 beds for criticallyill patients and 4 for semi-critical patients, in a tertiary hospital with 280 beds. Throughout the study period, a protocol was in place across the hospital for detecting and monitoring atrisk patients: This protocol is multidisciplinary in nature, involving nursing staff, the attending doctor and intensivist on duty in the different steps summarised in FIGURE 1.
Respiratory rate (RR), respirations per min (rpm), peripheral oxygen saturation (SpO2), heart rate (HR), beats per min (bpm), systolic arterial pressure (SAP), rapid response team (RRT), PAR (patient at risk), Intensive Care Unit (ICU)
Figure 1: Protocol for detecting and monitoring at-risk patients.
Early detection of deterioration: Monitoring by nurses on the hospital ward for clinical warning signs. If any of these abnormalities are observed, the nurse in charge decides whether assessment is needed by the ward doctor in charge of the patient, who the person responsible for contacting the ICU doctor on duty if deemed necessary (though if the ward doctor is unavailable, this may be done by the head nurse of the ward). Calls to an intensivist triggered in the traditional way were recorded as a function of the reason for the alert and the person who detected the crisis, and care was provided in a similar way.
Some patients discharged from the ICU, namely, those considered to be at particularly high risk of clinical deterioration (e.g., with warning signs or highly-complex conditions, or after prolonged admission), are followed-up by an ICU outreach team and which facilitates continuity of care and collaboration in clinical decision making.
Activation of the intensivist followed by a rapid response (within minutes) involving anamnesis, physical examination and complementary tests, as deemed appropriate. The patient is assessed by the RRT using a modified PR early warning score [5] (TABLE 1). Decision making about admission of a patient to the ICU is guided by this score, but the final decision is left to the intensivist who visits and assesses the patient.
| Variable | Score | 3 | 2 | 1 | 0 | 1 | 2 | 3 |
| SBP | <80 | 80-90 | 90-180 | 181-200 | >200 | |||
| PR | <40 | 40-45 | 45-120 | 121-140 | >140 | |||
| RR | <9 | 9-18 | 19-25 | 26-30 | >30 | |||
| Tª | <35 | 35-38.5 | >38.5 | |||||
| NRL | disorientation | O3 | O1-2 | |||||
| SpO2 | <85b | 85-89a | 90-95 | >95 | ||||
| Diuresis 8h | 0 | < 200 | > 200 | |||||
• bFor patients with no chronic respiratory disease counts for 4 points
• O3: response to voice
• O2: response to pain
• O1: No response
SBP: systolic blood pressure (mm Hg). PR: Pulse rate (beats per min). RR: Respiratory rate (respirations per min). Ta: Temperature. NRL: Neurological status
SpO2: Peripheral oxygen saturation. Diuresis 8 h: Urine output in the previous 8 h. O: Eye response
Table 1: Patient at risk warning scale.
Allocation to a level of care by the RRT, with the following options: Patient admitted to the ICU, or patient monitored on the hospital ward in collaboration with other specialists (principally from the internal medicine unit), who act as liaison doctors, for decision making and treatment changes, with reassessment of the PR scor e [5] and need for ICU admission at least once every 24 h, or Patient kept on the hospital ward with no monitoring by the ICU outreach team but, as deemed necessary, involvement of other medical services (mainly those of internal medicine, nephrology and psychiatry). When decisions concern the limitation of life support, patients are referred for palliative care, when the palliative care unit is operational, and otherwise, a comfort care plan is agreed between the ICU and ward staff.
Decisions regarding the level of care are reviewable, depending on clinical changes in patients during their hospital stay. In the event of cardiorespiratory arrest, the process for calling for emergency help is independent of the protocol described above; the ICU is contacted directly and responds immediately providing advanced life support.
We collected data on the following: Patient demographic characteristics; diagnosis; severity scores during the first 24 h after admission (Acute Physiology and Chronic Health Evaluation II [APACHE II] [15] and Simplified Acute Physiology II Score [SAPS II]) [16]; previous comorbidity (Defined as the presence of two or more of the following conditions: hypertension, diabetes mellitus, chronic renal failure, ischaemic cardiomyopathy, heart failure, or chronic obstructive pulmonary disease); criteria for detecting deterioration (Airway, breathing, circulatory or neurological warning signs, or subjective assessment of the attending doctor or nurse), person who triggered the alert, ward of origin, modified PR score [5] on ICU admission, presence of multiple organ dysfunction syndrome (MODS) and maximum score on the sepsis-related organ failure assessment (SOFA) [17], length of stay in the ICU (in days) and death. We recorded whether patients met criteria indicating a delayed alert, namely, whether they had a PR score of over 2, or showed 2 or more of the aforementioned warning signs in the assessment of SAP or oxygen saturation using pulse oximetry at any point from 8 to 24 h prior to ICU admission.
• Data analysis
Statistical analysis was carried out using IBM SPSS Statistics for Windows, Version 21 (IBM SPSS, Armonk, NY, USA). Qualitative data are expressed as frequency and continuous data as mean ± standard deviation (SD) or median (P50) and range, depending their distribution. Comparisons between patients who did and did not meet criteria indicating a delayed alert were made using the Fisher’s exact, chisquare, Student’s t or Mann Whitney U tests as appropriate given the nature of the data, considering p<0.05 to be statistical significant.
The study was conducted in accordance with the ethical standards for handling of patient data and medical records required by the clinical trials and research committee of our hospital.
Results
We analysed a total of 80 consecutive admissions of 69 patients (55.1% male), with a mean age of 67.91 years old (SD 13.85), and of these, 42% had multimorbidity. The general characteristics of these 80 admissions to the ICU during the study period are summarised in TABLE 2.
| Variable | Total admissions 80 |
Delayedalertgroup 33 |
Rest of theadmissions 47 |
P value |
|---|---|---|---|---|
| n men: n women | 39:41 | 18:15 | 21:26 | 0.38 |
| Age m | 68.73 (SD 13.56) | 71.70 (SD 13.39) | 65.64 (SD 13.42) | 0.1 |
| Multimorbidity n | 50 (62.5%) | 22 (66,6%) | 28 (59,57%) | 0.51 |
| APACHE II score m | 16.15 (SD 7.1) | 19.33 (SD 7.33) | 13.91 (SD 6.07) | 0.001 |
| SAPS II score m | 41.13 (SD 17.82), | 47 (SD 21.49) | 37 (SD 13.48) | 0.01 |
| MODS score m | 25 (31.3%) | 18 (54,54%) | 7 (14,89%) | <0.0001 |
| SOFAmáx m | 10.6 (SD 4.34) | 10.39 (SD 4.59) | 11.14 (SD 3.93) | 0.7 |
| EPAR score at admission m | 3.26 (SD 2.45) | 4.09 (SD 2.54) | 2.68 (SD 2.23) | 0.53 |
| ICU stay (m days) | 6.91 (SD 8.66) | 9.15 (SD 8.67) | 5.34 (SD 8.39) | 0.052 |
| Death n | 10 (12.5%) | 6 (18,18%) | 4 (8,5%) | 0.3 |
APACHE II score: Acute Physiology and Chronic Health Evaluation II. SAPS II score: Simplified Acute Physiology II Score. MODS: multiple organ dysfunction syndrome. SOFA: maximum score on de sepsis-related organ failure assessment.
Table 2: General characteristics of admissions to the ICU.
The results concerning alert criteria were: Admission to the ICU was triggered by circulatory, respiratory, and neurological warning signs respectively in 27, 24 and 17 patients, by findings during monitoring following discharge from the unit in 8, by the subjective assessment of a ward doctor or nurse in 3 and by airway warning signs in 1. Among all these admissions, the alert prompting a call to the ICU was classified as delayed in 33 cases (41.25%): Patients had a modified PR [5] score of more than 2 in 21 cases, and showed 2 or more warning signs in relation to oxygen saturation in 12 cases. Overall, this delayed alert group had higher severity scores on APACHE II [15] and SAPS II [16] and a higher incidence of MODS, differences compared to the rest of the sample being statistically significant. Specifically, the incidence of MODS was 1.75 higher (95% CI: 1.22 to 2.50) and the relative risk of death was 2.14 higher (95% CI 0.65-6.98) in the delayed alert group than the other patients [17]. Their ICU stay was longer, but the difference did not reach statistical significance. Out of the 80 admissions, 34 were transfers from surgical units, 50% of these being classified as delayed alerts, compared to 34.78% of those from medical units (p=0.172).
There were 10 deaths (12.5%), all of them during ICU admission, 9 following the withdrawal of life support.
Discussion
We present a study analysing differences in outcome in patients from hospital wards requiring ICU admission as a function of the timeliness of the detection of their clinical deterioration and assessment by an RRT. Our main findings are that patients with high PR scores on hospital wards are in a more severe clinical condition and have poorer MODS, than those who are transferred rapidly at the beginning of their clinical deterioration; they may also have longer ICU stays.
• Detection of at-risk patients
Care activity for patients under the care of intensivists seeks to achieve early detection of severe and potentially severe patients, and to allow timely initiation of treatment, thereby avoiding deterioration in patient status and reducing mortality rates and costs [18,19]. In line with this, there have been campaigns to promote new approaches for managing sepsis, acute myocardial infarction, cerebrovascular accident, and polytrauma and, in recent years, at-risk patients on the hospital ward [19]. Although there is little evidence to help us identify the best way to assess patients to predict deterioration [1], early alert systems have been developed based on changes in vital signs1 and/ or blood test results (hyperlactatemia, acidemia, hypo- or hyperkalaemia, elevated troponin levels, thrombocytopenia, hypercapnia) [3-20]; these provide warning signs for ward staff and may be used to justify requests for assessment by a RRT. Developed as multidisciplinary teams closely linked to intensive medicine [5-19], RRTs have two main lines of action: Follow-up of selected patients discharged from the ICU, and support in the identification and treatment of patients on hospital wards with significant clinical deterioration [21], to avoid delayed ICU admission, and reduce cardiac arrest rates [11-22], unplanned ICU admissions [14-22], the severity of patients admitted to the ICU from wards [13,14,22] and in-hospital mortality [10].
Our protocol for detecting high-risk patients on the ward uses alert criteria that are well documented in the literature [1,14,20,23-29], combining clinical parameters based on the assessment of vital signs, including monitoring of respiratory function, neurological status, and diuresis, and the subjective assessment of the attending clinicians. Various authors [14,20,25-29] have established more specific alert criteria: SpO2<90% with 10 L per minute of supplemental oxygen; SpO2<90% with oxygen therapy; ventilation with a mask with a fraction of inspired oxygen >50%, SAP>180 or >200 mm Hg; HR<45, >125, 130, or 140 bpm; RR<5, 6, or 8 rpm, or tachypnoea above 24, 28, 30 or >36 rpm; the Glasgow coma score decreasing by more than 2 points, or falling below 13; repeated seizures; uncontrollable pain; difficulty speaking; suspected stroke or acute myocardial infarction; and urine output <50 mL in 4 h. Differences in criteria seem to be related to the hospital setting, and it is plausible that it is considered necessary to use more specific thresholds for alert criteria in large hospitals, to decrease the number of RRT activations, even though this may mean that patients assessed have a higher severity. Our data are obtained from a 280-bed tertiary hospital with 17 intensive care beds. We have opted for more sensitive criteria that may trigger activation of the RRT to assess patients who are not in fact critically ill [30].
• Assessment of the alert by the RRT: PR scores
Although Etter et al. [30] found an association between the number of alert criteria met, the need for ICU admission, and 60-day survival, most of the scientific literature refers to scales for assessing risk [24,31] in patients on hospital wards with progressive scores according to the degree of deviation from normal of the vital sign; and some authors propose that the total score can guide decisions on treatment needed and which hospital unit should provide it. In our protocol, we have used a modified version of the PR score of Goldhill et al. [5], developed to predict the need for ICU admission, with an admission rate rising from 14.1 to 44.2% for scores above 2 points.
In the analysis of Smith et al. [25] of nearly 10,000 medical admissions, the area under the receiver operating characteristic (ROC) curve for the Goldhill scale to predict death within 24 h was 0.8, similar to that for another 31 scales assessed. A study published by the same research group 2 years later [32] compared the results of 34 early warning systems applied to data on over 35,000 medical admissions. In that study, the area under the ROC curve for the Goldhill scale was found to be 0.841 (95% CI: 0.832-0.851), very similar to that for ViEWS, the system which yielded the largest area (ROC of 0.888, 95% CI: 0.88 to 0.895), and which used similar criteria and was designed to predict in-hospital mortality in the context of detecting of high-risk patients.
In our protocol, patient management is not determined by the PR score (on assessment by the RRT) alone. On the one hand, some deviations from normal in vital signs can be interpreted as acceptable fluctuations, clinicians deciding that the patient does not need intensive care; and on the other hand, some patients (such as those with acute myocardial infarction) may need ICU support despite obtaining low PR scores. Nevertheless, the sensitivity and specificity of these types of score for predicting early in-hospital mortality [24-32] mean that we should recognise their usefulness in hospital settings and seek to universalise their use.
• RRTs and mortality
Various reviews and meta-analyses [11,25,32-34] have been published assessing the effectiveness of RRTs in reducing inhospital mortality and cardiac arrest rates. These studies reached conclusions that highlighted the potential of such teams but also found differences that can be understood as follows:
a) It is difficult to draw definitive conclusions in these types of meta-analysis, given that demonstrating effectiveness requires long implementation and study periods [12]; and there is also great heterogeneity in the studies included [12,34,35,37], with different detection protocols [19,21,36], assessment scales and target populations [19,21,36]. Reviewing the studies with positive results, we find that the systems concerned usually involve intensivists [24] and a protocol that is used continuously, 24/7 [22].
b) In comparisons between periods with RRTs operating and control periods (historical or contemporaneous controls), there is likely to be statistical contamination, as there are generally crash teams at all times in all hospitals, and these operate in a similar way [12] to RRTs.
c) Some authors link RRTs to higher ICU admission rates [4,26]; and associated mortality rates are higher than among patients admitted via other routes [26]. These trends are probably attributable to differences in clinical profile and treatment decisions between groups and potentially late assessment by the RRT of patients on ward.
The most recently published meta-analysis [34] includes large series from hospital populations in different healthcare settings, and provides evidence of the benefits of RRTs. Our study has not found improvements in terms of in-hospital or in-ICU mortality, which may be attributable to the relatively small sample size and design of the analysis, but the results do suggest that early detection and treatment of patients who require ICU admission decreases the severity of their condition and their risk of MODS. It seems that PR scores for use on hospital wards help objectively assess patient severity. Additionally, they help identify patients whose illness may have a poorer course, inturn, allowing assessment of whether they require ICU admission, and enabling timely treatment.
• Delayed activation of RRTs and outcome
The prevalence of delayed alerts in our study was 41.25%. Other authors have indicated rates of between 20-50% [14,38], these rates depending on hospital characteristics, the sensitivity of the criteria set, and the hospital protocol for activating RRTs, which in turn, affect the rate of delayed alerts to the ICU [38]. Our criteria to define a delayed alert was a PR score of over 2 points, given its predictive usefulness for ICU admission [5], or showing ≥2 warning signs in the assessment of SAP and SpO2 at any point from 8 to 24 h prior to ICU admission, given the high sensitivity of hypoxaemia and hypotension in the detection of critically ill patients. Recently, Boniatti et al. [14] found a higher rate of delayed alerts (More than 8 h after the onset of symptoms) when the criteria used were SAP<90 mm Hg, RR<5 or >36 rpm, or SpO2<90%; the rate of delayed alerts was lower in their study than ours but they used more specific criteria, and this may explain the higher mortality rate in their delayed alert group (61.8 vs. 41.9%, p<0.001), and greater need for ICU admission (63 versus 36.9%, p<0.001) [12]. In our series, the severity and incidence of MODS were significantly higher in patients with delayed alerts who required ICU admission; the relatively small sample size may explain the similar mortality rates and that the difference in length of ICU stay only bordered significance.
The factors underlying delayed alerts are poorly described in the literature. These include cognitive and sociocultural issues [14,39] as well as factors related to the organisation and staffing levels [35-38] that may reduce the likelihood of hospital staff activating the RRT. It has been suggested that delayed alerts may be minimised using multimodal approaches, such as a combination of clinical notes, structured interviews and multidisciplinary teams [39]; and in our opinion, the following aspects are also important: The availability of information and communicating technology to support early detection and alerts [20], and hospital-wide awareness that such protocols improve the safety and quality of care provided to patients on the hospital ward.
• Limitations
The retrospective nature of the data collection may lead to systematic errors and relatively small sample size reduces the statistical power of the analysis. The fact that in our protocol the PR score was calculated by the RRT after its activation and that is not routinely used for all hospitalised patients mean that we are unable to determine its sensitivity, specificity, predictive values or likelihood ratios for predicting the need for ICU admission.
Given the study protocol, we have not analysed differences in outcome as a function of the alert criterion triggering activation of the RRT or the reason for delayed alerts.
The apparent need for longer ICU stays by patients with delayed alerts compared to the rest was not statistically significant, and as noted earlier, this is likely due to the relatively small sample size.
Conclusions
Delays in alerts to the need for assessment by RRTs are common, increasing patient severity on ICU admission and possibly also the length of ICU stay. Further research is needed exploring the reasons to explain such delays, establishing guidelines for improving early detection and treatment of at-risk patients on hospital wards, and assessing the impact of delayed alerts on outcome.
References
- De Vita MA, Smith GB, Adams-Pizarro I et al. Identifying the hospitalised patient in crisis-A consensus conference on the afferent limb of Rapid Response Systems. Resuscitation81(4), 375-382 (2010).
- Holanda MS, Domínguez MJ, Ruiz Oet al.EICS (Extended Intensive Care Service): Looking outside the ICU. Med.Intensiva. 35(6),349-353 (2011).
- Jäderling G, Bell M, Martling CRet al. ICU admittance by a rapid response team versus conventional admittance, characteristics, and outcome. Crit. Care. Med. 41(3),725-731 (2013).
- Morgan RJ, Williams F, Wright MM. An early warning scoring system for detecting developing critical illness. Clin. Intensive. Care. 8, 100 (1997).
- Goldhill R, McNarry A, Mandersloot Get al. A physiologically-based early warning score for ward patients: the association between score and outcome. Anaesthesia 60(6), 547-553 (2005).
- Kellett J. Hospital medicine (part 2): What would improve acute hospital care? Eur. J.Intern. Med. (20),465-469 (2009).
- Calvo E, Mozo MT, Gordo F. Introduction of a management system in Intensive Care Medicine based on the safety of the seriously ill patient during the entire hospitalization process: extended intensive care medicine. Med.Intensiva. 35(6), 354-360 (2011).
- Berwick DM, Calkins DR, McCannon CJet al. The 100.000 lives campaign: setting a goal and a deadline for improving health care quality. JAMA. 295(3), 324-327(2006).
- Abella A, Torrejón I, Enciso Vet al. ICU without walls Project. Effect of the early detection of patients at risk. Med.Intensiva. 37(1), 12-18 (2013)
- Neily J, Mills P, Young Yet al. Association between implementation of a medical team training program and surgical mortality. JAMA. 304(15),1693-1700 (2010).
- Chan P, Jain R, Nallmothu Bet al. Rapid response teams. A systematic review and meta-analysis. Arch. Intern. Med. 170(1),18-26 (2010).
- Chrysochoou G, Gunn SR. Demonstrating the benefit of medical emergency temas (MET) proves more difficult than anticipated. Crit. Care. 10, 306 (2006).
- Cardoso LT, Grion CM, Matsuo T et al. Impact of delayed admission to intensive care units on mortality of critically ill patients: a cohort study. Crit. Care. 15(1) R 28 (2011).
- Boniatti M, Azzolini N, Viana Met al.Delayed medical emergency team calls and associated outcomes. Crit. Care. Med. 42(1),26-30 (2014).
- Knaus WA, Draper EA, Wagner DPet al. APACHE II: a severity of disease classification system. Crit. Care. Med. 13(10), 818-819 (1985).
- Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute phisiology score (SAPS II) based on an European/North American multicenter study. JAMA. 270(24), 2957-2963 (1993).
- Vincent JL, Moren R, Takala Jet al.The SOFA (Sepsis- related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive. Care. Med. 22(7),707-710 (1996).
- Afessa B, Gajic O, Morales IJet al. Association between ICU admission during morning rounds and mortality. Chest. 136 (6),1489-1495 (2009).
- Mozo T, Torrejón I, Gordo F (2015) UCI sin paredes: una realidad posible.
- Socías L, Heras G, Estrada VMet al.Application of Medical Information Systems for the detection of high risk patients: Rapid care alerts. Pilot study of the ARA-Son Llàtzer Project. Med.Intensive. 37(1),19-26 (2013).
- Mc Neill G, Bryden D. Do either early warning systems or emergency response teams improve hospital patient survival? A systematic review. Resuscitation 84(12),1652-67 (2013).
- De Vita MA, Bellomo R, Hillman Ket al. Findings of the first consensus on medical emergency teams. Crit. Care. Med. 34(9), 2463-2478 (2006).
- Richmond R. Rapid Response teams. Health Policy Newsletter(21),2 (2008).
- Al-Qahtani S, Al-Dorzi HM, Tamim HMet al.Impact of an intensivist-led multidisciplinary extendend rapid response team on Hospital-wide cardiopulmonary arrests and mortality. Crit. Care. Med. 41(2), 506-517 (2013).
- Smith GB, Pryterch DR, Schmidt PEet al. Review and performance evaluation of aggregate weighted “track and trigger” systems. Resuscitation 79, 11-21 (2008).
- Karpman C, Keegan MT, Jensen JBet al. The impact of rapid response team on outcome of patients transferred from the ward to the ICU: a single-center study. Crit. Care. Med. 41, 2284-2291 (2013).
- Karvellas C, De Souza I, Gibney Ret al. Association between implementation of an intensivist-led medial emergency team and mortality. BMJ. Qual.Saf. 21, 152-159 (2012).
- Parr MJ, Hadfield JH, Flabouris Aet al. The medical emergency team: 12 month analysis of reasons for activation, inmediate outcome and not-for-resuscitation orders. Resuscitation.50(1), 39-44 (2001).
- Jones D, DeVita M, Bellomo R. Rapid-response teams. N. Engl. J. Med.365, 139-146 (2011).
- Etter R, Ludwig R, Lersch Fet al. Early prognostic value of the medical emergency team calling criteria in patients admitted to intensive care from the emergency department. Crit. Care. Med. 36(3), 775-781 (2008).
- Gao H, Mc Donnell A, Harrison DAet al. Systematic review and evaluation of physiological track and trigger warning systems for identifying at-risk patients on the ward. Intensive. Care. Med. 33(4), 667-679 (2007).
- Prytherch DR, Smith GB, Schmidt PEet al.ViEWS-Towards a national early warning score for detecting adult inpatient deterioration. Resuscitation. 81(8), 932-937 (2010).
- McGaughey J, Alderdice F, Fowler Ret al.Outreach and early warning systems (EWS) for the prevention of intensive care admission and death of critically ill adult patients on general hospital wards. Cochrane. Database. Syst. Rev. 3, CD005529.
- MaharajR, Raffaele I, WendonJ. Rapid response systems: a systematic review and meta-analysis. Crit. Care. 19,254 (2015).
- Chen J, Bellomo R, Flabouris Aet al.The relationship between early emergency team calls and serious adverse events. Crit. Care. Med. 37(1), 148-153 (2009).
- Tibballs J, Kinney S. Reduction of hospital mortality and of preventable cardiac arrest and death on introduction of a pediatric medical emergency team. Pediatr.Crit.Care. Med. 10(3), 306-312 (2009).
- Buist M, Moore G, Bernard Set al.Effects of medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 324(7334), 387-390. (2002).
- Calzavacca P, Licari E, Tee Aet al.The impact of rapid response system on delayed emergency team activation patient characteristics and outcomes- A follow-up study. Resuscitation 81(1),31-35 (2010).
- Marshall S, Kitto S, Shearer Wet al. Why don´t hospital staff actívate the rapid response system (RRS)? How frequently is it needed and can the process be improved? Implement. Sci. 6,39 (2011).