Case Report - International Journal of Clinical Rheumatology (2018) Volume 13, Issue 2
A case series of malignancies: mimics of Rheumatological disorders
- *Corresponding Author:
- Jeet Hemantkumar Patel
Department of Rheumatology
Sir Ganga Ram Hospital
New Delhi, India
E-mail: jeet5patel5@gmail.com
Abstract
Background: Malignancy and Autoimmunity interplay is full of complexities. We here, describe few cases of malignancies presented as mimics of autoimmune disorders. A case of acute myeloid leukaemia had leukocytoclastic vasculitis, positive ANA, positive SS-A, and few clinical features of autoimmune disease and it mimicked UCTD. Second case of signet ring cell type of adenocarcinoma of G.I tract mimicked CTD as it had ANA positivity and ILD. Third case was epitheloid sarcoma which mimicked pyomyositis while fourth case was multiple myeloma presented with leukocytoclastic vasculitis, positive ANA, malar rash and active urinary sediments and it had mimicry of SLE. Malignancies can present as autoimmune diseases or they can mimic flare of Rheumatological diseases. Cancer can present as vasculitides, CTDs, myositis or arthritides. Sometimes, it is difficult to ascertain whether autoimmune disorders have caused cancers or malignancies have caused autoimmune disturbances. ANA can be positive in upto 27% cancer patients. There is clearly increased risk of cancers amongst patients of autoimmune diseases compared to general population. Malignancies including metastasis can also present with true paraneoplastic autoimmune disorders. They usually present later in the course of the disease but sometimes surprise internists with sudden appearance in early course of the disease. High index of suspicion is required to detect malignancies in autoimmune diseases as both have invariably similar presentations. PET scan and tissue diagnosis are amongst the major investigations to treat patients with spectrum of malignancy and autoimmunity.
Introduction
It is not uncommon in day to day Rheumatology practice that patients initially classify for some autoimmune disorders and later surprise the doctor with some varied diagnosis. Here, we describe four such cases in which there were initial possibilities of some autoimmune diseases and finally turned out to be malignancies. A clinician must have a high index of suspicion for malignancies, especially when a patient has a provisional diagnosis of undifferentiated connective tissue disease (UCTD), undifferentiated arthritis, unclassifiable vasculitis, lung dominant CTD (LD-CTD) and unclassifiable autoinflammatory disorder or treatment resistant autoimmune diseases e.g. corticosteroid resistant dermatomyositis or sjögren’s syndrome.
Case 1
A 63 year old lady presented with complaints of chronic low grade fever, fatigue and nonscaly, non-tender, non-discharging, mildly itchy erythematous nodular skin lesions all over body Figure 1. She also had dryness of mouth, polyarthralgia, constitutional symptoms and significant weight loss. Hemogram revealed anaemia (Hb-8.4 g/dl), leukopenia (TLC- 2.4 cells/mm3) and peripheral smear showed moderate anisopoikilocytosis with some schistocytes and acanthocytes. ANA was positive by ELISA (267 U/dl) and ENA revealed SS-A 3+. ESR was 140 mm fall in 1st hour and CRP was 48 mg/L. Screening for major infections including tuberculosis was negative. Serum protein electrophoresis was negative. HRCT chest and CECT abdomen revealed early ILD changes and hepatomegaly respectively. Skin biopsy was suggestive of small vessel leukocytoclastic vasculitis. She was treated outside with corticosteroids and DMARDs for provisional diagnosis of UCTD (on the basis of positive ANA, positive SS-A, cytopenias, ILD, vasculitis in skin biopsy and clinical features). Bone marrow examination showed increase in MPO stain positive myeloblasts, seen as focal clusters as well as interspersed amongst normal hematopoietic elements. It was compatible with acute myeloid leukemia (AML). Tablet Azacytidine was started and patient is currently under follow up of hemato-oncologist.
Case 2
A 70 year old female, a diagnosed case of myelofibrosis with a history of Anti-Tubercular treatment (ATT ) for 8 months for tubercular cervical lymphadenitis presented to us with fatigue, weight loss and chronic dry cough. CECT chest revealed mild ILD changes. ANA was 1:640 positive with homogeneous pattern. She was treated as LD-CTD (ANA+, fatigue, constitutional symptoms and ILD) with low dose steroid and anti-malarial.
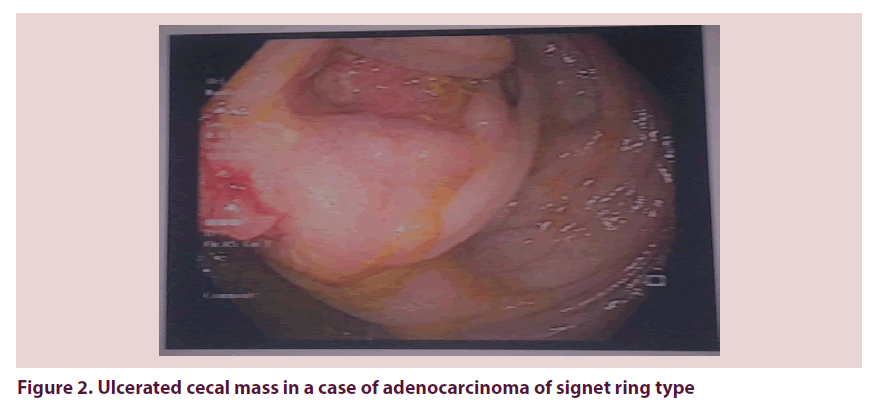
After one month, patient presented with complaints of recurrent vomiting, nausea, increased dry cough and shortness of breath. Hemogram revealed anaemia (Hb-10.9 g/dl), mild leukocytosis (TLC-11300 cells/mm3) and normal platelet count. Abdominal X ray showed distended stomach and X ray Chest showed blunting of costo-phrenic angles with opacities in lower lobes bilaterally. Upper GI endoscopy revealed D1-D2 junction thickening and gastric outlet obstruction. Colonoscopy revealed ulcerated mass in the caecum around the appendicular orifice with ileocecal valve involvement Figure 2. PET CT revealed non- FDG avid diffuse thickening in GE junction with cardia of stomach, D1-D2 and dilation of proximal duodenum and stomach. Pleural fluid examination was positive for malignant cells (signet ring cells +ve) and ascitic fluid also showed few clusters of tumour cells with mesothelial cells Biopsy from ileocecal region and gastric biopsy showed signet ring type of adenocarcinoma. PET CT revealed FDG avid diffuse thickening in Ileocolic junction, mild FDG avid mesenteric lymph nodes and FDG avid mesenteric, omental and peritoneal thickening. Nasojejunal tube was inserted and patient was treated with adequate nutritional support and appropriate fluid management. Chemotherapy was started (Tablet Capecitabine and injection Bivacizumab). ICD was inserted and due to high output in ICD, pleurodesis was done. Palliative care was started. In spite of all possible efforts, patient succumbed to death due to multiorgan dysfunction syndrome. It was a case of poorly differentiated adenocarcinoma of signet ring type involving cecum with secondary gastric spread and malignant pleural effusion, ascites, myelofibrosis and gastric outlet obstruction.
Case 3
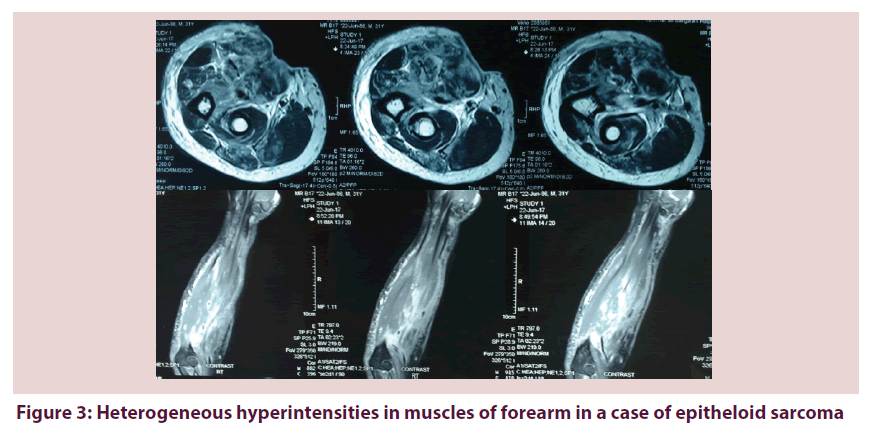
A 31 year old male presented with few pustular lesions around right elbow followed by elbow pain and swelling. He had low grade fever, fatigue and constitutional symptoms without other joint involvement. Swelling progressed from elbow proximally and distally in spite of repeated courses of antibiotics during 3 months duration. ESR, CRP and CPK were elevated. Initial diagnosis of pyomyositis was made although total count was normal. MRI revealed inhomogeneous patchy enhancement in flexor and extensor group of muscles in forearm. Inhomogeneous enhancement was also present in subcutaneous fat planes of forearm. It was consistent with infective myositis and diffuses cellulitis of right forearm Figure 3. He underwent fasciotomy + debridement and biopsy of involved part. Biopsy revealed epitheloid sarcoma. PET CT revealed no metastasis. Right mid-arm amputation was done and patient was well and is under current follow up with oncosurgeon.
Case 4
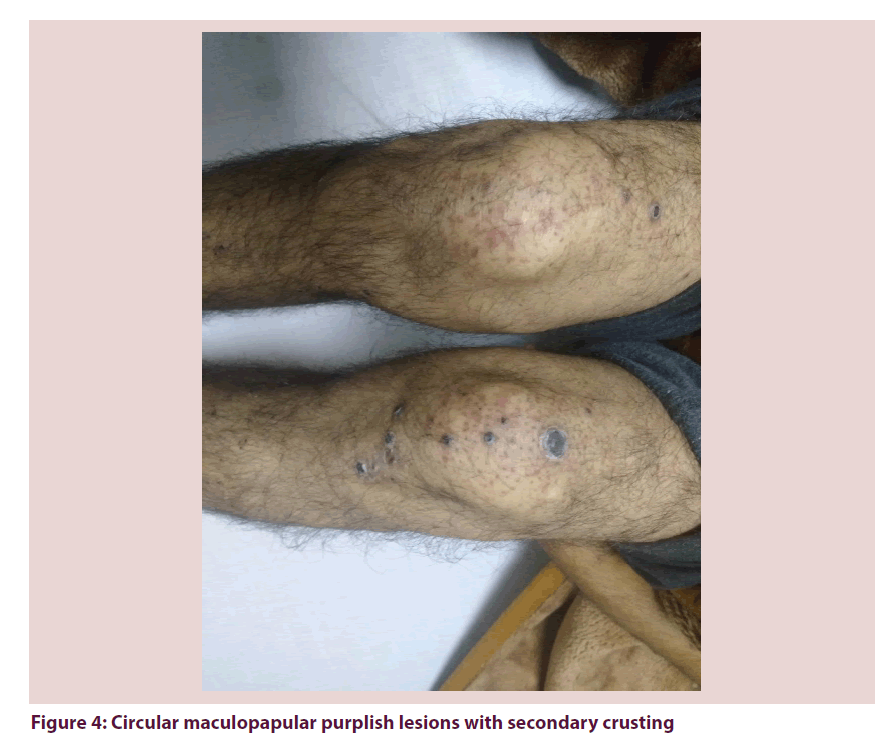
A 53 year old gentleman presented with maculopapular diffuse erythematous mildly itchy skin rash over face. After 1 month, he noticed circular maculopapular purplish itchy lesions with secondary crusting all over body Figure 4. He also had cough, haemoptysis, one episode of epistaxis, tingling/numbness in extremities and significant weight loss. Skin biopsy revealed focal leukocytoclastic vasculitis with no evidence of granuloma or cancer and was consistent with papulonecrotic tuberculid. He was started on ATT. Complete blood count revealed anaemia and kidney function was within normal range. ESR was 145 mm/1st hour. Serum albumin was 2.8 g/dl; serum globulin was 10.0 g/dl with A/G ratio reversal (0.28). Urine microscopy showed presence of 15-20 RBCs, few granular casts and 15-20 WBCs and no proteinuria. Mantoux test and IGRA were negative. ANA was 1:100 positive, direct coomb’s test was 2+ positive and complements were low. Clinical picture along with investigations was suggestive of systemic lupus erythematosus (SLE) (malar rash, vasculitic skin lesions, hematuria, pyuria and casts in urine, positive direct coomb’s test, positive ANA, low complements) or ANCA associated vasculitis. Serum protein electrophoresis, urinary protein electrophoresis and bone marrow biopsy confirmed the diagnosis of multiple myeloma. Chemotherapy was started and he is currently under the care of oncologist. Summary of all above mentioned cases is described in Table 1 with two additional cases.
| Case No. | Malignancies in our patients | Features of autoimmune diseases | Mimic of autoimmune disease | Treatment course |
|---|---|---|---|---|
| 1 | Acute myeloid leukaemia | Positive ANA, positive SS-A, ILD, leukocytoclastic vasculitis, dry mouth, polyarthralgia, fatigue | UCTD | Chemotherapy |
| 2 | Signet ring cell type adenocarcinoma | Positive ANA, ILD, fatigue, constitutional symptoms | LD-CTD | Died |
| 3 | Epitheloid sarcoma | Raised CPK, swelling around right elbow | Pyomyositis | Mid-arm amputation |
| 4 | Multiple myeloma | leukocytoclastic vasculitis, malar rash, positive ANA, positive coomb’s test, low complements, WBCs, RBCs in urine examination, raised acute phase reactants | SLE | chemotherapy |
| 5 | Gall bladder adenocarcinoma with liver metastasis | Raised IgG4 level, raised IgG level, retro-peritoneal fibrosis | IgG4 related diseases | Palliative chemotherapy |
| 6 | Gastro-intestinal stromal tumor of lesser curvature of stomach | Polyarthralgia of small joints of hand, early morning stiffness, tenosynovitis of extensor tendons at wrist | Rheumatoid arthritis | NSAIDS |
Table 1. Summary of malignancy cases mimicking autoimmune diseases
Discussion
Cancers and autoimmune diseases have three different clinical relationships together: increased risk of cancers in rheumatological disorders, rheumatological manifestations of cancers, and lastly, clinical features of cancers mimicking autoimmune diseases. Much has been written for first two scenarios while for third relationship, literature is less in present date.
Autoimmune diseases have defective immune system with inefficient clearing of apoptotic cells, microorganisms and cancer cells. Breach in innate and adaptive immune system leads to increased risk of infections and even cancers in these disorders. There is also increase prevalence of autoantibodies in cancer patient which also points towards a link between cancers and autoimmune diseases. ANA was positive in up to 27% cancer patients in one study and some of them had clinical picture similar to rheumatoid arthritis, SLE, autoimmune myositis, and cutaneous vasculitis etc. There are no known antibodies to ENA or double stranded DNA which points towards difference in autoantigens involvement in cancers and autoimmune diseases [1].
Data of large autoimmune diseases cohort showed increased risk of cancers compared to healthy population (two fold increased risk for SLE and scleroderma etc.). Patients of systemic sclerosis had elevated risks for lung cancer (five fold), liver cancer (three fold), and non-melanoma skin cancer (four fold). GST and PTPN are amongst the few genes which can leads to cancer and are associated with autoimmune disorders [2]. According to Swedish registry; there was also increased risk of 11 different types of gastrointestinal cancers in 33 different autoimmune disorders. Data also showed modification of cancer risk due to use of anti-inflammatory drugs and immunomodulator medications [3].
Thus, it is shown that cancer patients may have high prevalence of autoantibodies and may present with paraneoplastic manifestations as a mimic of autoimmune disorders. On the other hand, autoimmune diseases have higher risk of different types of cancers, especially hematological malignancies and gastrointestinal cancers. Scleroderma, autoimmune myositis, immunosuppressive drugs are all implicated in causation of cancer while sjögren’s syndrome, SLE, sarcoidosis, IgG4 related diseases, Behcet’s disease are amongst other autoimmune disorders which might increase the risk for cancers [4]. There is a very complex interaction between different cytokines, complement system, neuroendocrine system and innate/adaptive immune system in cancer generation and cancer spread in associated autoimmune disorders [5].
Prevalence of hematological malignancies, particularly non-Hodgkin’s Lymphoma (NHL) in autoimmune diseases is around 5%. Relationship between autoimmunity and lymphoproliferative tumors is bi-directional. Risk of NHL is highest in primary sjögren’s syndrome followed by SLE and rheumatoid arthritis. Data on effect of biologic DMARDS on cancer generation is conflicting while use of conventional DMARDS haven’t shown to increase baseline risk of cancer (which is already higher in autoimmune diseases compared to general population) [6]. Sometimes, it is difficult to conclude whether an autoimmune disease has caused cancer or cancer has presented as paraneoplastic autoimmune disorder. Although none of the above described cases were treated with cancer therapies that target immune checkpoints, treatment of cancers with newer drugs e.g. check point inhibitors have opened a new field of autoimmune disorders which also kept in mind while dealing with cancers and autoimmune disorders [7].
Conclusion
Cancers can mimic autoimmune diseases or present with true paraneoplastic autoimmune disorders. They can even present later in the course of the disease or mimic flare of the autoimmune diseases. High index of suspicion is required to detect malignancies in autoimmune diseases as both have similar presentations most of the time. On the same time, thorough investigation (preferably PET CT) including tissue diagnosis is also required in already diagnosed cases of rheumatological disorders to exclude malignancies before giving statement that clinical manifestations are due to disease activity or autoimmunity.
References
- Solans-Laque R, Perez-Bocanegra C, Salud-Salvia A et al. Clinical significance of antinuclear antibodies in malignant diseases: association with rheumatic and connective tissue paraneoplastic syndromes. Lupus. 13, 159–64 (2004).
- Volkers N. Do Autoimmune Diseases Raise The Risk of Cancer? JNCI: J National Cancer Institute. 91(23), 1–1992 (1991).
- Hemminki K, Liu X, Ji J et al. Autoimmune disease and subsequent digestive tract cancer by histology. Annals of Oncology. 10, 1093–333 (2011).
- Giat E, Ehrenfeld M, Shoenfeld Y. Cancer and autoimmune diseases. Autoimmunity Reviews. 16(10), 1049–1057 (2017).
- Kim R, Emi M, Tanabe K. Cancer immunosuppression and autoimmune disease: beyond immunosuppressive networks for tumour immunity. Immunology. 119(2), 254–264 (2006).
- Zintzaras E, Voulgarelis M, Moutsopoulos H. The Risk of Lymphoma Development in Autoimmune Diseases: A Meta-analysis. Arch Intern Med. 165, 2337–2344 (2005).
- Vlist M, Kuball J, Radstake T et al. Immune checkpoints and rheumatic diseases: what can cancer immunotherapy teach us? Nature Reviews Rheumatology. 12, 593–604 (2016).